Despite ongoing rise and fall of new biomarkers of infection, CRP is still widely used and preferred in paediatric practice to detect BI in children. It is one of the most extensively studied sepsis marker. This is a frequently advised test in children presenting with signs and symptoms suggestive of acute infection. It is used as a baseline test to differentiate BI from Non Bacterial Infections (Non BIs) and also to monitor the response to antibiotics [1]. The value of CRP increases within six hours of acute phase response, remain persistently high as long as the inflammation or tissue damage continues and then decreases after a successful treatment [2]. It can be measured quantitatively with a simple method [3]. The rapid decrease of CRP permits the use of this test during the follow up of patients with BIs. However, a great variation in the sensitivity, specificity, and predictive values of this test, has compromised its diagnostic accuracy. Recent evidences state its limited utility as a sole diagnostic marker in children with various infections [4-6]. Therefore, in order to identify children at higher risk of bacterial illnesses, the present study includes laboratory findings, such as WBC and ANC, in addition to CRP.
The aim of this study was to determine the diagnostic performance of CRP alone and its conjunction with WBC and ANC for detection of BI and its differentiation from non bacterial in resource limited settings where other diagnostic markers like procalcitonin is not feasible.
Materials and Methods
This prospective study was conducted in the Department of Paediatrics, Kalinga Institute of Medical Sciences, a tertiary care hospital in Odisha. The inclusion criteria was: Age 1 month to 14 years, history of fever for more than 24 hours and serum CRP testing performed at baseline on admission. Children with immunosuppressive disorders, congenital heart disease, malignancies, chronic diseases and those with prior antibiotic therapy were excluded. A total of 97 consecutive febrile children in whom CRP was advised on admission were studied prospectively. All children attending Outpatient Department (OPD) with a fever of over 100.4°F underwent both a clinical evaluation and relevant blood tests which included complete blood count, blood culture, CRP levels, urine routine/microscopic examination and urine culture.
The study was conducted over a period of four months between August to November 2016. Informed consent was obtained from the parents or legal guardians for blood sampling. The study protocol was approved by the Hospital Ethics Committee.
The data were collected for the following parameters: diagnosis, age, sex, hospitalisation duration, negative/positive cultures (blood, urine, pus, CSF), CRP levels, total WBC count, percentage of neutrophils and ANC. The CRP values of the patients who were admitted to hospital were determined on admission quantitatively by turbidometry. On the basis of their final diagnosis, children were classified into two groups: patients with BI and those without BI. The following children were considered as having BI: 1) bacteraemia-recovery of a single bacterial pathogen in blood culture; 2) urinary tract infection-growth of a single pathogen at ≥105 colony-forming units/mL; 3) lobar pneumonia-chest radiograph showing presence of infiltrate as observed by the radiologist; 4) bacterial meningitis-leucocytosis or positive cerebrospinal fluid culture; 5) bone or joint infections-local isolation of a microorganism; and 6) children at risk of sepsis defined as according to quick Sequential (Sepsis-related) Organ Failure Assessment (qSOFA) score [7].
Statistical Analysis
Continuous normally distributed parameter was reported through Mean (±Standard Deviation). Skewed parameter was reported as median (inter-quartile range). Categorical variable was shown as frequency (percentage). Association between any two categorical variables was assessed through either Chi-square test or Fisher’s-exact test. Independent t-test was applied to assess the significant difference of mean between the two groups for a normally distributed data. Wilcoxon rank sum test is applied for skewed data.
The diagnostic performances of the parameters considered (CRP, WBC, and ANC) were first investigated by area under the Receiver Operating Characteristic (ROC) curve analysis. This technique summarises the validity coefficients of a parameter and provides an overall index of diagnostic accuracy from a plot of sensitivity against the false-positive rate (1-specificity) for all possible cut-off scores. Based on ROC analysis, the best statistical cut-off value for each parameter was calculated and reported. Diagnostic measures such as sensitivity, specificity, positive and negative predictive values along with likelihood ratios for a positive and negative test were also reported. All the statistical analysis was done through the standard statistical software Stata version 13.1. A p-value of <0.05 was considered as statistically significant.
Results
A total of 456 patients were admitted to the paediatric ward during the study period out of which CRP was done as a baseline investigation in 97 patients. Of these, 31 (32%) patients were female. The median age of patients with BI was 4.90±4.14 and those with non BI was 4.72±4.10. BI was diagnosed in 41 children (42%) [Table/Fig-1] and non BI in 56 children. Fourteen patients were admitted to Paediatric Intensive Care Unit (PICU) of which nine had BI and five non BI. In the BI group, 5 had blood culture positive, another 5 patients had urine culture positive, 1 stool culture, 1 pus culture and 1 sputum culture positive.
Clinical characteristics and laboratory findings of bacterial and non-bacterial patients.
| Variable | Bacterial(N=41) | Non-Bacterial(N=56) | p-value |
|---|
| Age (years) Mean±SD | 4.90±4.14 | 4.72±4.10 | 0.828* |
| Gender; n (%) |
| Male | 26 (63.4%) | 40 (71.4%) | 0.403$ |
| Female | 15 (36.6%) | 16 (28.6%) |
| WBC (mm3); Median (range) | 15800 (3330-48100) | 9100 (3400-21500) | <0.001* |
| ANC (mm3); Median (range) | 11760 (1392-41366) | 4834.5 (1155-31900) | <0.001* |
| CRP (mg/L); Median (range) | 3.1 (0.02-32) | 0.4 (0.02-18) | <0.001* |
| Location; n (%) |
| Ward | 32 (78.0%) | 51 (91.1%) | 0.071$ |
| ICU | 9 (22.0%) | 5 (8.9%) |
| Antibiotic, n (%) |
| Received | 41 (100%) | 44 (78.6%) | 0.002$ |
| Not received | 0 (0.0%) | 12 (21.4%) |
*-Based on Wilcoxon Rank Sum Test; $-Based on Chi-square test
Among the 97 children in whom CRP was ordered as baseline investigation, the final diagnosis was pneumonia (14), wheeze associated respiratory tract infection (9), upper respiratory tract infection (5), acute gastroenteritis/dysentery/enteritis (15), bacteraemia (6), urinary tract infection (7), enteric fever (3), febrile convulsion (8), meningitis/encephalitis (7), fever without localising sign (6), viral hepatitis (5) and other miscellaneous infections (12).
In the study group 41 had BI and 56 had non BI. Among the non bacterial group, 3 had hepatitis A IgM positive, 2 had PCR for respiratory viruses positive, 2 had Japanese encephalitis IgM positive and 1 had herpes simplex virus IgM positive.
Demographic characteristics and laboratory findings of patients with and without BI are presented in [Table/Fig-1]. There was no significant difference for age and sex between BI and non BI. CRP, WBC, and ANC were significantly higher in the group of children with BI (p<0.001).
In the current sample data, the statistical cut-off values for detecting BI was 1.2 gm/L (sensitivity, 82.9%; specificity, 75.0%) for CRP, 11400/mm3 (sensitivity, 75.6%; specificity, 73.2%) for WBC, and 6710/mm3 (sensitivity, 75.6%; specificity, 73.2%) for ANC [Table/Fig-2].
Sensitivity, Specificity, Positive Predictive Value (PPV), Negative Predictive Value (NPV).
| Parameter | Cut-offs | AUROC{% (95% CI)} | Sensitivity{% (95% CI)} | Specificity{% (95% CI)} | PPV{% (95% CI)} | NPV{% (95% CI)} | DA{% (95% CI)} | LR+ | LR- |
|---|
| CRP (mg/L) | 1.2 | 81.4 (72.2–90.5) | 82.9 (67.9–92.8) | 75.0 (61.6–85.6) | 70.8 (55.9–83.0) | 85.7 (72.7–94.0) | 78.3 (68.8–86.1) | 3.32 | 0.23 |
| WBC (mm3) | 11400 | 75.9 (65.3–86.5) | 75.6 (59.7–87.6) | 73.2 (59.7–84.2) | 67.4 (52.0–80.5) | 80.4 (66.9–90.2) | 74.2 (64.3–82.6) | 2.82 | 0.33 |
| ANC (mm3) | 6710 | 81.7 (72.5–91.0) | 75.6 (59.7–87.6) | 73.2 (59.7–84.2) | 67.4 (52.0–80.5) | 80.4 (66.9–90.2) | 74.2 (64.3–82.6) | 2.82 | 0.33 |
Diagnostic accuracy, Likelihood Ratio Values of C-Reactive Protein (CRP), White Blood Cell (WBC) and Absolute Neutrophil Count (ANC) for Bacterial Infection Prediction
AUROC– Area Under the Receiver Operating Characteristic curve
LR+ positive Likelihood Ratio, LR- Negative Likelihood Ratio
The PPVs for CRP, WBC and ANC were lesser (70.8%, 67.4% and 67.4% respectively) as compared to the PPVs (85.7%, 80.45 and 80.4% respectively). The overall Diagnostic Accuracy (DA) of these parameters were 78.3%, 74.2%, 74.2% respectively for CRP, WBC and ANC. Likelihood ratio is another way to assess the performance of a diagnostic test. The positive likelihood ratio for all the parameters were observed less than 5 which indicated that minimal increase occurred in the likelihood of disease when these test parameters were positive. Similarly the negative likelihood ratios between 0.2 to 0.5 indicated minimal decrease in the likelihood of disease when the test parameters were negative [Table/Fig-2].
Also, diagnostic performance of CRP in conjunction to WBC and ANC is shown through [Table/Fig-3]. Detailed diagnostic performance was shown separately when all the three parameters are above the cut-off values and when either of these parameters was above the cut-off value [Table/Fig-3]. Sensitivity, specificity, PPV, NPV and DA with 95% CIs are 60.9%, 98.2%, 96.1%, 77.5% and 82.5% respectively when all the three parameters are above the cut-off values. Similar diagnostic indices (Sensitivity, specificity, PPV, NPV and DA) were 95.1%, 44.6%, 55.7%, 92.6% and 66.0% respectively when any of these three parameters were above the cut-off values.
Diagnostic performance of combined parameter.
| Parameter | Sensitivity(% [95% CI]) | Specificity(% [95% CI]) | PPV(% [95% CI]) | NPV(% [95% CI]) | DA(% [95% CI]) |
|---|
| CRP and WBC and ANC | 60.9 (44.5–75.8) | 98.2 (90.4–99.9) | 96.1 (80.4–99.9) | 77.5 (66.0–86.5) | 82.5 (73.4–89.4) |
| CRP or WBC or ANC | 95.1 (83.5–99.4) | 44.6 (31.3–58.5) | 55.7 (43.3–67.6) | 92.6 (75.7–99.1) | 66.0 (55.6 – 75.3) |
PPV- Positive Predictive Value; NPV- Negative Predictive Value; DA - Diagnostic Accuracy; CRP-C-reactive Protein; WBC- White Blood Cell and ANC- Absolute Neutrophil Count
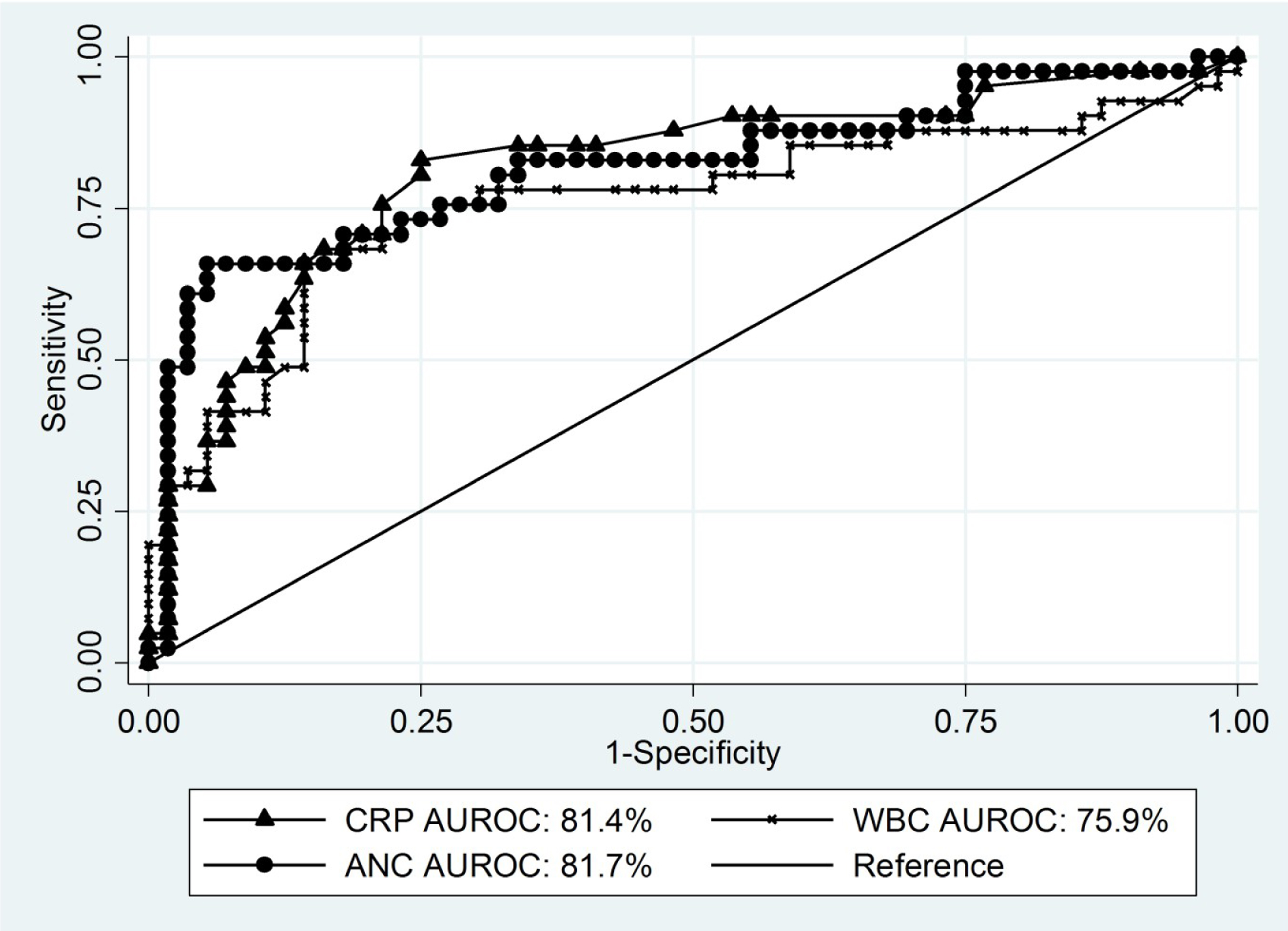
As shown in [Table/Fig-4] the area under the ROC curve (AUC) was 81.4% for CRP, 75.9% for WBC and 81.7% for ANC. The difference between AUCs for CRP, ANC or leukocyte count was found higher as compared to WBC.
Diagnostic performance through Area Under the Receiver Operating Characteristic curve (AUROC) for CRP, WBC and ANC.
CRP- C-reactive Protein; WBC– White Blood Cell Count; ANC- Absolute Neutrophil Count
Discussion
To differentiate bacterial from non BI classic infectious indices such as CRP and various haematological parameters are used in the evaluation of febrile children. We evaluated the role of infection markers such as total WBC, ANC along with CRP in the diagnosis of BI.
The high sensitivity of CRP (82.9%) indicates it can be useful for ruling out a BI if the level of CRP is below the cut-off value. Similarly, a high specificity (>70%) of all the parameters demonstrates that these are useful for ruling in patients with BI [Table/Fig-2].
This sensitivity increased to 95% when other two additional parameters (white blood count, absolute neutrophil count) were added indicating when the value of at least any one of these is below the cut-offs, it is a more useful indicator for ruling out a BI. Similarly when the value of all the parameters were above the cut-off, the specificity was 98.2% providing the usefulness of ruling in a BI.
Thayyil S et al., evaluated the usefulness of CRP in early diagnosis of severe BIs in children which showed a sensitivity of 75% and specificity of 68.7% which is lower than value of the current study of 83% and 75% respectively [8]. Andreola B et al., studied the predictive value of CRP in serious BI in children (1 week-36 months) with fever without focus. They reported that CRP has a sensitivity of 71.3% (61.0-80.1) and a specificity of 81.2% with a positive likelihood ratio of 3.79 and the negative likelihood ratio of 0.35 [9]. Our study showed positive likelihood ratios of 3.32 and the negative likelihood ratios of 0.23 which is comparable. The results of this study also showed that the quantitative CRP test is a valuable tool for distinguishing non BIs from BIs in febrile children. Hsiao AL et al., reported a positive likelihood ratio of 2.43 (95% confidence interval 1.73 to 3.43) and negative likelihood ratio of 0.61 (0.44 to 0.83) for white blood cell counts of 15,000/mm3 or more [10], and Andreola et al., reported a sensitivity of 51.6% (41.0-62.1), specificity of 75.5% (70.3-80.2), a positive likelihood ratio of 2.08 (1.58 to 2.75) and a negative likelihood ratio of 0.65 (0.52 to 0.80) for WBC counts>15,000/mm3 [9]. In our study the sensitivity and specificity for WBC counts >11,400/mm3 was 75.9% (95% CI: 59.7-87.6%) and 75.6 % (95% CI: 59.7-84.2%) respectively. This shows that WBC count assays provide less diagnostic value than tests for CRP. Our study shows that it has no role in ruling out BI but can be used to diagnose BI with reasonable accuracy. This finding is similar to other studies quoted by Den Bruel AV et al., in their systemic review [6].
Gwaiz LA and Babay AH, suggested that ANC is more accurate than total WBC in predicting bacteraemia as it was more sensitive than WBC [11]. However, Andreola B et al., demonstrated a sensitivity of 29.9% and specificity of 78.4% which indicates ANC is less sensitive but far more specific in predicting acute BI. Our study showed a sensitivity of 75.6% (59.7-87.6) and specificity of 73.2% (59.7-84.2) for ANC value of 6710/mm3.
Pulliam PN et al., demonstrated that CRP performs better in predicting severe BI in febrile children less than 36 months of age compared to leukocyte and neutrophil count [12]. Andreola B et al., demonstrated that CRP has a superior discriminatory power to total and differential WBC in detecting serious BI in children with fever without a source as it is more sensitive and specific which is comparable to our study [9]. The same results concerning the CRP and procalcitonin value in evaluating young children with bacterial or viral infection were demonstrated by the study of Olaciregui I et al., [13]. In a recent study Kossiva L et al., evaluated the parameters complete blood count in combination with CRP and ESR to distinguish the presence from the absence of infection [14]. In the current study, CRP has a better discriminatory power with higher sensitivity and specificity as compared to WBC and ANC in predicting BI especially for ruling in patients who have a BI.
The confidence interval of the combinations of blood tests largely overlapped with the individual tests so it provided no additional diagnostic value over the individual tests in our study. It is important for the clinician to realise that there is no such thing as a positive or negative CRP. The test does not provide a biparous (yes/no) result but the value should be interpreted along with clinical and other laboratory parameters. One should also remember that the normal value itself may vary depending upon subject characteristics and laboratory methodology; hence the cut-off used varies widely from as low as 1 mg/L [15,16] to as high as 9 mg/L [17].
The CRP definitive cut-off value of 1.2 mg/L for paediatric infections well discriminates bacterial from non BIs and which has been indicated by area of under the ROC curve (81.4%).
Limitation
The limitation of the present study was the small sample size. Other limitations were, serial CRP levels in these patients would have been more helpful as a single CRP gives a probability but not a certainty of presence or absence of serious bacterial infection. Although, procalcitonin is considered to be more specific in predicting BI in febrile children because of lack of resources this biomarker was not included in our study.
Conclusion
C-reactive protein value of 1.2 mg/L well discriminates bacterial from non BIs. CRP alone is found to be good diagnostic criteria to assess the BI among the children and addition of clinical and/or laboratory parameters (WBC and ANC) may enhance clinician’s abilities in the early recognition of clinically undetectable serious BI.
Hence, the combination of total WBC count, ANC along with CRP could be a reliable diagnostic tool to detect the presence of BI in infants and young children. As evident from likelihood ratio, routine ordering of CRP for detection of BI in febrile children is reasonably acceptable but further comparison of the performance of other diagnostic markers will be more meaningful to infer the diagnostic criteria for BI among children.
*-Based on Wilcoxon Rank Sum Test; $-Based on Chi-square test
Diagnostic accuracy, Likelihood Ratio Values of C-Reactive Protein (CRP), White Blood Cell (WBC) and Absolute Neutrophil Count (ANC) for Bacterial Infection Prediction
AUROC– Area Under the Receiver Operating Characteristic curve
LR+ positive Likelihood Ratio, LR- Negative Likelihood Ratio
PPV- Positive Predictive Value; NPV- Negative Predictive Value; DA - Diagnostic Accuracy; CRP-C-reactive Protein; WBC- White Blood Cell and ANC- Absolute Neutrophil Count