Acute Visual Loss as the Presenting Feature of Metastatic Upper Gastrointestinal Cancer-A Rare Case Report
Sandra Luz Treviño-Rodríguez1, Abraham Olvera-Barrios2, Jesús Hernán González-Cortés3, Hugo Alejandro Treviño-Rodríguez4, Jesús Mohamed-Hamsho5
1 Professor, Department of Ophthalmology, Hospital Universitario "Dr José Eleuterio González", Universidad Autónoma de Nuevo León, Monterrey, Nuevo León, Mexico.
2 Consultant, Department of Ophthalmology, Hospital Universitario "Dr José Eleuterio González", Universidad Autónoma de Nuevo León, Monterrey, Nuevo Leon, Mexico.
3 Professor, Department of Ophthalmology, Hospital Universitario "Dr José Eleuterio González", Universidad Autónoma de Nuevo León, Monterrey, Nuevo Leon, Mexico.
4 Professor, Department of Ophthalmology, Hospital Universitario "Dr José Eleuterio González", Universidad Autónoma de Nuevo León, Monterrey, Nuevo León, Mexico.
5 Professor, Department of Ophthalmology, Hospital Universitario "Dr José Eleuterio González", Universidad Autónoma de Nuevo León, Monterrey, Nuevo Leon, Mexico.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sandra Luz Treviño-Rodríguez, Av. Francisco I Madero, esquina con Gonzalitos sin numero, Oftalmologia HU, Monterrey, Nuevo León, Mexico.
E-mail: drasandytrevino@gmail.com
Choroidal metastases are the most frequent intraocular tumours in adults. Primary tumour sites include lungs in men (68%) and breasts in women (40%). Gastrointestinal cancer is the origin in only 2% of the cases, occurring in women. Only 30% of patients present to the ophthalmologist with no previous history of cancer.
We hereby report the case of a 41-year-old female with no relevant medical history, complaining of sudden-onset blurred vision in the right eye (OD: hand motion), since one day and 20/25 vision in the left eye (OS) due to bilateral, multifocal choroidal metastatic disease. Systemic treatment with carboplatin and paclitaxel was started and the patient refused to undergo orbital External Beam Radiotherapy (EBRT). A follow up of four weeks recorded the rapid progression of bilateral exudative retinal detachment, increase in size of choroidal lesions, visual acuity decline (OD: Light perception, OS: Count fingers, at her last visit), as well as appearance and worsening of systemic symptoms.
This represents a relevant example of a serious underlying multiorgan disease diagnosed after an ophthalmologic examination. Our report highlights the importance of including the differential diagnosis of uveal metastases in patients with suspicious posterior segment lesions despite the absence of systemic symptoms.
Intraocular tumours, Metastases, Metastatic disease, Serous retinal detachment, Uveal
Case Report
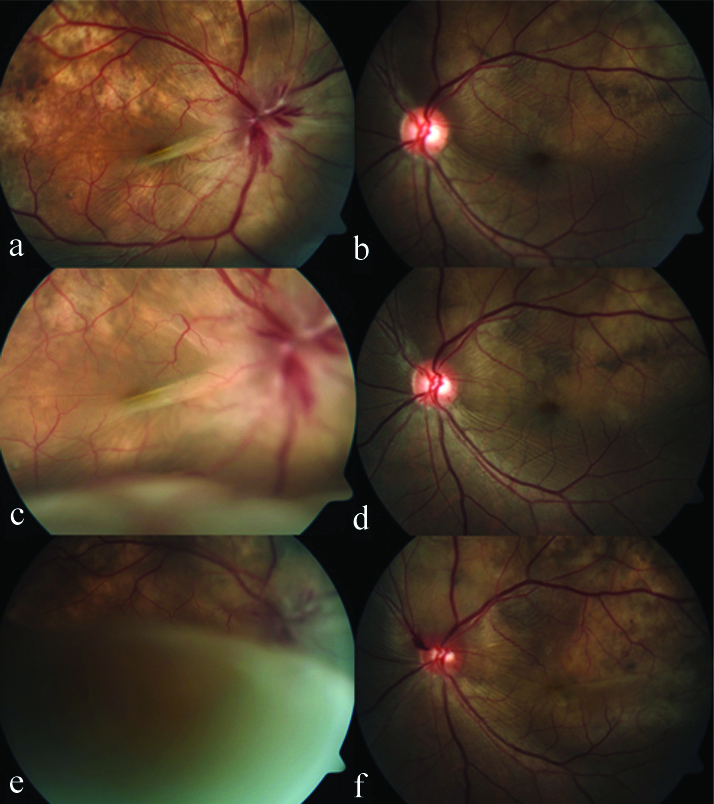
A 41-year-old female without a relevant medical history reported to the ophthalmology clinic, complaining of painful, sudden-onset, non progressive blurred vision in the right eye, since one day, associated with redness. Her best corrected visual acuity was hand motion OD and 20/25 for the OS. Automated refraction revealed: Sphere +7.50, Cylinder -0.75, OD; and Sphere: 0.00, Cylinder: 0.00, OS. On anterior segment biomicroscopy, the right eye showed sectoral hyperaemia of the temporal bulbar conjunctiva, chemosis and engorged scleral temporal vessels with a violaceous tinge and tenderness, along a quiet anterior chamber. The cornea was clear, and pupillary reflex testing showed no abnormalities. Left anterior segment examination was unremarkable. Intraocular pressure by means of Goldmann applanation tonometry was 7 and 10 mmHg for OD and OS, respectively. Funduscopic examination under mydriasis revealed radial retinal folds emanating from the Optic Nerve Head (ONH) with subretinal fluid (OD>OS), along with an area of pigmentary mottled changes of a mild creamy yellow-white appearance in relation to the superior temporal vascular arcade for both eyes (OU). An inferior Serous Retinal Detachment (SRD) was evidenced bilaterally (OD>OS). The right ONH was oedematous, hyperaemic, and an inferotemporal flame-shaped haemorrhage was seen. Venous pulse was absent. The left ONH was normal. In both the eyes (OU) the vitreous was clear and no cells were present [Table/Fig-1a,b]. Rapid visual deterioration along with progression of the SRD OU was evidenced during follow up [Table/Fig-1c-f]. Visual acuity deteriorated in OD from hand motion to Light Perception (LP), and in OS from 20/25 to Count Fingers (CF), four weeks after the initial visit.
Color fundus photography of both eyes during a three-week follow up: a,b) Right and left fundus one week after the initial evaluation; c,d) Two weeks after initial visit, progression of the serous retinal detachment (SRD) with respective increase in subretinal fluid and enlargement of choroidal lesions is seen (OD>OS); e,f) After three weeks, further worsening for both eyes with increase of the inferior SRD OD; f) Left optic nerve head infiltration, an increase of subretinal fluid along a discrete SRD with macular involvement is evidenced.
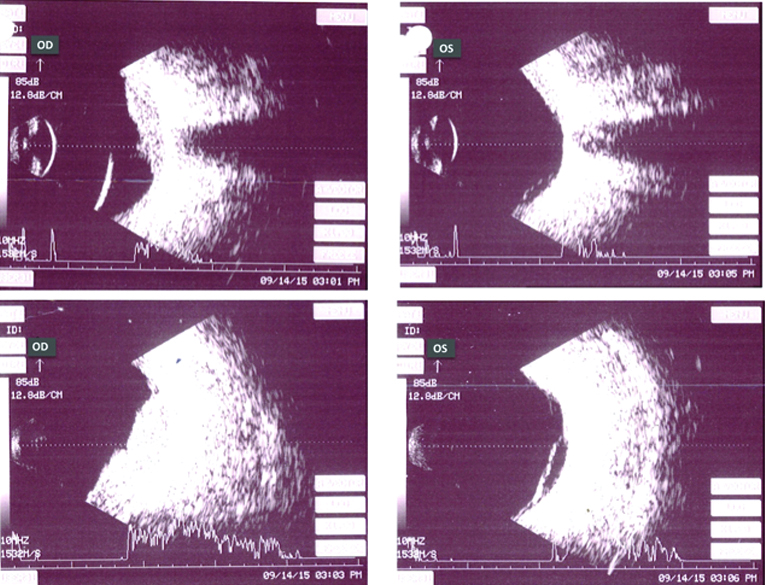
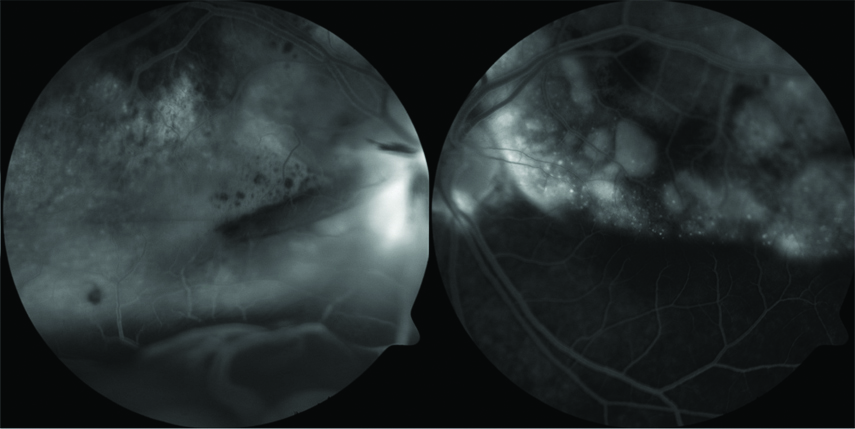
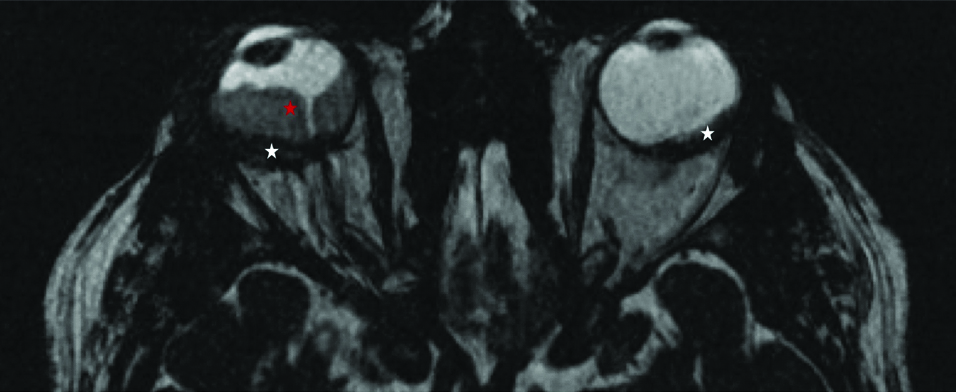
A-scan and B-scan ocular ultrasonography performed on the initial visit demonstrated bilateral highly echogenic choroidal lesions with moderate to high internal reflectivity (OD>OS) with ONH involvement of OD [Table/Fig-2]. On fundus fluorescein angiography, bilateral mottled hypofluorescent areas in the early phase, that became hyperfluorescent in relation to the superior vascular temporal arcades OU were evidenced [Table/Fig-3]. After further questioning about systemic symptoms, the patient complained of a three-month history of a persistent, non productive cough and a work-up for choroidal metastases was carried out. Chest X-ray evidenced an illdefined radiopaque lesion in the lower lobe of the left lung. The patient was immediately referred to the Pulmonary and Critical Care Department of the hospital and also for thoracic Computed Tomography (CT) scan and magnetic resonance imaging of the brain [Table/Fig-4].
Left column: A-scan and B-scan ocular ultrasonography of the right eye. Right column: left eye, less prominent choroidal lesions with the same ultrasonographic properties that spare the optic nerve head, inferior peripheral serous retinal detachment is shown.
Fluorescein angiography two weeks after the initial visit. Left image: disseminated early hypofluorescent lesions with a mottled pattern and late hyperfluorescence with diffuse leakage due to the serous retinal detachment on the right eye. Right image: left eye, early mottled hypofluorescence with late hyperfluorescence and pooling of fluorescein inside the tumoural lesions is evidenced in relation to the superior temporal vascular arcades.
Brain magnetic resonance imaging. Fast imaging employing steady-state acquisition sequence showing a bilateral, irregular increase in choroidal thickness and volume of up to 5.8 mm in the right eye, and up to 3.8 mm in the left eye (white stars). Both lesions show an intense homogeneous enhancement after the administration of contrast material. Serous retinal detachment is also evident (red star).
The chest CT scan revealed mediastinal adenopathy and a tumour of the left lung. Bronchoscopy, percutaneous biopsy and bronchoalveolar lavage resulted in the identification of a metastatic undifferentiated adenocarcinoma of upper Gastrointestinal (GI) tract origin by immunohistochemistry. Extension studies reported metastatic disease to the thyroid, right lung, liver and left suprarenal gland, in addition to the previously mentioned sites of involvement.
Systemic treatment with carboplatin and paclitaxel was started. EBRT was offered but not initiated because of the patients own decision. The family requested that the patient be transferred to a hospital in her hometown where she died three months after the diagnosis. The family did not consent an autopsy.
Discussion
This report represents a case of an advanced metastatic disease from upper GI origin, with blurred vision as the presenting clinical feature. Among the causes of acute visual loss, metastatic disease to the choroid is an infrequent, yet important and challenging diagnosis [1]. The differential diagnosis includes choroidal melanoma, osteoma, hemangioma, granuloma, neovascularisation with disciform scar and posterior scleritis [2]. After analysis of a series of 520 eyes, breast and lung were the most common primary sites for women and men, 68% and 40%, respectively. Metastatic gastrointestinal cancer is responsible for 9% of the cases in men and only 2% in women [1,3].
Choroidal metastases usually present late in the course of the disease with an incidence of about 10% in patients with malignant tumours [4]. Up to 30% of cases with ocular metastases have no previous history of cancer [1-3]. The most common location for metastatic lesions to the uvea is the posterior pole, with macular involvement in about 40% of the cases [1,2]. At the time of diagnosis 70% of the patients will experience painless visual loss; still 6 to 10% of the cases may remain asymptomatic [1]. Metastases present as flat, yellow or white lesions with a creamy appearance and secondary retinal changes such as SRD or atrophy of the Retinal Pigment Epithelium (RPE) [1,2]. It is reported that 20 to 40% of the cases are bilateral, and about 20% are multifocal [5], characteristics that represent important clues to the diagnosis and were of paramount importance in our patient. Though, several reports of uveal metastases exist, a disseminated metastatic disease of superior GI tract origin, manifesting initially as unilateral blurred vision presenting with bilateral and multifocal choroidal lesions in a female patient is a rather unusual presentation.
Treatment modalities consist of chemotherapy with EBRT [6,7] and the entity carries a poor prognosis with survival rates of 4 to 11 months [8,9].
Conclusion
Choroidal metastases are the most frequent intraorbital tumours. The diagnosis can be challenging since almost one third of the patients can present without a previous history of cancer. We highlight the importance of keeping the differential diagnosis of metastatic uveal disease in mind, even in the absence of systemic signs or symptoms, when suspicious intraocular lesions are evidenced, because of the mandatory multidisciplinary approach required for these cases.
[1]. Shields CL, Shields JA, Gross NE, Schwartz GP, Lally SE, Survey of 520 eyes with uveal metastasesOphthalmology 1997 104(8):1265-76.10.1016/S0161-6420(97)30148-1 [Google Scholar] [CrossRef]
[2]. Arepalli S, Kaliki S, Shields CL, Choroidal metastases: origin, features, and therapyIndian J Ophthalmol 2015 63(2):122-27.10.4103/0301-4738.15438025827542 [Google Scholar] [CrossRef] [PubMed]
[3]. Demirci H, Shields CL, Chao AN, Shields JA, Uveal metastasis from breast cancer in 264 patientsAm J Ophthalmol 2003 136(2):264-71.10.1016/S0002-9394(03)00192-2 [Google Scholar] [CrossRef]
[4]. Arevalo JF, Fernandez CF, Garcia RA, Optical coherence tomography characteristics of choroidal metastasisOphthalmology 2005 112(9):1612-19.10.1016/j.ophtha.2005.03.03016039718 [Google Scholar] [CrossRef] [PubMed]
[5]. Zhang HR, Ma ZZ, Feng Y, Guo T, Clinical characteristics of choroidal metastasisZhonghua Yan Ke Za Zhi 2009 45(4):301-08. [Google Scholar]
[6]. Wiegel T, Bottke D, Kreusel KM, Schmidt S, Bornfeld N, Foerster MH, External beam radiotherapy of choroidal metastases-final results of a prospective study of the German Cancer Society (ARO 95-08)Radiother Oncol 2002 64(1):13-18.10.1016/S0167-8140(02)00134-2 [Google Scholar] [CrossRef]
[7]. Amer R, Pe’er J, Chowers I, Anteby I, Treatment options in the management of choroidal metastasesOphthalmologica 2004 218(6):372-77.10.1159/00008093915564754 [Google Scholar] [CrossRef] [PubMed]
[8]. Hasturk S, Soylu M, Zeren EH, Hanta I, Basaloid large cell lung carcinoma presenting concurrently with metastatic uveal tumorLung Cancer 2001 32(1):95-101.10.1016/S0169-5002(00)00202-6 [Google Scholar] [CrossRef]
[9]. Shields JA, Shields CL, Eagle RC, Choroidal metastasis from lung cancer masquerading as sarcoidosisRetina 2005 25(3):367-70.10.1097/00006982-200504000-0002015805918 [Google Scholar] [CrossRef] [PubMed]