Cysticercosis is a parasitic infection caused by the larval form of pork tapeworm, Taenia solium. Disseminated cysticercosis is an unusual manifestation of cysticercosis which has been reported in endemic areas. Only a few cases of disseminated cysticercosis have been reported worldwide, to date in literature. Herein, we present an incidental finding of disseminated cysticercosis in a middle-aged male who had presented to us with multiple fractures following a road traffic accident.
Muscle, Neurocysticercosis, Open fractures, Skeletal/Parasitology, Taenia solium
Case Report
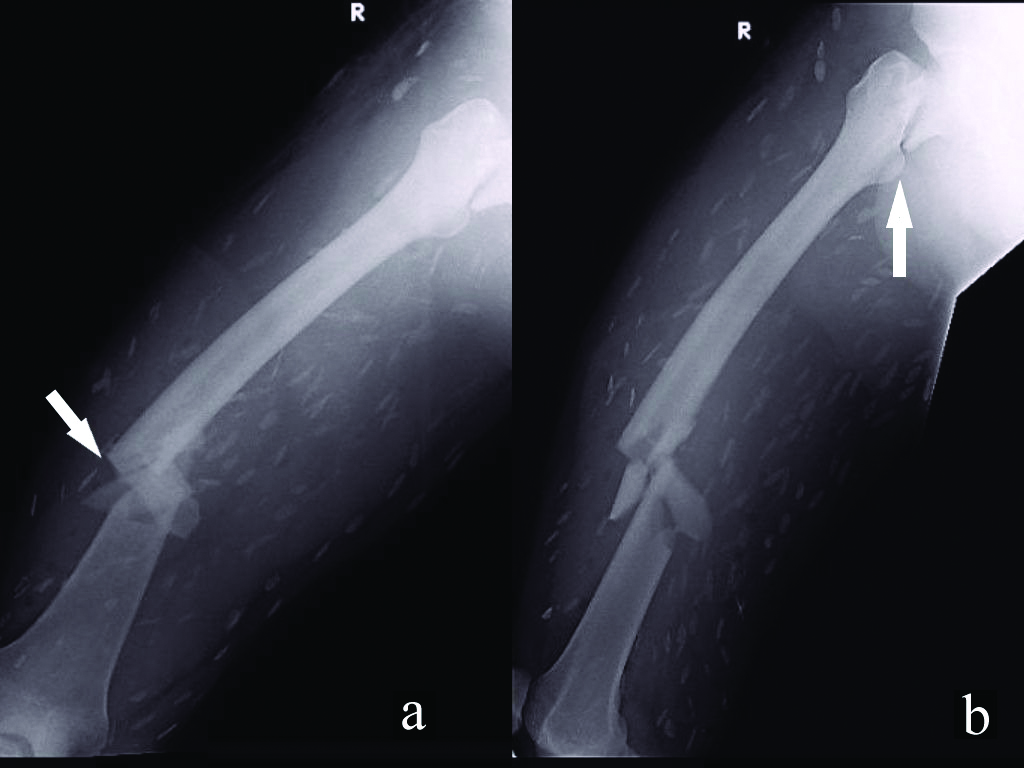
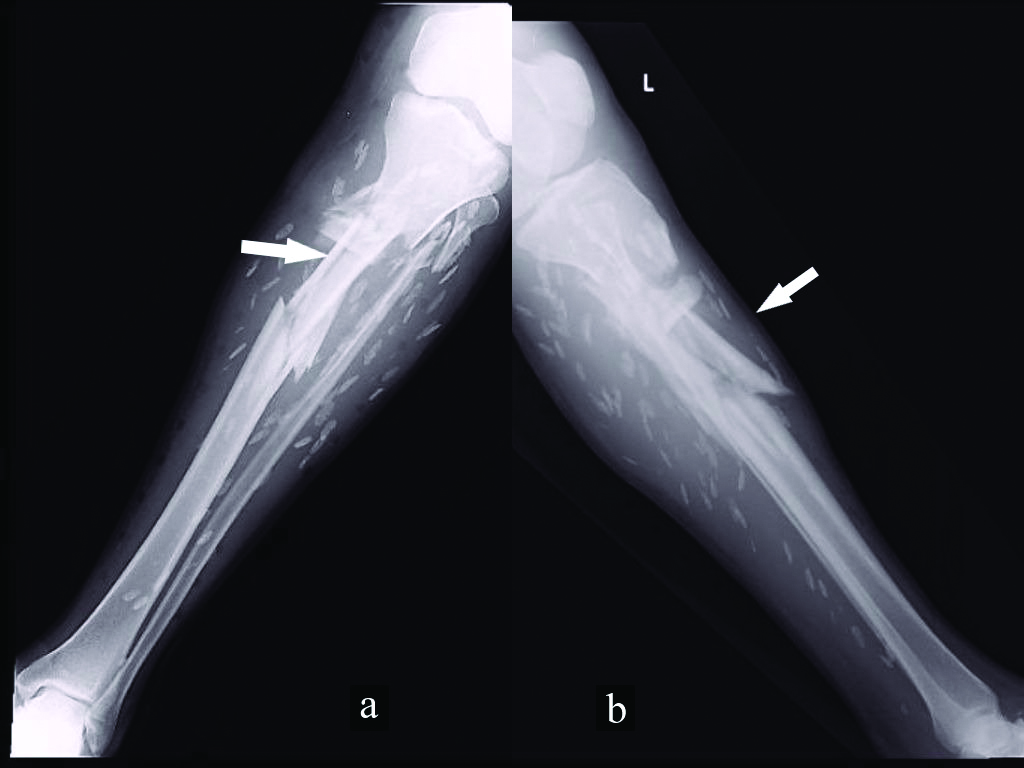
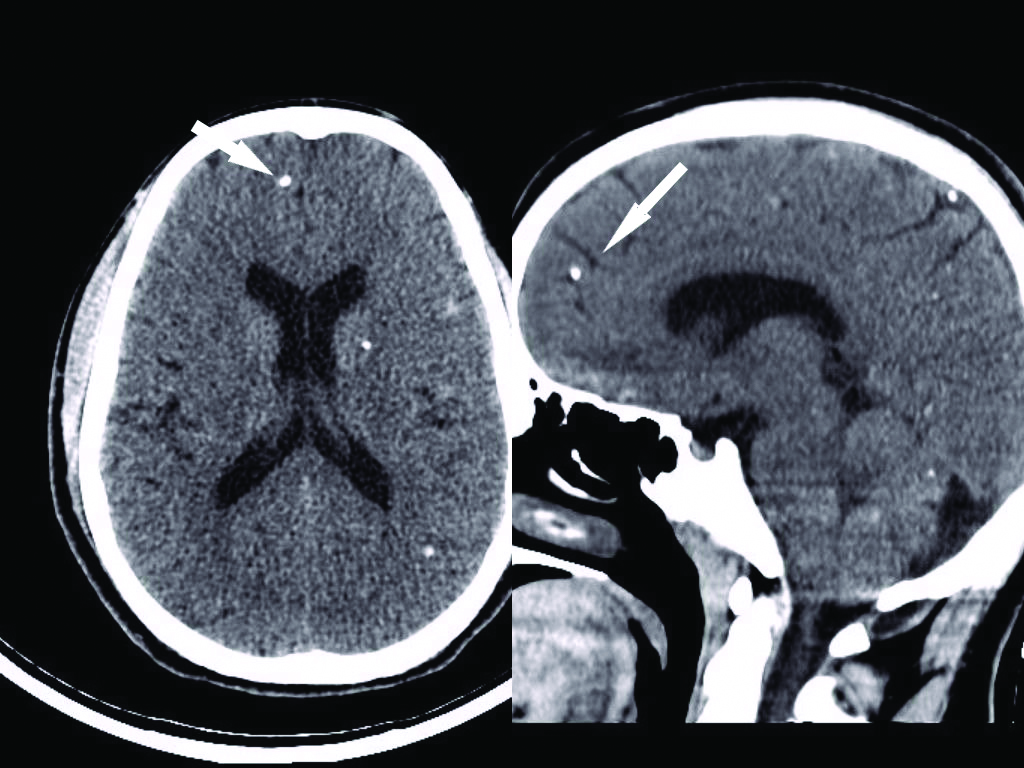
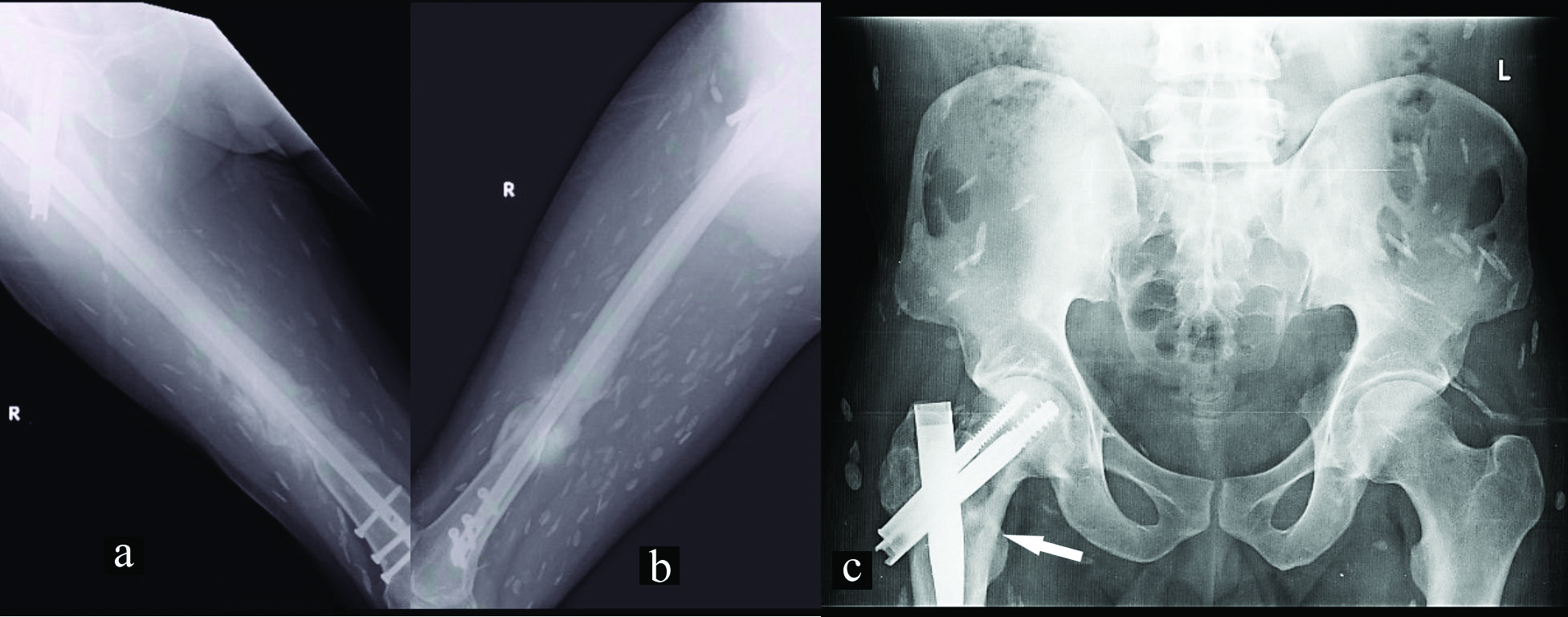
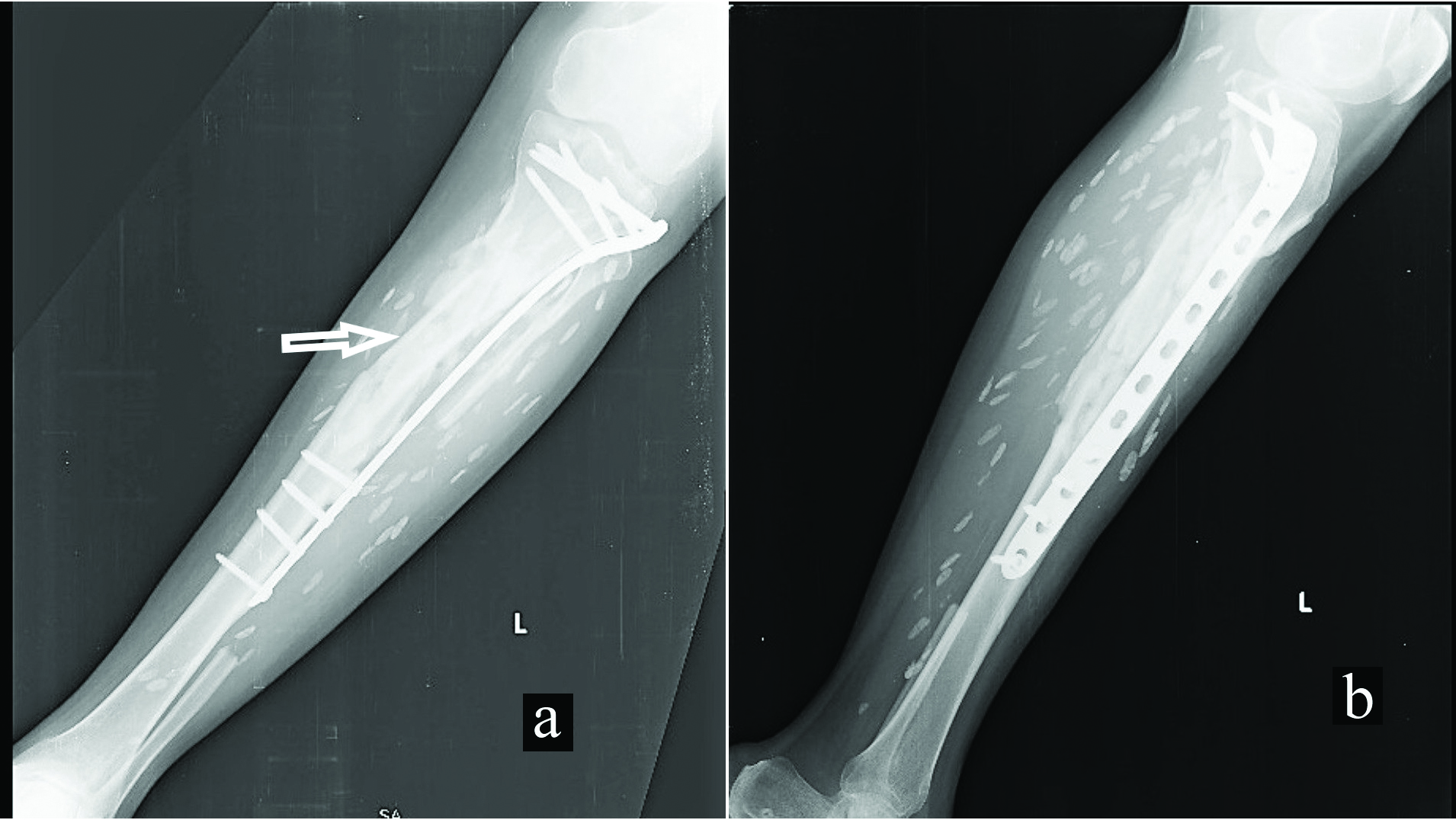
A 34-year-old male was brought to the trauma centre following a road traffic accident. He had deformities in his right thigh and left leg along with a wound over his left leg on the anteromedial aspect, about 5 cm below the knee joint with the tibia exposed and another wound over the lateral aspect of right thigh. On radiological examination, he had a basicervical fracture neck of femur with ipsilateral femur shaft fracture on the right side and fracture of left proximal tibia with metaphyseal comminution [Table/Fig-1,2]. To our surprise the radiographs taken for assessment showed numerous ‘cigar’ shaped multiple cysts in soft tissue plane of limbs, chest and the neck. On blood investigations, haemoglobin was 11 gm/dL, normal differential leucocyte count and total counts, the serum lactate was 22.5 mg/dL and erythrocyte sedimentation rate was 49 mm/hr. Renal and liver function tests were normal. The plain CT study of the brain showed multiple intra-axial small calcified foci at the white and grey matter junction involving both cerebral hemispheres diffusely, suggestive of nodular calcified stage of neurocysticercosis [Table/Fig-3]. The patient had a normal Glasgow Coma Scale (GCS) of 15. The fundus examination was normal.
Anteroposterior (a) and lateral X-rays (b) of right femur, the arrows show a basicervical fracture neck of femur with ipsilateral femur shaft fracture along with multiple disseminated calcified cysts in the surrounding soft tissue.
Anteroposterior (a) and lateral X-rays (b) fracture of left proximal tibia with metaphyseal comminution with disseminated calcified cysts in surrounding soft tissue.
CT scan of the brain with arrows showing multiple cysts disseminated in the brain.
The patient gave a history of regular consumption of pork. He did not have any history of seizures, headache, vomiting, sleep disturbances, myalgia or any disturbance in vision. Echocardiography did not show any cardiac involvement and electrocardiogram was normal. On physical examination of uninjured limbs, we noted few non tender nodes in the subcutaneous plane which the patient, had noticed them more two years earlier. A provisional diagnosis of right sided basicervical fracture neck of femur with ipsilateral Type II open fracture of the femur shaft, Type II open fracture of left proximal tibia with disseminated cysticercosis was made based on the history, physical findings and radiography which showed the above-mentioned fractures and multiple calcified cysts in subcutaneous and intramuscular plane. However, the differential diagnosis of multiple neurofibromatosis was kept in mind in view of multiple painless nodules.
The patient was taken up for surgery at the earliest in view of open fractures to prevent complications associated with it. However, there were two main concerns, first being the epileptogenic nature of his pre-existing condition as there was dissemination into the brain and second being the chances of anaphylaxis that could be caused due to rupture of cysts during the wound debridement and surgical fixation of fractures.
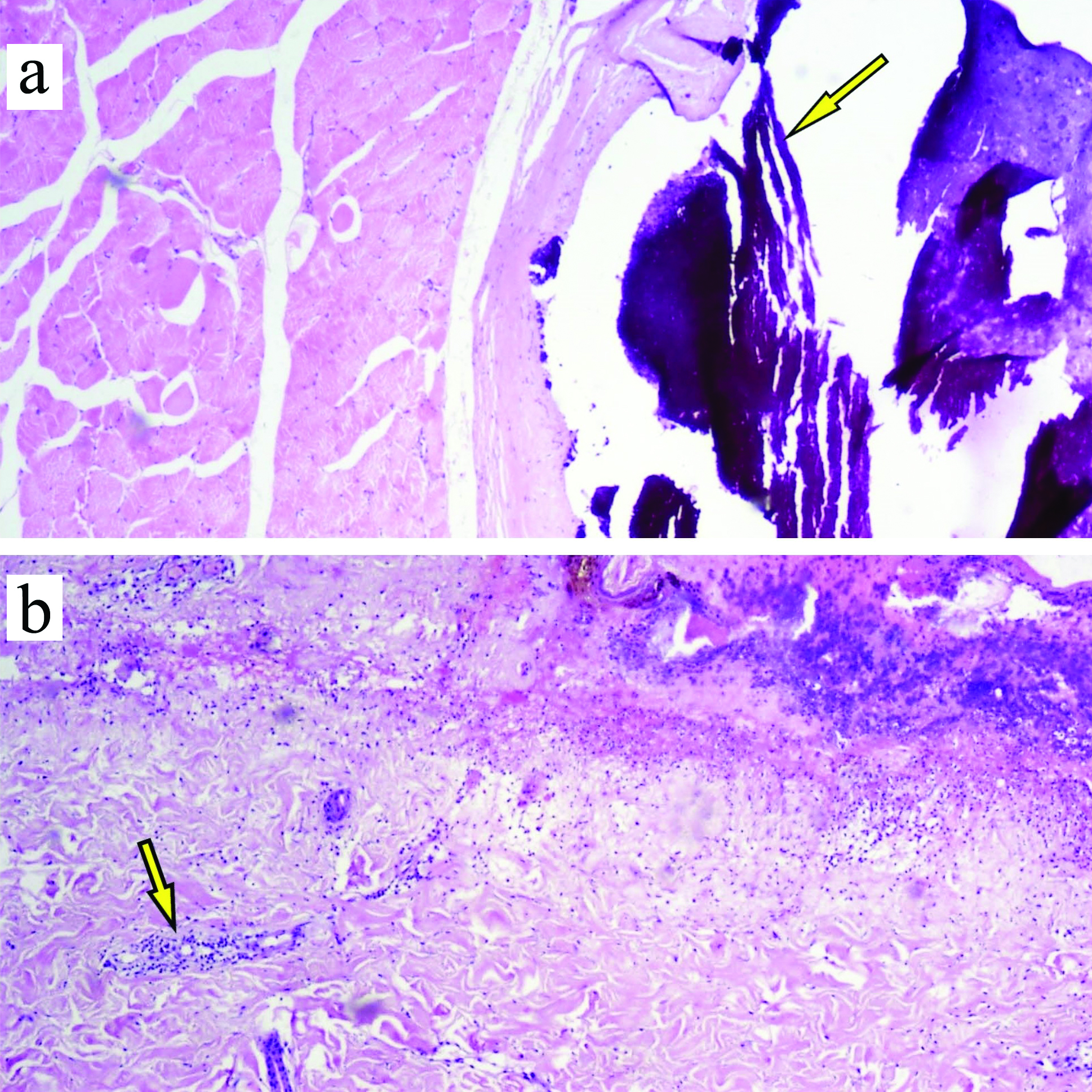
The patient and his attenders were appraised about his condition and the risks, following which he was taken up for surgery under the cover of phenytoin and corticosteroids. He underwent debridement and proximal femoral nailing for the right femur and debridement and Minimally Invasive Plate Osteosynthesis (MIPO) using a lateral proximal tibial plate. The perioperative period was uneventful. The cysts found during debridement were sent for histopathological analysis [Table/Fig-4], dystrophic calcification enclosed by fibrocollagenous capsule with scanty lymphocyte infiltration, there was no evidence of parasites, granulomas [Table/Fig-5]. Post operatively three consecutive days of early morning stool samples showed no parasites, ova or any cysts. As per the advice of physicians, the patient was not started on any anti-helminthic as he was totally asymptomatic and the cysts in the body were calcified.
Gross specimen of calcified cysts with surrounding muscle.

Histopathology image: a) arrow showing dystrophic calcification (H&E stain 10X); b) showing fibrocollagenous capsule with scanty lymphocyte infiltration.
During the follow up the fractures in the right lower limb united uneventfully [Table/Fig-6], while the proximal tibial fracture did not show any signs of union at 12 weeks. For which he underwent bone grafting using grafts from fibula and iliac crest [Table/Fig-7].
Post operative anteroposterior (a) and lateral (b) X-rays of right femur and anteroposterior view of pelvis (c) with fracture union.
Post operative anteroposterior (a) and lateral (b) X-rays of left tibia after bone grafting.
Discussion
Cysticercosis cellulosae is the larval form of Taenia solium. Humans are the definite host as they harbour the adult tapeworm, while pig is the intermediate host harbouring the larval stage. To develop the disease, the eggs enter the intestinal lumen through autoinfection or contaminated eatables [1].
Disseminated cysticercosis is of very rare occurrence, it is an uncommon manifestation of cysticercosis [2]. However, literature has a mention of various presentations and manifestations of this condition with dissemination of the cysts into the muscles, tendon sheath, brain, spinal canal and myocardium subcutaneous plane. The clinical presentation in the patient depends on the cyst burden, viability of the cyst, the host reaction and their location in the body [3]. The common features of disseminated cysticercosis include intractable epilepsy, dementia, lingual and subcutaneous nodules. Only a few cases have been reported to date where the patients have been asymptomatic despite dissemination in the body [4]. Saeed N et al., had previously reported an asymptomatic case of disseminated cysticercosis wherein the patient had presented with open fracture of the femur [5]. Our patient had been asymptomatic except few palpable painless subcutaneous nodules till the time of presentation.
On clinical examination, cysticercosis can easily be misdiagnosed as abscess, lipoma, tuberculous lymphadenitis, pyomyositis, neuroma, neurofibroma, or ganglion cysts depending on their location in the body [1]. Therefore, it is important to elicit a thorough history and to conduct a detailed clinical examination to rule out above conditions.
The X-ray, CT and MRI are useful in localisation of cysts in the body. MRI is a better modality as it can differentiate the stages of the parasite [6]. In our patient also, X-ray showed multiple white radio-dense foci in muscles and CT showed dissemination into the brain. In addition, echocardiography was done to rule out dissemination in the myocardium. However, we didn’t get the MRI in our patient due to the emergency scenario.
Serological tests like Enzyme Linked Immunosorbent Assay (ELISA) and enzyme linked immunoblot assay can be used to detect antibodies against cysticercosis with the latter being more sensitive and specific for diagnosis [4].
Serious anaphylactic reaction can be caused due to rupture of the cysts and release of cyst fluid, the patient can have severe angioedema, hypereosinophilia and increased IgE levels [7]. This was one of the concerns in our patient as there was high risk of cyst rupture during the debridement and fixation of fractures. This is a serious complication of orthopaedic surgery in a patient with disseminated cysticercosis. Moreover, neurocysticercosis is epileptogenic in nature; hence, the patient was taken up for surgery under general anaesthesia under the cover of corticosteroids and antiepileptics.
On histopathology, cysticercosis can vaguely be classified into early, intermediate and late stages [5]. Based on histopathology our case corresponded to the late stage of the disease which showed calcification and an oedematous and fibrocollagenous stroma with foci of necrosis, neutrophilic, lymphocytic infiltrate and few eosinophils.
A multidisciplinary team approach is advocated in treatment as usually multiple systems may be involved. Active disseminated cysticercosis should be managed symptomatically with antiepileptics and steroids, surgically (in cases of neurocysticercosis) and with cysticidal drugs. Though controversial the use of cysticidal drugs like albendazole (15 mg/kg/day for 30 days) or praziquantel (10-15 mg/kg/day for 2 to 3 weeks) have been advocated in management of viable cysts, especially in the case of neurocysticercosis [4,8]. Recently, a critical review concluded that albendazole is more effective than praziquantel regarding clinically important outcomes in patients with neurocysticercosis [6].
Asymptomatic subcutaneous and intramuscular cysticerci do not require any treatment. There is no role for cysticidal drugs in case of calcified cysts as the parasites are dead. However, in case of widespread dissemination it is better to keep the patient under close watch as few cysts may still be active, and patient may become symptomatic later.
Conclusion
Disseminated cysticercosis should always be a differential diagnosis of subcutaneous and intramuscular swellings, especially in endemic areas. In unusual presentation of disseminated cysticercosis with multiple fractures as in our case, it is essential to be aware of serious anaphylactic reaction that could occur due to rupture of the cysts while fixing the fractures.
[1]. Krishnaswami CS, Case of cysticercus celluloseInd Med Gaz 1912 27:43-44. [Google Scholar]
[2]. Kumar A, Bhagwani DK, Sharma RK, Kavitha Sharma S, Datar S, Disseminated cysticercosisIndian Pediatr 1996 33:337-39. [Google Scholar]
[3]. Thamilselvan P, Muthuraman K, Thasan S, Kasinathan G, Mandal J, Parija S, A stratified analysis of clinical manifestations and different diagnostic methods of neurocysticercosis-suspected Tamilian population residing in and around puducherryJ Clin Diagn Res 2017 11(5):DC10-15.10.7860/JCDR/2017/23711.984428658758 [Google Scholar] [CrossRef] [PubMed]
[4]. Banu A, Veena N, A rare case of disseminated cysticercosis: case report and review of literatureIndian J Med Microbiol 2011 29:180-83.10.4103/0255-0857.8178721654117 [Google Scholar] [CrossRef] [PubMed]
[5]. Saeed N, Ehsan A, Vasenwala S, Disseminated cysticercosis incidentally diagnosed in patient of fracture shaft of femurBMJ Case Reports 2017 :bcr201621745110.1136/bcr-2016-21745128246113 [Google Scholar] [CrossRef] [PubMed]
[6]. Nasim M, Agarwal S, Disseminated cysticercosis incidentally diagnosed in a patient of low backache: A case report and concise review of literatureAsian Pacific Journal of Tropical Medicine 2012 :582-86.10.1016/S1995-7645(12)60103-5 [Google Scholar] [CrossRef]
[7]. Minciullo PL, Cascio A, David A, Pernice LM, Calapai G, Gangemi S, Anaphylaxis caused by helminths: review of the literatureEur Rev Med Pharmacol Sci 2012 16(11):1513-18. [Google Scholar]
[8]. Bhalla A, Sood A, Sachdev A, Varma V, Disseminated cysticercosis. A case report and review of literatureJ Med Case Rep 2008 2:13710.1186/1752-1947-2-13718447915 [Google Scholar] [CrossRef] [PubMed]