Previous studies reported that the local anesthetics used during dental procedures, antibiotics, and NSAIDs are the most prescribed drugs in dentistry; however, their prescription pattern varies in different countries [1,2]. Despite the beneficial anti-inflammatory and analgesic properties of NSAIDs, the use of these agents could be associated with an increased risk of Gastrointestinal (GI), renal and cardiovascular complications [3,4]. Also, NSAIDs use during pregnancy cause potential adverse effects including labor prolongation, the constriction of the ductus arteriosus, haemostatic and renal abnormalities in the foetus and neonate [5].
In dentistry, antibiotics are prescribed either for the treatment of dental infections or prophylaxis of local and systemic dental infections. Most of previous studies are focused on antibiotic prescription pattern by dentists and there are few valid reports regarding dentists’ analgesic prescription patterns. Antibiotic prescription patterns varies among dentists in different countries but β-lactams, macrolides and metronidazole are the most commonly prescribed antimicrobials by dentists [1,6-10].
Analgesics and especially NSAIDs are the second most frequently prescribed drugs by dentists but the type of NSAIDs prescription varies among dentists in different part of the world [11-13].
There are limited valid reports on dentist’s prescription pattern for NSAIDs and there is a variation in the type of prescribed NSAIDs, as well as antibiotics, in different parts of the world and the choice of either NSAIDs/antibiotics for treatment of dental complications shows a significant variation among dentists in different countries, so this study was performed to analyse the antibiotics and NSAIDs prescription patterns by dentists, using a systematic review.
Materials and Methods
Search Strategy
A systematic review of literature relating to dentists prescription patterns of NSAIDs and antibiotics including the type of study (prophylaxis or treatment), antibacterial drug category, type of antibiotics, type of NSAIDs, type of non-opioid and opioid analgesics were searched from January 2000 to December 2016. Reports were extracted by several databases including PubMed, MEDLINE and Scopus and assessed all relevant articles using a structured data abstraction process. An electronic search for PubMed database was performed by https://www.ncbi.nlm.nih.gov/pubmed/ link and Scopus articles were searched using https://www.scopus.com/search for document searches. The search strategy included English language and all original articles or review studies that reported the dentists’ prescription pattern of NSAIDs and antibiotics for either prophylaxis or treatment of dental complications, using WHO (1993) GP prescribing indicators criteria [14].
Search Terms
The following keywords were used as the grouped terms (dentists, prescription patterns, dentists’ prescription patterns) and (NSAIDs or non-opioid analgesics or opioid analgesics or antimicrobials or antibiotics). From each report, information about the type of study (prophylaxis or treatment), antibacterial drug category, type of antibiotics, type of NSAIDs, name of non-opioid analgesics and name of opioid analgesics was extracted.
Selection Criteria and Review Procedure
Each potential study was reviewed independently by two authors for the eligibility for dentists’ prescription patterns for NSAIDs/antibacterial drugs, using WHO (1993) GP prescribing indicators criteria [14]. In the case of disagreements about the eligibility of a study, the two authors discussed the eligibility criteria and came to a final decision.
Due to restricted researches on dentists’ prescription patterns, we did not set any specification for sampling procedure and study quality to obtain a full coverage of documented topics. We included studies that either specifically titled dentists NSAIDs, antibiotics or dentists’ prescription patterns.
Prescriptions which did not meet the WHO (1993) GP prescribing indicators criteria (drugs per prescription; generic or brand name; drug category and injections) and also the percentage or the frequency of prescribed drugs were excluded from the study [14].
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist was used for article selections. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) check list was used to assess reported items quality related to article’s title and abstract, the introduction, methods, results and discussion sections and funding [15].
Data Extraction and Data List Items
All the data that fulfilled our eligibility criteria were extracted independently by two authors. The prescription pattern studies have been found to be heterogeneous, as they were conducted in different countries by different methods, i.e., data collection was performed from patient’s prescription or questionnaire data for either prophylaxis or treatment purposes or NSAIDs/antibacterial prescription patterns. So, for this reason we did not try to analyse the data from a statistical viewpoint; but, the results are summarised according to the type of antibacterial/or NSAIDs prescription drugs. Finally, the name of the main author, the country which the study was performed, type of antibacterial drug, types of NSAIDs drug, type of analgesic drug prescribed was recorded in the appropriate tables.
Results
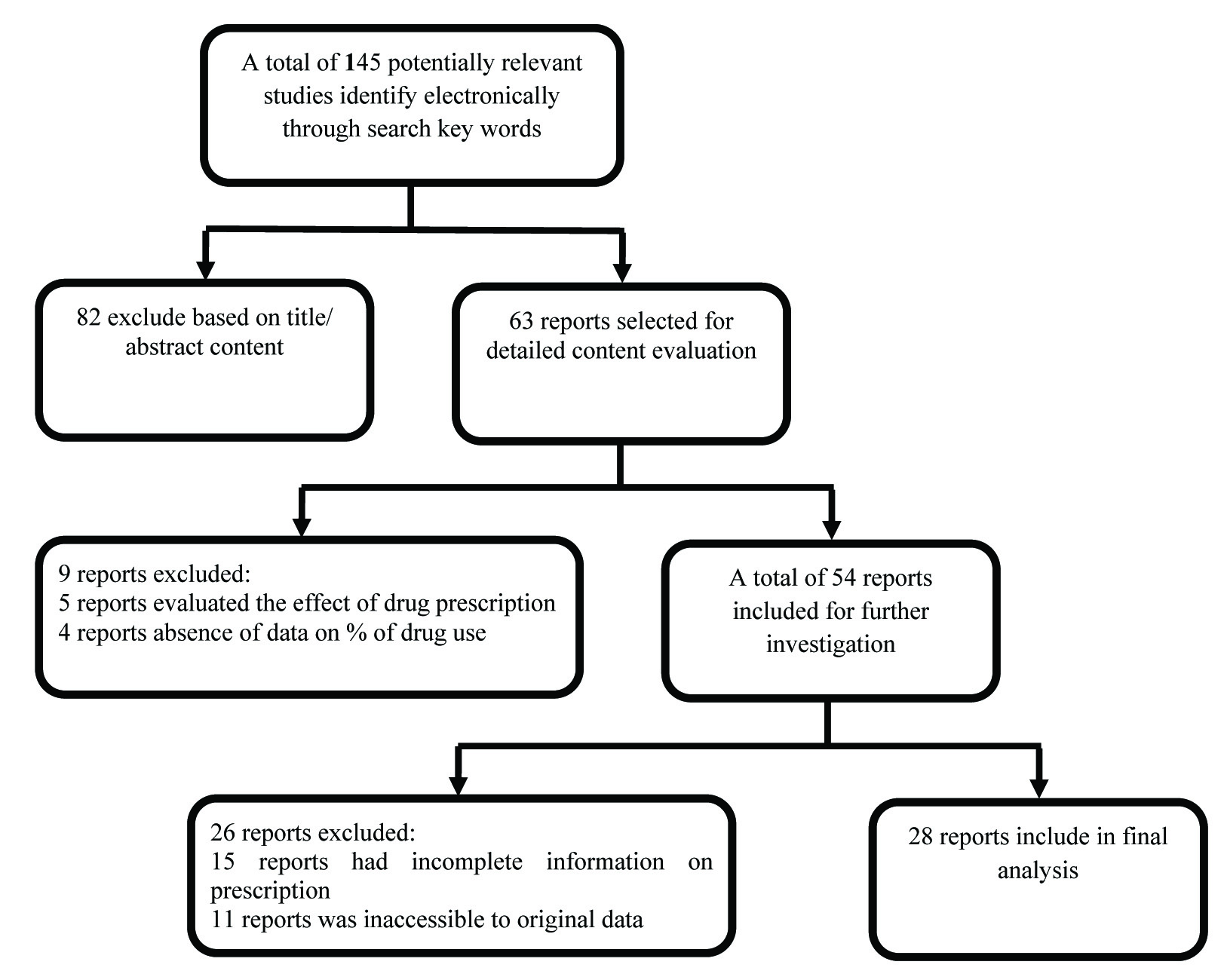
A total of 145 related topics in Scopus, PubMed and MEDLINE for dentists’ prescription were identified by our database search [Table/Fig-1]. Following an initial screening step, 82 articles were excluded either by title/abstract content. Then 63 article titles were selected for further investigations. Among the selected papers, nine reports excluded because five reports evaluated the effects of interventions on the trend of drug prescription and in four reports the percentage of drug used was absent. Further, 54 reports were selected for detailed content evaluations. Among these 26 articles were excluded for the following reasons: 15 reports had incomplete information for prescription (drugs per prescription; generic or brand name; the percentage or the frequency of prescribed drugs) and in 11 reports we had no access to the original data including tables, figures and total number of prescriptions & methods of data collection. Finally, 28 articles met criteria for inclusion i.e., type of antibiotics, type of NSAIDs, non-opioid analgesics and opioid analgesics as suggested above. All of the 28 papers fulfilled the requirements based on STROBE checklist including article’s the title and abstract, the introduction, methods, results and discussion sections and funding. Overall 21 articles reported the antibacterial prescription, four articles reported the NSAIDs prescription and three articles reported the prescription pattern for the combinations of both NSAIDs and antibacterial drugs.
Flow Chart for scientific reports selection for dentists’ prescription pattern of NSAIDs and antibiotics.
Our results showed that most studies on dentists prescription patterns were done on evaluating antibiotics prescribed in dental problems, i.e., 24 (21 studies solely on antimicrobials and three studies are combinations) out of 28 published researches which had the inclusion criteria for this study reported the antibiotic prescription pattern by dentists. Our results showed that the β-lactams were the most frequently prescribed antibacterial drug category followed by metronidazole and macrolides [16-22]. Amoxicillin (23 out of 24 studies) was the most frequently prescribed antibacterial and ibuprofen (six out of seven studies) was the most frequently prescribed NSAIDs in most countries [1,2,6,11,17,19,21,23-25]. Among antibacterials, prescription rates of amoxicillin by dentists varied from 12.5% in Croatia to 95% in Canada [20,26]. Also, amoxicillin was the drug of choice for endodontic prophylaxis for most of published papers. Amoxicillin/clavulanic acid (augmentin) was the most common prescribed drug in some countries such as Croatia (60.0%), Saudi Arabia (45.2%), Spain (61.0%) and Turkey (61.8%) [9,26-28]. Penicillin V was the other β-lactams used more frequently [Table/Fig-2,3] [7,23,29-31].
Findings from different studies conducted to evaluate prescribing pattern of antibiotics by dentists.
| Source | Place of study | Antibiotics prescribed(% of prescribed drug by dentists) | Methods of Data collection |
|---|
| Ford P et al., [17] | Australia | Amoxicillin (66.3%)/Metronidazole (13.6%)/Augmentin (7.1%)/Clindamycin (6.1%)/Cephalexin (3%)/Erythromycin (2%)/Penicillin V (1%)/Doxycycline (0.3%) | Dispensed medicine use data in Australia from 2001 to 2012 |
| Jaunay T et al., [18] | Australia | Amoxicillin (78-90%)/Metronidazole (20- 84%)/Tetracycline (20- 33%) | Questionnaires (n=85) |
| Lauber C et al., [20] | Canada | A- RoutinelyAmoxicillin (95%) B- Allergy to penicillin:Clindamycin (82%)/Erythromycin (10%) | Questionnaires (n=1500) |
| Perić M et al., [26] | Croatia | Augmentin (60.0%)/Clindamycin (14.8%) Amoxicillin (12.5%)/Metronidazole (11.5%)/Cephalexin (4%)/Azithromycin (1.2%) | Questionnaires (n=1500) |
| Cope A et al., [7] | England | Antibiotics (95.3%)/Amoxicillin (56.1%)/Metronidazole (31.3)/Erythromycin (4.4%)/Penicillin V (1.4%)/Clindamycin (0.6%) | Prescriptions of dental patients (n=5460) |
| Palmer N et al., [31] | England | Amoxicillin (75.5%)/Penicillin V (15.2%)/Erythromycin (4.4%)/Metronidazole (1.7%) | Prescriptions of dental patients (n=18614) |
| Konde S et al., [19] | India | Amoxicillin (70-86%)/Ofloxacin + Ornidazole (6-13%) /Cephalexin (2-12%)/ Clindamycin (5-6%) | Questionnaires (n=200) |
| Kakoei S et al., [23] | Iran | A- Routinely:Amoxicillin (90.1%)/Metronidazole (69.1%)/Penicillin (50.5%)/Ampicillin (16.8%) B- Allergy to penicillin:Erythromycin (66%)/Clindamycin (44%)/Metronidazole (27%) | Questionnaires (n=113) |
| Vessal G et al., 2011 [22] | Iran | Amoxicillin (44.2-75.4%)/Metronidazole (27.5%)/Penicillin (24.2%)/Tetracycline (13%)/Penicillin V (12.7-21.9%) | Questionnaires (n=219) |
| Dar-Odeh NS et al., [16] | Jordan | Amoxicillin (60%)/Metronidazole (39.4%)/Cephalosporins (11.11%)/Clindamycin (4.2%)/Doxycycline (2.6%) | Prescriptions of dental patients (n=2133) |
| Salako NO et al., [32] | Kuwait | A- Routinely:Amoxicillin (56.5-86.5%)/ Penicillin (9.1-23.7%)/Metronidazole (7.9-17.6%) B- Allergy to penicillin:Erythromycin (66.1%)/Cephalosporines (13.3%)/Metronidazole (7.3%) | Questionnaires (n=168) |
| Skučaitė N et al., [34] | Lithuania | Amoxicillin (50.4%)/Augmentin (25.6%)/Penicillin V (12.1%)/Lincomycin (3.4%) | Questionnaires (n=1431) |
| Ogunbodede E et al., [33] | Nigeria | Penicillin V (36.4%)/Metronidazole (16%)/Ampicillin (12.5%)/Ampiclox (8%)/Erythromycin (7%)/Tetracycline (4.2%)/Penicillin G procaine (2.2%)/Co-trimoxazole (2.2%) | Prescriptions of dental patients (n=313) |
| Iqbal A [27] | Saudi Arabia | Augmentin (45.2%)/ Amoxicillin (33.7%)/Amoxicillin + Metronidazole (15%)/Metronidazole (5.7%)/Clindamycin (4.4%)/Cephalosporines (2.5%) | Questionnaires (n=157) |
| Roy KM and Bagg J [30] | Scotland | Amoxicillin (49.1%)-Metronidazole (22.2%)-Penicillin V (18.5%)-Erythromycin (6.6%) – Cephalosporins (1.5%) – Ampicillin (0.9%) – Tetracyclines (0.6%)-Clindamycin (0.5%) | Prescriptions of dental patients (n=3550) |
| Sancho-Puchades M et al., [21] | Spain | A- Routinely:Amoxicillin (65-87%)/Augmentin (13-34%)B- Allergy to penicillin:Clindamycin (93.1%)-Erythromycin (7.7%)-Spiramycin (3.4%)-Azithromycin (3.4%) | Questionnaires (n=69) |
| Segura-Egea J et al., [28] | Spain | A- Routinely:Augmentin (61%)/Amoxicillin (34%)B- Allergy to penicillin:Clindamycin 300mg (65%)Azithromycin (15%)-metronidazole- spiramycin (13%) | Questionnaires (n=127) |
| González-Martínez R et al., [8] | Spain | A- Routinely:Amoxicillin (81%)-Augmentin (47.6%)-Clindamycin (38.1%)B- Allergy to penicillin:Clindamycin (66.7%)-Erythromycin (28.6%) | Questionnaires (n=134) |
| Arteagoitia MI et al., [6] | Spain | Amoxicillin (58.3%)/Augmentin (34.5%)/Spiramycin+ Metronidazole (2.2%)/Clindamycin (1.8%)/Metronidazole (1.3%) | Questionnaires (n=261) |
| Vlcek D et al., [25] | Swiss | Amoxicillin (45.7%)/Augmentin (33.7%)/Clindamycin (14.5%)/Others (6.1%) | Questionnaires (n=1795) |
| Kaplan RF et al., [9] | Turkey | Augmentin (61.8%)/Amoxicillin (46.5%)/Clindamycin (26.8%)/Metronidazole (19.7%)/Ampicillin (13.2%)/Penicillin G (7.1%)/Erythromycin (6.5%)/Clarithromycin (4.9%) | Questionnaires (n=589) |
N= number of questionnaires or prescriptions of the related study.
Findings from different studies conducted to evaluate prescribing pattern of combinations of antibiotics and NSAIDs by dentists.
| Source | Place of study | Antibiotics prescribed(% of prescribed drug by dentists) | NSAIDs prescribed | Methods of Data collection |
|---|
| Mainjot A et al., [10] | Belgium | Amoxicillin (51.1%)Augmentin (24.0%)Clindamycin (6.6%)Azithromycin (5.3%)Clarithromycin (4.4%)Doxycycline (4.4%)Spiramycin (2.2%) | NSAIDs (38.7%):Ibuprofen (82.5%)Paracetamol (22.8%) | Prescriptions of dental patients (n=1033) |
| Jayadev M et al., [1] | India | Amoxicillin (43.3%)Amoxicillin + Metronidazole (29.2%)Augmentin (16%)Ofloxacillin 200mg + Ornidazole 500mg (8.2%)Amoxicillin + Cloxacillin 500mg (3.4%) | Diclofenac (51.1%)Ibuprofen + Acetaminophen (18.8%)Ibuprofen (14.1%)Ketorolac (13.8%)Acetaminophen (2%) | Questionnaires(n=400) |
| Tanwir F et al., [2] | Pakistan | Total Antibiotics (17%):Amoxicillin+ metronidazole (80%)Amoxicillin (24%)Augmentin (16%)Clindamycin (1%)Others (4.8%) | Painkillers (64.2%):Ibuprofen (45.7%)Naproxen (26.1%)Diclofenac (11%)Paracetamol (7.9%)Flurbiprofen (9.2%) | Prescriptions of dental patients (n=709) |
N= number of questionnaires or prescriptions of the related study.
For patients with penicillin allergy, clindamycin was the most common alternative in some countries such as Canada and Spain. The clindamycin prescription rate for penicillin allergy ranged from 65% to 93.1% in Spain and 82% in Canada, whereas in other countries such as Iran and Kuwait, erythromycin was the most commonly alternative drug for endodontic prophylaxis (66% and 66.1%, respectively), followed by azithromycin and metronidazole [20,21,23,28,32]. Tetracyclines, clarithromycin, azithromycin, lincomycin and spiramycin were used in a limited rate in some countries [Table/Fig-2,3] [9,16-18,21,22,26,33,34].
Other antibacterial drug categories such as sulfonamides, aminoglycosides, chloramphenicol, vancomycin, second, third and fourth generations of cephalosporines and quinolones were not prescribed by dentists; although, one report showed the prescription of ofloxacin (fluoroquinolone) and ornidazole combination by paediatric dentists [19].
[Table/Fig-3,4] shows dentists’ prescription pattern of NSAIDs/analgesic drugs. Among the seven reports, ibuprofen was the most frequent prescribed NSAIDs/analgesics drug prescribed by dentists (6 out of 7 studies) followed by diclofenac, naprosin and paracetamol. Nimesulide, etodolac, flurbiprofen, and ketoprofen were other NSAIDs prescribed in a lower rate by dentists [11-13]. Oxycodone, hydrocodone and propoxyphene were the opioid analgesics prescribed alone or in combination with acetaminophen or ibuprofen [11,24].
Findings from different studies conducted to evaluate prescribing pattern of NSAIDs by dentists.
| Source | Place of study | NSAIDs prescribed(% of prescribed drug by dentists) | Methods of Data collection |
|---|
| Sarkar C et al., [12] | Nepal | 1-NSAIDs: (89.7%) | Prescriptions of dental patients (n=1820) |
| Ibuprofen (41%)Nimesulide (22%)Paracetamol + Ibuprofen (27%)Diclofenac (4%)Paracetamol (1%) |
| 2-Opioid analgesics (10.3%): |
| Paracetamol + propoxyphene (56%)Paracetamol + dextropropoxyphene (44%) |
| Mickel AK et al., [24] | USA | 1- NSAIDs: | Questionnaire (n=63) |
| 400 mg Ibuprofen (1.6%)600 mg Ibuprofen (31.7%)800 mg Ibuprofen (17.5%) |
| 2- NSAIDs + Opioid analgesics: |
| (11-17%)Vicodin®* (6.3%)Vicoprofen®† (4.8%)Ibuprofen_Vicodin® (12.7%)Ibuprofen_+ APAP** (4.8%)Lortab®†+ Ibuprofen (1.6%) |
| Barasch A et al., [11] | USA | 1-NSAIDs: | Prescriptions of dental patients (n=842) |
| Ibuprofen (57%)Naprosin (43%). |
| 2-Acetaminophen + Narcotics: |
| Acetaminophen/hydrocodone (67%)Acetaminophen/oxycodone (28%). |
| Şermet S et al., [13] | Turkey | 1-NSAIDs: | Questionnaires (n=130) |
| Naproxen (37.9%)Flurbiprofen (13.5%)Paracetamol (13.5%)Diclofenac (11.4%)Etodolac (3.8%)Ketoprofen (2.5%)Ibuprofen (2.1%) |
N= number of questionnaires or prescriptions of the related study.
*Vicodin® and Lortab®: Hydrocodone/acetaminophen, † Vicoprofen®: Hydrocodone/ibuprofen,
**APAP: Acetaminophen
Discussion
Our results showed that most studies focused mainly on antibacterial prescription patterns for prophylaxis and treatment of dental complications. Our results are in complete agreement with previous reports indicating that antibiotics and NSAIDs are the most frequent prescribed drugs by the dentists [12,13,26,34,35]. β-lactams, macrolides and metronidazole are the most frequent prescribed antibacterial drugs and ibuprofen was the most frequent prescribed NSAIDs by dentists [6,16,17,23,25]. Although, there was a wide range of variation in different countries, amoxicillin and amoxicillin/clavulanic acid (augmentin) were the most frequently antibacterial drugs prescribed by dentists, followed by metronidazole and clindamycin [2,9,27,28,34]. The amoxicillin prescription rate for treatment of endodontic infection showed a wide range of variation and marked differences in various countries, i.e., the lowest prescription rate for amoxicillin was reported in Croatia (12.5%) and the highest rate (95%) in Canada [20,26]. Although, amoxicillin was the most common prescribed antibacterials in most countries, amoxicillin/clavulanic acid (augmentin) was the most common prescribed antibacterial in some other countries but it is more expensive than amoxicillin and is used as alternative to β-lactamas resistant bacterial strains. Therefore, the empirical use of amoxicillin with clavulanic acid for treatment of dental infections is an evidence for increase in inappropriate use of antibiotics in dentistry which result in antimicrobial treatment failure and the development of resistance to antibiotics to commonly used antibiotics [19].
There is no confirmed information concerning the resistance of dental infections to commonly prescribed antibacterials. In this study, in almost all reports amoxicillin/clavulanic acid combination prescription was empirical which may result in the increase in growing resistance rate to commonly used antibacterials. Due to the increasing prevalence of bacteria which are resistant to treatment by commonly prescribed antibiotics, clinicians should be compliant with strict guidelines on the rationale use of antibiotics in dental practice. The diagnostic microbiology laboratory and the subsequent susceptibility testing is therefore important for guiding clinicians in the use of empirical therapy and managing resistant infections.
Our results showed that metronidazole was the second most frequently prescribed drug in combination with one or more antibiotics (mainly amoxicillin) for treatment of dental anaerobic infections. There was a wide range of variation in metronidazole prescription rate in different countries. The lowest prescription rate of 1.3-2.2% reported in Spain and the highest prescription rate of 84% in Australia [6,18]. Also, metronidazole prescription rate was relatively low in Norway (6.3-6.9%), Croatia (11.5%), Saudi Arabia (5.7 %) and almost high in Iran (69.1%), Jordan (39.4%) and England (31.3%) [7,16,23,27,36].
Metronidazole is used empirically to target anaerobic microorganisms, however, the emergence of resistance to this drug is low, therefore, the presence of metronidazole resistance has not been widely investigated [37].
Erythromycin and clindamycin were the most commonly used macrolides in dentistry. Clindamycin was the most common alternative in patient allergy to penicillin in some countries such as Canada and Spain, but the prescription rate showed marked variation even in one country (65% to 93.1% in Spain) [8,20,21,28]. In some countries such as Iran and Kuwait, erythromycin was the most common alternative in penicillin allergy (66.0% & 66.1%, respectively) [23,32]. The macrolides prescription for endodontic prophylaxis in most countries is in agreement with standard guidelines in dental treatments [28].
Tetracyclines were prescribed in a limited rate by dentists. Tetracyclines can be used in dental periodontic practice, however, their use is restricted due the emergence of documented adverse effects including esophageal ulcer [38]. Our search showed that the antibacterial drug categories such as, aminoglycosides, chloramphenicol, vancomycin, second, third and fourth generations of cephalosporines and quinolones were not prescribed by dentists, although, two reports showed the prescription of co-trimoxazole (2.2%) and ofloxacin (fluoroquinolone)/ornidazole combination (6%-13%) by paediatric dentists in Nigeria and India, respectively [19,32].
Amoxicillin, amoxicillin/clavulanic acid (augmentin) and metronidazole were the most commonly prescribed antimicrobials by dentists in patients without allergy to penicillins and clindamycin in patients with history of penicillin sensitivity [8,21,23]. Penicillin V, cloxacillin, cephalexin, erythromycin, azithromycin, tetracyclines and lincomycin are other antimicrobials less commonly prescribed by dentists [9,19,22].
Inappropriate use of antibiotics by dentists is reported from different countries. For example, almost half or more of dentists in Kuwait and South Australia prescribed antibiotics for non-indicated conditions in dental dry socket and dental localized swelling conditions [19,33]. Dentists must have the adequate knowledge for both therapeutic and prophylactic clinical indications of antibiotics, as well as a clear need for the development of prescribing guidelines to encourage the rational and appropriate use of the antibiotics in dental practice. Thus, educational programs concerning antibacterial drug therapy are needed for dentists to improve rational drug therapy and patient safety.
In the present study, ibuprofen was the most frequent NSAID drug prescribed by dentists, followed by naproxen and naprosin. Other non-opioid analgesics such as nimesulide, paracetamol, etodolac, diclofenac, flurbiprofen, and ketoprofen were prescribed in a few numbers of countries. There was a wide variation between the types of NSAIDs/analgesics drug used by dentists. For example, ibuprofen was the most frequently prescribed NSAIDs in Iran, Nepal and USA [11,12,35], but diclofenac and naproxen were the most frequently prescribed by dentists in India and Turkey, respectively [1,13]. Previous reports showed that ibuprofen was the most frequent NSAID drug prescribed by dentists followed by naproxen and nimesulide [11,12,35]. Diclofenac, etodolac, ketoprofen and flurbiprofen are other NSAIDs less frequently prescribed by dentists [13]. Acetaminophen alone or in combination with oxycodone and hydrocodone or propoxyphene was the other analgesic most frequently prescribed by dentists [11-13,24]. Codeine, oxycodone and hydrocodone and propoxyphene were the non-opioid analgesics prescribed either alone or in a combination with non-narcotic analgesics (mainly ibuprofen and acetaminophen) [11,24]. The reasons for the widespread use of ibuprofen by dentists is not determined yet and there is no documented data showing the superiority of ibuprofen over other NSAIDs. Further, clinical trial researches is needed to evaluate and compare the efficacy of different NSAIDs in management of dental related pain.
Tooth pain is the most common form of pain in the oral facial region. Previous studies reported that and 20% of patients suffer from moderate to severe post endodontic pain which needs medication about >7% of patients have all-cause persistent tooth pain after endodontic procedures [24]. NSAIDs, acetaminophen, and opioids are the main drugs used for medical management of tooth pain and the combination of opioids and non-opioid analgesics shows additive effects on pain management, since they produce analgesia by different mechanisms [11,12,24]. The combination of ibuprofen and acetaminophen with codeine for 3-7 days is the most common form of prescription for alleviation of dental pain, although, some clinician uses the combination of tramadol and acetaminophen in the management of acute postoperative dental pain [24,39].
Opioid drugs, mainly codeine, oxycodone and hydrocodone prescription by dentists is reported in limited studies [11,24]. However, other researchers confirmed the increase in the efficacy of analgesic effects and longer duration of action of mild opioid such as oxycodone or codeine in combination with acetaminophen for acute postoperative pain in adults [11,39]. Briefly, our results showed that amoxicillin alone or in combination with metronidazole, amoxicillin/clavulanic acid (augmentin), penicillin V, erythromycin & clindamycin are used most commonly for treatment of dental complications and ibuprofen is the most commonly used NSAIDs prescribed by dentists in different countries [2,7,17,26,28,30]. Dentists’ prescription pattern for NSAIDs and antibiotics is relatively, but not completely, in agreement with standard guidelines in dental practice.
Limitation
Our study had some limitations. Search terms and search strategy were selected in English language, so the results were directly biased to English language. Therefore, we missed some studies in other countries which were published in their original language. Also, we included the results of prescription patterns for both general dentists and specialist dentists (mainly endodontists), which affects the prescription pattern, so we suggested that prescription pattern of both groups of dentists should be evaluated separately in future studies. Further, due to restricted research on dentists’ prescription patterns, we had not set any specification for sampling procedure and study quality to obtain a full coverage of the documented topics. Our data did not include patients’ main diagnosis and complications for which drugs were prescribed. Moreover, the age of patients, which affects the prescription pattern, is not included in our study.
Conclusion
Our results showed that β-lactams antibiotics were the most frequently prescribed antibacterial drug category followed by metronidazole and macrolides. Amoxicillin and amoxicillin/clavulanic acid (augmentin) were the most frequently prescribed antibacterial in most countries. Clindamycin and erythromycin were prescribed for patients with a history of penicillin sensitivity. Ibuprofen was the most frequent NSAID drug prescribed by dentists followed by naproxen. Oxycodone, hydrocodone and codeine were the most common opioid drugs prescribed by dentists. The empirical use of amoxicillin/ clavulanic acid (augmentin) in some countries could be an evidence for inappropriate use of antibiotics in dentistry.
N= number of questionnaires or prescriptions of the related study.
N= number of questionnaires or prescriptions of the related study.
N= number of questionnaires or prescriptions of the related study.
*Vicodin® and Lortab®: Hydrocodone/acetaminophen, † Vicoprofen®: Hydrocodone/ibuprofen,
**APAP: Acetaminophen