Synchronous Neuroendocrine Tumour of Small Intestine in a Case of Squamous Cell Carcinoma Cervix–An Incidental Finding
Anamika Kashyap1, Shailaja Shukla2, Priyanka Banga3
1 Senior Resident, Department of Pathology, Lady Hardinge Medical College, New Delhi, Delhi India.
2 Director Professor, Department of Pathology, Lady Hardinge Medical College, New Delhi, Delhi, India.
3 Postgraduate Student, Department of Pathology, Lady Hardinge Medical College, New Delhi, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shailaja Shukla, Director Professor, Department of Pathology, Lady Hardinge Medical College, New Delhi-110001, Delhi, India.
E-mail: shukla_shailaja@yahoo.com
Multiple Primary Cancers (MPCs) are defined as two or more malignancies in a single individual without any relationship between cancers. Neuroendocrine carcinoma is a relatively rare tumour and its coexistence with other primary cancers is being increasingly recognised. Sometimes, the patients may present with the symptoms related to the other primary cancer (often described as second primary malignancy) which are usually more aggressive and the concurrent Neuroendocrine Tumour (NET) may be detected later. We present a case of a 60-year-old female presenting with haematuria due to bladder involvement by carcinoma cervix. The coexistence of small intestinal NET was co incidentally established. The second primary malignancy in NET can occur even many years later and can be multiple involving different organs. Therefore, patients with NET should be thoroughly evaluated with regular follow up.
Bladder, Malignancy, Multiple primary cancer
Case Report
A 60-year-old female presented with vaginal discharge and bleeding along with painless haematuria since three months. Gynaecological examination showed a 5 cm exophytic friable lesion arising from her cervix. Contrast Enhanced Computed Tomography (CECT) abdomen and Magnetic Resonance Imaging (MRI) pelvis were suggestive of carcinoma cervix extending to bladder with multiple locoregional lymph nodes. A clinical diagnosis of Stage IV cervical cancer was made. Urine cytology revealed few atypical cells [Table/Fig-1a]. A diagnosis of keratinising squamous cell carcinoma cervix was given on Papanicolaou (Pap) smear and cervical biopsy. A radical hysterectomy along with cystoureterectomy was performed. A small bowel nodule was noticed per operatively at a distance of 3 cm proximal to ileocaecal junction and was thus removed.
a) Urine cytology showing atypical cell (marked with arrow) (Pap stain 10X); b) Squamous cell carcinoma cervix (H&E stain 10X); c) Squamous cell carcinoma cervix (H&E stain 40X); d) Neuroendocrine tumour (H&E stain 40X); e) Immunohistochemistry showing NSE positivity in neuroendocrine tumour (H&E stain 10X).
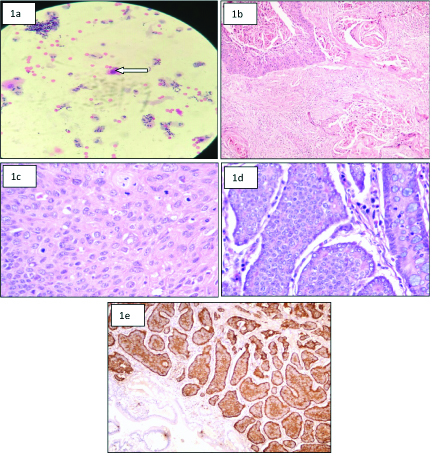
Gross examination showed a distorted friable diffusely infiltrative cervical growth of 5×3×4 cm involving the cervix and body of uterus and infiltrating into posterior wall of urinary bladder. Small bowel segment measuring 1 cm in length showed a 0.5 cm yellow sub-mucosal tumour nodule within the wall. Histopathology of cervix and bladder showed keratinising squamous cell carcinoma cervix with extension into urinary bladder [Table/Fig-1b,c]. Bilateral adnexa and all iliac lymph nodes were found to be free of tumour. Small intestine nodule on histopathology showed nest of tumour cells limited to submucosa with mitoses 1-2/10 High Power Field (HPF) and no necrosis). These cells on immunohistochemistry showed positivity for Neuron Specific Enolase (NSE) and chromogranin [Table/Fig-1d,e]. Final diagnosis of Stage IV keratinising squamous cell carcinoma of cervix involving urinary bladder with synchronous well differentiated low grade NET of small intestine was given. Patient was not willing for chemotherapy and lost to follow up after surgery.
Discussion
Multiple primary cancer are defined as two or more malignancies in a single individual without any relationship between these cancers. In the literature, the prevalence of MPC is estimated between 0.73% and 11.7% and the incidence is increasing with age [1]. The incidence of multiple cancers have progressively increased over time possibly due to greater awareness, improved diagnostic techniques and facilities. Causal mechanisms of MPC are caused by multiple factors including genetic factors, environmental factors, therapeutic effects and various combinations of these three factors. MPC is classified into two categories: 1) synchronous cancers diagnosed together or at an interval of two months; 2) metachronous cancers diagnosed one after another at an interval more than two months apart [2]. However, many authors take six months as the cut-off time period [3]. Pearson CM and Fitzgerald PJ reported that there is an increased incidence of carcinoid tumours with secondary primary malignancies [4].
The NET of digestive tract has been associated with Second Primary Malignancies (SPMs) like carcinomas of colorectum, breast, genitourinary tract and melanoma.
Three diagnostic criteria are used for diagnosing MPCs: 1) each tumour must have features which are definite of that malignancy; 2) each tumour must be distinct from each other; and 3) one tumour must not be a metastasis of the other. MPCs are classified into four types according to location: 1) multicentric, if the two tumours present in same organ; 2) systemic, if they are present in organs of the same system; 3) paired organs; and 4) random, if they occur at unrelated sites [5,6]. The present case fulfilled all the three diagnostic criteria of MPC and with a rarely occurring random detection of synchronous carcinoid tumour in a cervical carcinoma case.
Among the MPC, NETs associated with other primary cancers are commonly found. Approximately, 55% NETs are associated with synchronous or metachronous secondary primary malignancies [7]. It has been hypothesised that a common carcinogenic effect may stimulate the growth of NET associated SPM. Also, NETs produce and secrete various neuropeptides or non-neuropeptides which have specific growth factor properties [8]. Most SPM present concurrently with NET and are usually more aggressive. Many patients may present with symptoms related to the SPM and not the NET which is often detected as an incidental finding. In the present case also, the medical history was significant only for carcinoma cervix involving the urinary bladder. The patient had no hormone related symptoms and the NET was accidently detected during surgery.
This case highlighted the rarity of the synchronous, random occurrence of cervical cancer with NET warranting the need for extensive sampling of any suspicious area and a thorough histopathological examination even in patients who do not present with symptoms related to the organ under suspicion.
Conclusion
Patients of any malignancy with synchronous NET present with symptoms of the primary malignancy but have an aggressive course. Thus, a thorough evaluation of all primary cases is important to predict the prognosis and provide appropriate treatment to such patients.
[1]. Spratt JR, Hoag MG, Incidence of multiple primary cancers per man year of follow up: 20-year review from the Ellis Fischel State Cancer HospitalAnn Surg 1966 164:775-84.10.1097/00000658-196611000-000015923101 [Google Scholar] [CrossRef] [PubMed]
[2]. Howe HL, A review of the definition for multiple primary cancers in the United StatesWorkshop Proceedings from December 4-6, 2002, in Princeton, New Jersey Springfield (IL): North American Association of Central Cancer Registries 2003 [Google Scholar]
[3]. Sakellakis M, Peroukides S, Iconomou G, Boumpoucheropoulos S, Kalofonos H, Multiple primary malignancies: report of two casesChin J Cancer Res 2014 26:215-18. [Google Scholar]
[4]. Pearson CM, Fitzgerald PJ, Carcinoid tumours-a reemphasis of their malignant nature. Review of 140 casesCancer 1949 2(6):1005-26.10.1002/1097-0142(194911)2:6<1005::AID-CNCR2820020608=3.0.CO;2-1 [Google Scholar] [CrossRef]
[5]. Aydiner A, Karadeniz A, Uygun K, Tas S, Tas F, Disci R, Multiple primary neoplasms at a single institution: differences between synchronous and metachronous neoplasmsAm J Clin Oncol 2000 23:364-70.10.1097/00000421-200008000-0001110955865 [Google Scholar] [CrossRef] [PubMed]
[6]. Derwinger K, Gustavsson B, A study of aspects on gender and prognosis in synchronous colorectal cancerClin Med Insights Oncol 2011 5:259-64.10.4137/CMO.S787121912492 [Google Scholar] [CrossRef] [PubMed]
[7]. Habal N, Sims C, Bilchik AJ, Gastrointestinal carcinoid tumours and second primary malignanciesJ Surg Oncol 2000 75:301-06.10.1002/1096-9098(200012)75:4<306::AID-JSO14>3.0.CO;2-3 [Google Scholar] [CrossRef]
[8]. Oberg K, Expression of growth factors and their receptors in neuroendocrine gut and pancreatic tumours, and prognostic factors for survivalAnn NY Acad Sci 1994 733:46-55.10.1111/j.1749-6632.1994.tb17255.x7978895 [Google Scholar] [CrossRef] [PubMed]