Introduction
Knee pain is a leading cause of disability and the most prevalent form in the world. It is associated with tissue inflammation, physical disability and imbalanced homeostasis in cartilage. As the number of people with age greater than 35 years increases, so does the prevalence of knee pain and the need for cost effective treatment and care. A treatment strategy is needed which takes into account the underlying physiology of degenerative joint disease, but it should also consider the different age ranges and their needs in different population.
Aim
To assess the clinical and functional benefits associated with the use of intra-articular Platelet Rich Plasma (PRP) in treatment of patients with knee pain of primary Osteoarthritis (OA).
Materials and Methods
A prospective observational study of 50 patients visiting the outpatient department from 1st January 2013 to 31st December 2015 with Kellgren and Lawrence Grade 1 and 2 OA knees were evaluated with the Western Ontario and McMaster Universities Arthritis Index (WOMAC) before the treatment and at 1, 3 and 9 months after the PRP intra-articular treatment.
Results
Statistically significant improvements in WOMAC scores were noted in all the evaluated measures in all patients.
Conclusion
A minimum of two intra-articular injections of PRP is an effective treatment for mild to moderate osteoarthritis of knees.
Introduction
Platelet-rich plasma is an autologous concentration of a higher number of platelets in a small volume of plasma compared to whole blood, prepared by centrifugation of whole blood. Platelets contain various amount of cytokines and growth factors which have the capacity of stimulating cellular growth, vascularisation, proliferation, tissue regeneration, and collagen synthesis. PRP delivers high concentrations of cytokines and growth factors to damaged tissues and is considered to have a regeneration effect on tendon and cartilage tissue [1,2]. Chronic knee pain puts a person to inconvenience in social, familial and business environments. Knee pain can occur in numerous ways and due to various diseases. Between the ages of 30 and 65 years, the general incidence and prevalence of knee OA has been reported to increase by as much as 10 times that of younger age groups, affecting nearly 33.6% of people >65 years or an incidence of 1 in 10 [3,4]. Since PRP contains growth factors and plasma proteins, it can regulate anti inflammatory signals and equilibrate angiogenesis [4,5]. Based on this, its use in order to reduce the progression of knee pain has been suggested in a study [6]. In OA knee, PRP injections delay the need for joint replacement surgery by promoting cartilage repair thus relieving osteoarthritic symptoms [7]. PRP is prepared from the patient’s own blood, so there is no risk of developing a tumour or donor blood transfusion infections like HIV, HBsAg, HCV etc., [8]. Adverse effects can occur as with any injection like small risk of infection or local injury to nerves or blood vessels, scar tissue formation and calcification at the injection site [9]. The conservative treatment options for osteoarthritic knee pain are: Non Steroidal Anti Inflammatory Drugs (NSAIDs) including non selective Cyclooxygenase (COX) inhibitors and selective COX-2 inhibitors (Coxibs), steroids, chondroitin sulfate, diancerein, glucosamine sulfate etc. Intra-articular therapies with injectable steroids, hyaluronic acid, viscous gel etc., also aid in temporary pain relief.
The aim of the present study was to assess the clinical and functional benefits associated with the use of intra-articular PRP in treatment of patients with knee pain due to primary OA.
Materials and Methods
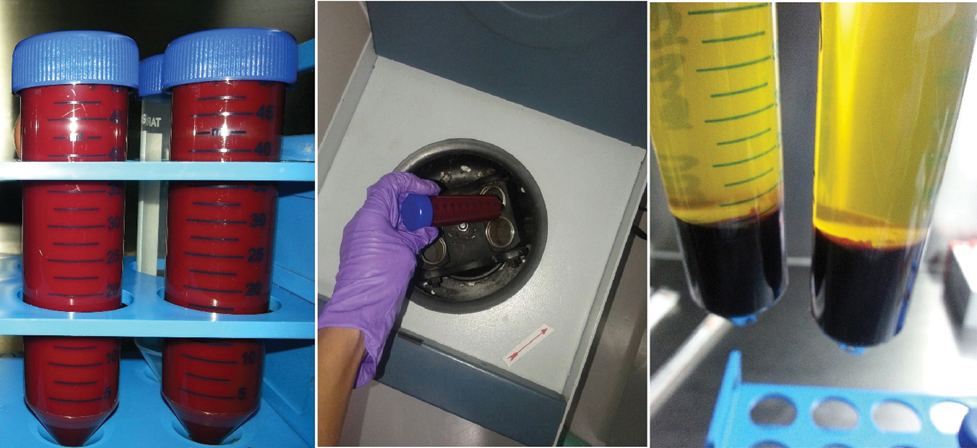
This was a prospective observational study done from January 1st 2014 to December 31st 2015. All patients presenting to orthopaedics outpatient department of Health Care Global (HCG) hospital, Bengaluru, Karnataka, India, with Kellgren and Lawrence Grade 1 and 2 OA knees were considered. All patients fulfilling the inclusion and exclusion criteria and consenting to participate in the study were enrolled. At the end of two years, 50 patients were enrolled and completed all 3 follow up WOMAC questionnaires by physical presence or telephone contact. PRP was prepared using buffy coat method, where 50 mL Whole Blood (WB) was mixed with anticoagulant citrate dextrose and centrifuged at a ‘hard spin’ of 4000 rpm for 15 minutes. A supernatant buffy coat is formed and contains leucocytes rich at upper and PRP in middle layer. This layer mainly comprises of the necessary PRP [10,11]. The difficulty lies in separating this thin buffy coat from the underlying RBC layer. To obtain PRP by buffy coat method WB was mixed with anticoagulant and stored at 20°C to 24°C before centrifugation [Table/Fig-1] and then centrifuged at a ‘high’ speed of 4000 rpm. Three layers were formed because of its density. The bottom layer consists of RBCs, the middle layer consists of PRP and the topmost layer consists of leucocyte rich with platelet poor plasma. Supernatant plasma was removed from the top of the container and this buffy coat layer was transferred to another sterile tube. This was centrifuged at a low speed of 1000 rpm (soft spin) to separate WBCs and obtain PRP [12].
Showing collection of patient’s own blood in 50 mL tube, centrifuging them and obtaining about 10 mL PRP in the lower layer.
Inclusion criteria had patients aged >40 years, both male and female, painful arthritic knees of Kellgren and Lawrence Grade 1 and 2, platelet count >150,000/cumm [13] and patients willing for intra-articular autologous PRP injection and attend to a follow up of minimum 3 visits post procedure at 1, 3 and 9 months respectively. Patients with cancer or metastatic disease, an active local or systemic infection, pregnant or is breastfeeding [14], uncontrolled diabetes mellitus, peripheral vascular disease, inflammatory arthritis, traumatic arthritis, metabolic arthritis (gout) etc., were excluded from the study along with patients willing for total knee arthroplasty.
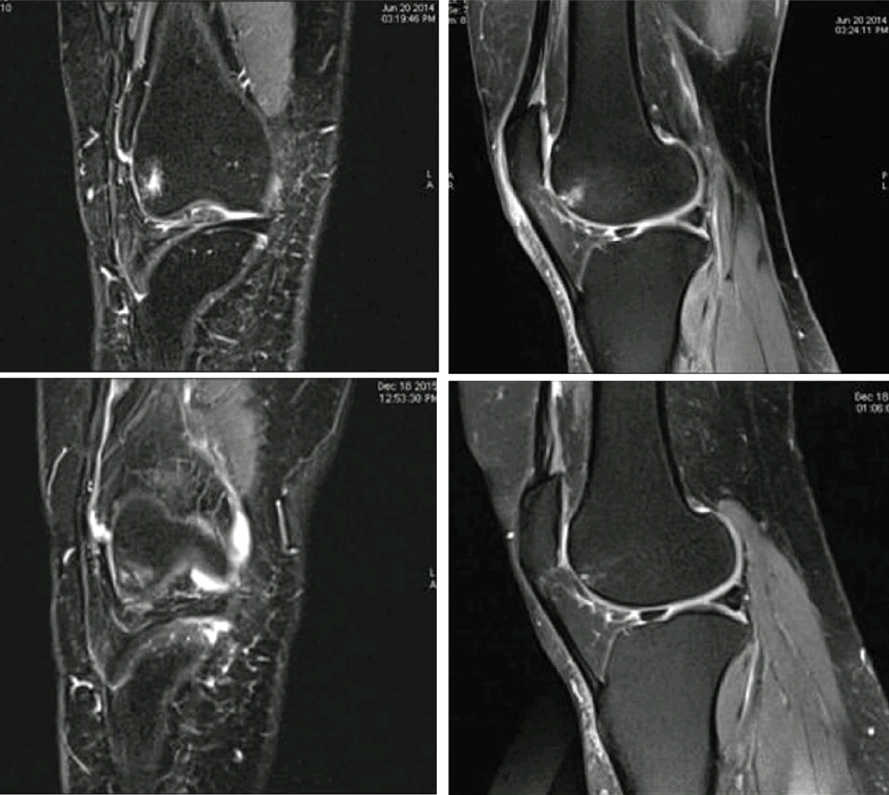
The WOMAC pain index is a disease-specific questionnaire for the disease, which assesses pain, stiffness and physical functions of patients. After receiving the approval for study from our hospital’s Ethics Committee, the aims and methods of PRP therapy as well as the benefits and the possible adverse effects of study were presented to the patients. Then, for each patient, WOMAC questionnaire for evaluation of patients’ pain, stiffness and physical functions was recorded and evaluated. Patients were evaluated before the PRP treatment and after the treatment at 1 month, 3 months and 9 months with WOMAC questionnaire. Under strict aseptic precautions about 6 mL of the autologous PRP preparation was injected intra-articular with a 21 gauge hypodermic needle behind the patella after synovial fluid aspiration in the affected knee [Table/Fig-2]. Acetaminophen was given for pain relief and physiotherapy started from next day with quadriceps and hamstrings strengthening exercises. Similarly another dose of PRP injection was given after a week interval. Longest follow up was of 18 months, which had also MRI knee imaging done pre and post PRP intervention. T2W images showed increased thickness of articular cartilage in both coronal and sagittal images [Table/Fig-3].
Showing the autologous derived PRP being given intra-articular into the knee under sterile aseptic conditions.

Showing MRI of knee in coronal and sagittal views; before intra-articular PRP injection in the upper row and 18 months post PRP injection in the lower row showing a comparatively thickened articular cartilage.
Statistical Analysis
Statistical analysis was done using unpaired t-test for the WOMAC values obtained pre and post PRP injection.
Results
A total of 50 patients with mild to moderate OA knees were involved in the study and completed a minimum of 9 months post PRP injection follow up. Gender wise 28 females and 22 males were involved making a percentage of 56% and 44% respectively. Two patients developed superficial tenderness at injection site which healed within a week by analgesics alone. WOMAC scores compared individually for pain, stiffness and physical function at 1st, 3rd and 9 months post PRP injection versus pre-injection [Table/Fig-4] showed statistical significance with p-value less than 0.001 for almost all except for pain at 1st month (p=0.2408) as shown in the [Table/Fig-5].
Showing WOMAC scores compared individually for pain, stiffness and physical function before PRP injection versus post PRP intra-articular injection after 1, 3 and 9 months.
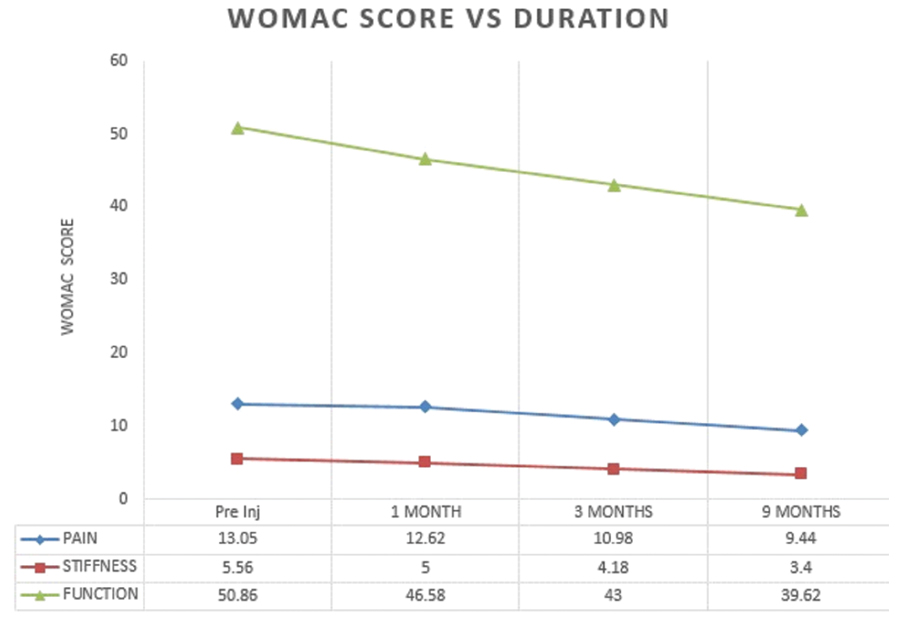
Showing WOMAC scores mean, standard deviation (SD), and p-value of pre and post PRP injection at 1, 3 and 9 months follow up.
| WOMAC scores | mean | Standard deviation (SD) | p-value (Pre Vs post inj.) |
|---|
| Pain pre PRP injection | 13.05 | 1.94 | - |
| Pain post PRP at 1 month | 12.62 | 1.78 | 0.2408 |
| Pain post PRP at 3 months | 10.98 | 1.76 | <0.001 |
| Pain post PRP at 9 months | 9.64 | 2.26 | <0.001 |
| Stiffness pre PRP injection | 5.56 | 0.70 | - |
| Stiffness post PRP at 1 month | 5.00 | 0.83 | 0.0005 |
| Stiffness post PRP at 3 months | 4.18 | 0.87 | <0.001 |
| Stiffness post PRP at 9 months | 3.40 | 1.11 | <0.001 |
| Physical function pre PRP injection | 50.86 | 5.01 | - |
| Physical function post PRP at 1 month | 46.58 | 5.10 | <0.001 |
| Physical function post PRP at 3 months | 43.00 | 6.52 | <0.001 |
| Physical function post PRP at 9 months | 39.62 | 8.27 | <0.001 |
WOMAC- Western Ontario and McMaster Universities Arthritis Index; PRP, Platelet rich plasma.
Discussion
In our study PRP showed beneficial effects in arthritic knees by decreased pain and stiffness and improving the physical function. Since the past decade, PRP has evolved as a non operative treatment modality for cartilage injuries [15]. Even though there are significant variations in its makeup, the initial PRP prepared by centrifugation consistently contains highly concentrated platelets and a number of plasma proteins. Platelets are produced by their precursor megakaryocytes as anucleated cells [16]. Different types of growth factors, adhesion molecules, coagulation factors, cytokines, chemokines and integrins are stored in platelets [17]. The platelets in PRP after activation release different growth factors at concentrations significantly higher than the baseline blood levels, which includes transforming growth factor-β, Platelet-Derived Growth Factor (PDGF), Insulin-like Growth Factor (IGF), basic fibroblast growth factors, Vascular Endothelial Growth Factor (VEGF), epidermal growth factors etc., [18]. Many of these are anabolic cytokines like transforming growth factor-β, IGF, basic fibroblast growth factor and PDGF, are chondroprotective and chondro-promoting [19]. These stimulate chondrocyte and multipotent Mesenchymal Stem Cell (MSC) proliferation, promote chondrocyte synthesis of aggrecan and Collagen type II (Co lII), drive MSC chondrogenic differentiation, prevent chondrocyte and MSC apoptosis, and diminish the catabolic effects of inflammatory cytokines, such as IL-1β, and Matrixmetallo Proteinases (MMPs). PRP platelets are also a source of inflammatory mediators and modulators. Platelets after incubation with polyacrylamide beads, may release numerous anti inflammatory cytokines, including IL-1 receptor antagonist (IL-1ra), soluble Tumour Necrosis Factor (TNF) Receptor (sTNF-R) I and II, IL-4, IL-10, IL-13, and interferon γ [20]. The significant difference between the concentrations of pro inflammatory factors and anti inflammatory cytokines in PRP suggests that PRP may suppress inflammation in OA knee pains, thereby protecting cartilage and reducing pain. PRP contains various plasma proteins, which form critical components in connective tissues healing mechanism [21]. Compared to serum, plasma contains fibrinogen and other clotting factors, which can be activated to form a provisional fibrin scaffold for cells to migrate, adhere and proliferate [22]. As articular cartilage is avascular and thus unable to initiate the same healing process as other tissues, PRP scaffold mimic the initial stage of wound healing and tissue repair. Dohan Ehrenfest DM et al., suggested the following classification for PRP: leukocyte poor PRP; platelet and leukocyte rich plasma; platelet rich and leukocyte poor fibrin; and platelet and leukocyte rich fibrin [23]. One study has showed the efficacy of PRP to improve functional outcomes for mild knee osteoarthritis [24]. Various RCTs have demonstrated the superiority of PRP over traditional approaches and have also demonstrated superiority of autologous PRP intra-articular injections over hyaluronic acid injections in reducing pain and recovering articular function [25,26], especially for younger patients and milder OA knees [27,28] with one study showing benefit of PRP even for Grade 3 knee OA [29]. Others have shown inconsistent superiority of PRP over viscosupplementation [30]. In an RCT with 1-year follow up, PRP was not superior to viscosupplementation for knee OA, with diminishing benefit beyond 9 months [31]. A study showed no difference for pain and functional outcome after having a single or a double injection of PRP, but both provided superior outcomes compared with control using saline [32]. Another study demonstrated superiority of PRP compared with viscosupplementation only when multiple PRP injections were used [28]. PRP was shown to be superior to steroid injection for knee OA [33]. Adverse effects have been minor, with leukocyte-rich PRP associated with increased pain and swelling relative to leukocyte-poor PRP [34].
Limitation
Though it is an observational study, a control group could have been used with a placebo or oral analgesics or intra-articular viscosupplementation or steroids etc. Sample size of 50 was also small to conclude the benefits of any medical intervention. MRI for cartilage thickness measurement was not done for most of the patients due to technical reasons. PRP is still under research process and FDA approval is still awaited but previous studies have stated that they can be used even without approval as it is an autologous substance.
Conclusion
PRP acts as one of the best non drug modalities of treatment and may delay the need for total knee arthroplasty. Thus, combining PRP (of which a minimum of two injections was appropriate), Hyaluronic Acid (HA) and stem cells would be an ideal combination for treatment of knee pain. Although, this is a promising method of treatment for knee pain, its long-term outcome is unknown and can’t be used in advanced osteoarthritis.
WOMAC- Western Ontario and McMaster Universities Arthritis Index; PRP, Platelet rich plasma.
[1]. Dragoo JL, Wasterlain AS, Braun HJ, Nead KT, Platelet-rich plasma as a treatment for patellar tendinopathy: a double-blind, randomized controlled trialAm J Sports Med 2014 42:610-18.10.1177/036354651351841624481828 [Google Scholar] [CrossRef] [PubMed]
[2]. Smyth NA, Murawski CD, Fortier LA, Cole BJ, Kennedy JG, Platelet-rich plasma in the pathologic processes of cartilage: review of basic science evidenceArthroscopy 2013 29:1399-409.10.1016/j.arthro.2013.03.00423669235 [Google Scholar] [CrossRef] [PubMed]
[3]. Ringdahl E, Pandit S, Treatment of knee osteoarthritisAm Fam Physician 2011 83:1287-92. [Google Scholar]
[4]. Magrans-Courtney T, Wilborn C, Rasmussen C, Ferreira M, Greenwood L, Campbell B, Effects of diet type and supplementation of glucosamine, chondroitin, and MSM on body composition, functional status, and markers of health in women with knee osteoarthritis initiating a resistance-based exercise and weight loss programJ Int Soc Sports Nutr 2011 8:8/10.1186/1550-2783-8-821689421 [Google Scholar] [CrossRef] [PubMed]
[5]. Raeissadat SA, Sedighipour L, Rayegani SM, Bahrami MH, Bayat M, Rahimi R, Effect of Platelet-Rich Plasma (PRP) versus autologous whole blood on pain and function improvement in tennis elbow: a randomized clinical trialPain Research and Treatment 2014 2014:19152510.1155/2014/191525 [Google Scholar] [CrossRef]
[6]. Civinini R, Nistri L, Martini C, Redl B, Ristori G, Innocenti M, Growth factors in the treatment of early osteoarthritisClin Cases Min Bone Metab 2013 10:2610.11138/ccmbm/2013.10.1.02623858307 [Google Scholar] [CrossRef] [PubMed]
[7]. Anitua E, Sánchez M, Orive G, Padilla S, A biological therapy to osteoarthritis treatment using platelet-rich plasmaExpert Opin Biol Ther 2013 :1-12.10.1517/14712598.2013.80145023834251 [Google Scholar] [CrossRef] [PubMed]
[8]. Interventional procedure overview of platelet-rich plasma injections for osteoarthritis of the knee. NICE Interventional Procedure Guidance. [Available from http://www.guidance.nice.org.uk] [Google Scholar]
[9]. Everts P, Knape J, Weirich G, Schonberger J, Hoffman J, Overdevest E, Platelet-rich plasma and platelet gel: a reviewJECT 2006 38:174-87. [Google Scholar]
[10]. Sampson S, Gerhardt M, Mandelbaum B, Platelet rich plasma injection grafts for musculoskeletal injuries: a reviewCurr Rev Musculoskelet Med 2008 1(3-4):165-74.10.1007/s12178-008-9032-519468902 [Google Scholar] [CrossRef] [PubMed]
[11]. Sampson S, Reed M, Silvers H, Meng M, Mandelbaum B, Injection of platelet-rich plasma in patients with primary and secondary knee osteoarthritis: a pilot studyAm J Phys Med Rehabil 2010 89(12):961-69.10.1097/PHM.0b013e3181fc7edf21403592 [Google Scholar] [CrossRef] [PubMed]
[12]. Scherer SS, Tobalem M, Vigato E, Heit Y, Modarressi A, Hinz B, Non-activated versus thrombin-activated platelets on wound healing and fibroblast-to-myofibroblast differentiation in vivo and in vitroPlast Reconstr Surg 2012 129:46e-54e.10.1097/PRS.0b013e318236201022186584 [Google Scholar] [CrossRef] [PubMed]
[13]. Sarzi-Puttini P, Cimmino MA, Scarpa R, Caporali R, Parazzini F, Zaninelli A, Osteoarthritis: an overview of the disease and its treatment strategiesSemin Arthritis Rheum 2005 35(1 Suppl 1):01-10.10.1016/j.semarthrit.2005.01.01316084227 [Google Scholar] [CrossRef] [PubMed]
[14]. Phillips S, Silvia Li C, Phillips M, Bischoff M, Ali P, Chahal J, Treatment of osteoarthritis of the knee with bracing: a scoping reviewOrthopedic Reviews 2016 8(2):625610.4081/or.2016.625627433297 [Google Scholar] [CrossRef] [PubMed]
[15]. Fortier LA, Hackett CH, Cole BJ, The effects of platelet-rich plasma on cartilage: basic science and clinical applicationOper Tech Sports Med 2011 16:154-59.10.1053/j.otsm.2011.03.004 [Google Scholar] [CrossRef]
[16]. Italiano JE Jr, Shivdasani RA, Megakaryocytes and beyond: the birth of plateletsJ Thromb Haemost 2003 16:1174-82.10.1046/j.1538-7836.2003.00290.x12871316 [Google Scholar] [CrossRef] [PubMed]
[17]. Macaulay IC, Carr P, Gusnanto A, Ouwehand WH, Fitzgerald D, Watkins NA, Platelet genomics and proteomics in human health and diseaseJ Clin Invest 2005 16:3370-77.10.1172/JCI2688516322782 [Google Scholar] [CrossRef] [PubMed]
[18]. Nurden AT, Nurden P, Sanchez M, Andia I, Anitua E, Platelets and wound healingFront Biosci 2008 16:3532-48.10.2741/2947 [Google Scholar] [CrossRef]
[19]. Brandl A, Angele P, Roll C, Prantl L, Kujat R, Kinner B, Influence of the growth factors PDGF-BB, TGF-beta1 and bFGF on the replicative aging of human articular chondrocytes during in vitro expansionJ Orthop Res 2010 16:354-60.10.1002/jor.2100719798738 [Google Scholar] [CrossRef] [PubMed]
[20]. Woodell-May J, Matuska A, Oyster M, Welch Z, O’Shaughnessey K, Hoeppner J, Autologous protein solution inhibits MMP-13 production by IL-1beta and TNF alpha-stimulated human articular chondrocytesJ Orthop Res 2011 16:1320-26.10.1002/jor.2138421437966 [Google Scholar] [CrossRef] [PubMed]
[21]. Mann KG, Biochemistry and physiology of blood coagulationThromb Haemost 1999 16:165-74.10.1055/s-0037-1615780 [Google Scholar] [CrossRef]
[22]. Xie X, Wang Y, Zhao C, Guo S, Liu S, Jia W, Comparative evaluation of MSCs from bone marrow and adipose tissue seeded in PRP-derived scaffold for cartilage regenerationBiomaterials 2012 16:7008-18.10.1016/j.biomaterials.2012.06.05822818985 [Google Scholar] [CrossRef] [PubMed]
[23]. Dohan Ehrenfest DM, Rasmusson L, Albrektsson T, Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF)Trends Biotechnol 2009 27(3):158-67.10.1016/j.tibtech.2008.11.00919187989 [Google Scholar] [CrossRef] [PubMed]
[24]. Kon E, Buda R, Filardo G, Di Martino A, Timoncini A, Cenacchi A, Platelet-rich plasma: intra-articular knee injections produced favorable results on degenerative cartilage lesionsKnee Surg Sports Traumatol Arthrosc 2010 18:472-79.10.1007/s00167-009-0940-819838676 [Google Scholar] [CrossRef] [PubMed]
[25]. Vaquerizo V, Plasencia MA, Arribas I, Seijas R, Padilla S, Orive G, Comparison of intra-articular injections of plasma rich in growth factors (PRGF-Endoret) versus Durolane hyaluronic acid in the treatment of patients with symptomatic osteoarthritis: a randomized controlled trialArthroscopy 2013 29:1635-43.10.1016/j.arthro.2013.07.26424075613 [Google Scholar] [CrossRef] [PubMed]
[26]. Spaková T, Rosocha J, Lacko M, Harvanova D, Gharaibeh A, Treatment of knee joint osteoarthritis with autologous platelet-rich plasma in comparison with hyaluronic acidAm J Phys Med Rehabil 2012 91:411-17.10.1097/PHM.0b013e3182aab7222513879 [Google Scholar] [CrossRef] [PubMed]
[27]. Sánchez M, Fiz N, Azofra J, Usabiaga J, Aduriz Recalde E, Garcia Gutierrez A, A randomized clinical trial evaluating plasma rich in growth factors (PRGF-Endoret) versus hyaluronic acid in the short-term treatment of symptomatic knee osteoarthritisArthroscopy 2012 28:1070-78.10.1016/j.arthro.2012.05.01122840987 [Google Scholar] [CrossRef] [PubMed]
[28]. Gormeli G, Gormeli CA, Ataoglu B, Colak C, Aslanturk O, Ertem K, Multiple PRP injections are more effective than single injections and hyaluronic acid in knees with early osteoarthritis: a randomized, double-blind, placebo-controlled trialKnee Surg Sports Traumatol Arthrosc 2017 25:958[Available from https://doi.org/10.1007/s00167-015-3705-06.]10.1007/s00167-015-3705-626233594 [Google Scholar] [CrossRef] [PubMed]
[29]. Cerza F, Carni S, Carcangiu A, Di Vavo I, Schiavilla V, Pecora A, Comparison between hyaluronic acid and platelet-rich plasma, intra-articular infiltration in the treatment of gonarthrosisAm J Sports Med 2012 40:2822-27.10.1177/036354651246190223104611 [Google Scholar] [CrossRef] [PubMed]
[30]. Raeissadat SA, Sedighipour L, Rayegani SM, Bahrami MH, Bayat M, Rahimi R, The effect of platelet-rich plasma on pain, function, and quality of life of patients with knee osteoarthritisPain Res Treat 2013 2013:165967 [Google Scholar]
[31]. Filardo G, Di Matteo B, Di Martino A, Merli ML, Cenacchi A, Fornasari P, Platelet-rich plasma intra-articular knee injections show no superiority versus viscosupplementation: a randomized controlled trialAm J Sports Med 2015 43(7):1575-82.10.1177/0363546515582027 [Google Scholar] [CrossRef]
[32]. Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A, Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trialAm J Sports Med 2013 41:356-64.10.1177/036354651247129923299850 [Google Scholar] [CrossRef] [PubMed]
[33]. Forogh B, Mianehsaz E, Shoaee S, Ahadi T, Raissi GR, Sajadi S, Effect of single injection of platelet-rich plasma in comparison with corticosteroid on knee osteoarthritis: a double-blind randomized clinical trialJ Sports Med Phys Fitness 2016 56(7-8):901-08. [Google Scholar]
[34]. Filardo G, Kon E, Pereira Ruiz MT, Vaccaro F, Guitaldi R, Di Martino A, Platelet-rich plasma intra-articular injections for cartilage degeneration and osteoarthritis: single- versus double-spinning approachKnee Surg Sports Traumatol Arthrosc 2012 20:2082-91.10.1007/s00167-011-1837-x22203046 [Google Scholar] [CrossRef] [PubMed]