Owing to advances in microsurgical techniques and anatomical studies on perforators, it is widely accepted that septocutaneous and direct cutaneous perforators can prove to be quite useful for a variety of flap options in conventional donor regions. Understanding of anatomic territories of individual perforator supplying skin and their crucial role in flap design and survival has thus become the need of hour. Though many studies have been conducted in the past related to perforators of various regions [1-2], still medial arm region is least explored with regard to its vascularity and anatomical details. Small defects of hand and forearm can usually be managed by local flaps. However, for larger defects, alternate donor site needs to be explored. Such a flap, should have some important properties like cosmetically acceptable, easy to nurse and must not hamper the daily routine of the patient. Medial arm perforator can serve as best option during flap surgeries with desired qualities of hidden scar and cosmetically acceptable [3-5].
Perignon D et al., also suggested medial arm flap to be ideal choice for elbow and head and neck surgeries [6]. Major advantage of using medial arm region flap in local reconstructive surgeries is that it does not sacrifice the major vessel. Its main requirement is pedicle of suitable length and diameter. However, the anatomical details of the medial arm perforators like their main source vessel, its location, its branching pattern, course and number of perforators varies from one individual to another. Due to these reasons, medial arm region is not very popular among surgeons for flap surgeries. In this article, the role of cadaveric study have been highlighted for better understanding of vascular anatomy of medial arm region. It was aimed to provide the reliable data regarding vascular supply of medial arm region along with relevant morphometric data regarding vessels, their branches and perforators supplying medial arm region.
Materials and Methods
Present cadaveric study was conducted in Department of Anatomy, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh in collaboration with Department of Plastic and Reconstructive surgery, PGIMER, Chandigarh, India. Duration of study was January 2015–December 2015. 30 upper limbs of 15 fresh adult cadavers (11 males, 4 females) with mean age of 79±3 years were studied. All these cadavers were donated to department of Anatomy, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh. Cadavers with any visible limb deformity or any kind of pathology were excluded from the study.
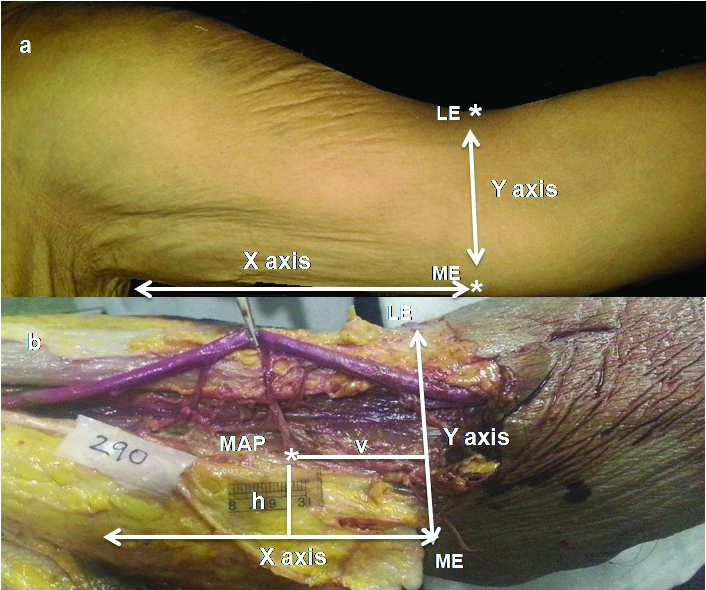
During dissection of upper limb, the arm was placed at 90° abduction and laterally rotated. Through a minimal axilla incision, axillary artery was located and injected with colored latex dye (10–15 mL) with the help of feeding tube. Dye was injected slowly, so as to avoid any vascular injury. Dissections were performed 24 hours after inserting the dye. The approach was a longitudinal incision over the lateral aspect of arm, across a vertical line perpendicular to medial epicondyle, extending along the long axis of arm upto the point midway between anterior and posterior pillar of axilla (X axis). Horizontally line extended between the medial and lateral epicondyles (Y axis). Dissections were performed in suprafascial plane from lateral to medial aspect. Then the individual perforators were identified, their location was projected over the skin with the help of a needle and traced on the transparent sheet. Distance of each perforator from X and Y axis was recorded. Then each individual perforator was followed upto its source vessel [Table/Fig-1].
Medial surface of arm was marked with X axis (vertical line perpendicular to medial epicondyle, along the long axis of arm) and Y axis (a horizontal line extending between the medial and lateral epicondyles), prior to dissection. The location of each perforator was marked by taking vertical (v) and horizontal (h), along these two axis. b) In this figure, location of perforator was traced along X axis and Y axis. The medial arm perforator (MAP) is seen lying along the lower one third of medial region of arm. This perforator is of suitable type (diameter 0.5 mm–1 mm). It is lying obliquely to the brachial artery (BA). (ME-Medial Epicondyle, LE-Lateral Epicondyle)
Following parameters were observed: total number of perforators, source vessel, dimensions and distribution of perforators, direction and branching pattern of perforators and distance of perforators from standard bony landmarks.
Results
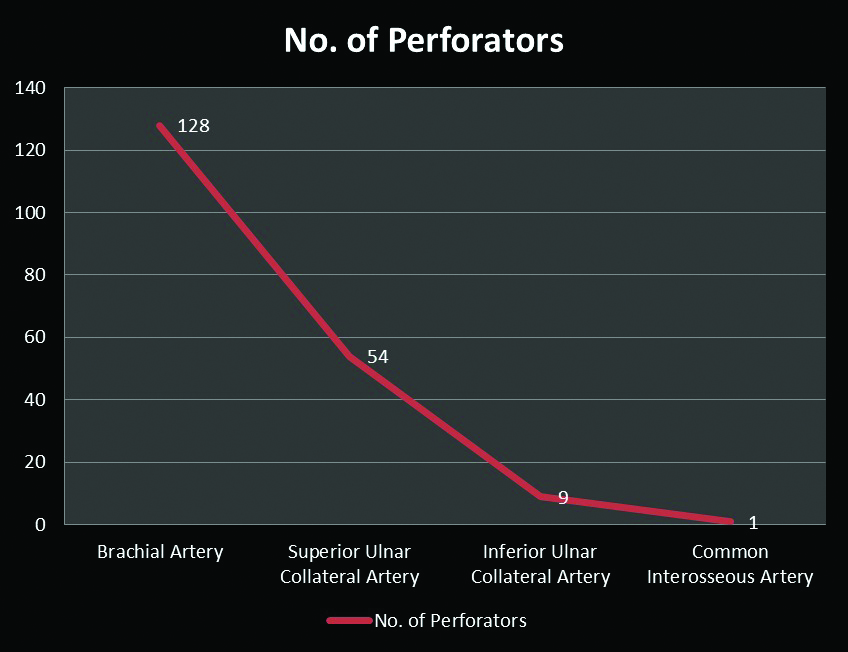
Total number of perforators were observed to be 192 [Table/Fig-2,3]. In majority of the cases, brachial artery began at the level of lower border of teres major muscle and was seen lying posteromedial to the brachial vein. However, in one case, it was seen lying superficial to the brachial vein. Branches arising from brachial artery were profunda brachii artery, muscular branches and superior and inferior ulnar collateral artery. However, in two cases, brachial artery gave rise to a very large superficial branch called superficial ulnar artery, which coursed superficially along arm and passed superficial to the medial epicondyle to enter forearm. In one of the cases, common interosseous artery was seen arising from brachial artery at the level of arm and superior and inferior ulnar collateral branches were absent. The average length of brachial artery was observed to be 26.3±1.76 cm varying from 18 cm to 32 cm. The mean external diameter at the point of origin was between 10±0.98 mm.
Origin and Distribution of Medial Arm Perforators.
| Types of perforators (Based on diameter) | Origin | Total No. (Percentage) |
|---|
| Brachial artery | Superior ulnar collateral artery (SUCA) | Inferior ulnar collateral artery | Common interosseous artery |
|---|
| <0.5 mm | 19 (10%) | - | 1 (0.5%) | 1 (.5%) | 21 (11%) |
| 0.5-1 mm (Suitable perforators) | 71 (37%) | 36 (19%) | - | - | 107 (56%) |
| ≥1 mm (Ideal perforators) | 38 (20%) | 18 (9%) | 8 (4%) | - | 64 (33%) |
| Total No. (Percentage) | 128 (67%) | 54 (28%) | 9 (4.5%) | 1 (0.5%) | 192 |
Distribution of Perforators in relation to medial arm region.
| Location of perforators | Diameter (mm) | Total No. (Percentage) |
|---|
| <0.5 | 0.5-1 | >1 |
|---|
| Lower 1/3rd arm | 17(8.85%) | 59(30.7%) | 27(14.1%) | 103(53.65%) |
| Middle 1/3rd arm | - | 40(20.8%) | 15(7.8%) | 55(28.6%) |
| Upper 1/3rd arm | 4(2.08%) | 8(4.2%) | 22(11.46%) | 34(17.75%) |
| Total No. (Percentage) | 21(10.93%) | 107(55.7%) | 64(33.36%) | 192 |
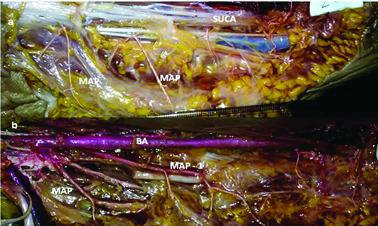
Source vessel: Regarding main source vessel giving rise to perforators of medial arm region, in 67% cases brachial artery was the main source vessel giving rise to perforators [Table/Fig-4,5a], followed by superior ulnar collateral artery (SUCA) branch in 28% of the cases and inferior ulnar collateral artery in rest of the cases except in one case, in which common interosseous artery was the main source vessel giving rise to majority of perforators, as it was located at a higher level in the arm [Table/Fig-2].
Graphical representation of number of perforators arising from each source vessel (brachial artery, superior and inferior ulnar collateral artery and common interosseous artery).
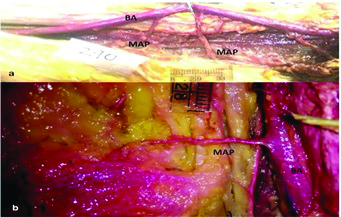
(a) Figure showing three perforators arising at the level of middle and lower one third of medial arm region. All these perforators are seen arising from brachial artery (BA). Upper medial arm perforator is seen in the middle, while middle and lower perforators were seen in the lower one third of medial arm region. Upper and lower perforators are of suitable types (diameter between 0.5–1 mm) and middle is an ideal type of perforator (diameter more than 1 mm). All these perforators are lying obliquely in relation to brachial artery (BA). (b) Figure showing suitable perforator (diameter more than 0.5 mm), running perpendicular to the brachial artery (BA) in the lower one third of medial arm region. Length of this perforator was 2.64 cm.
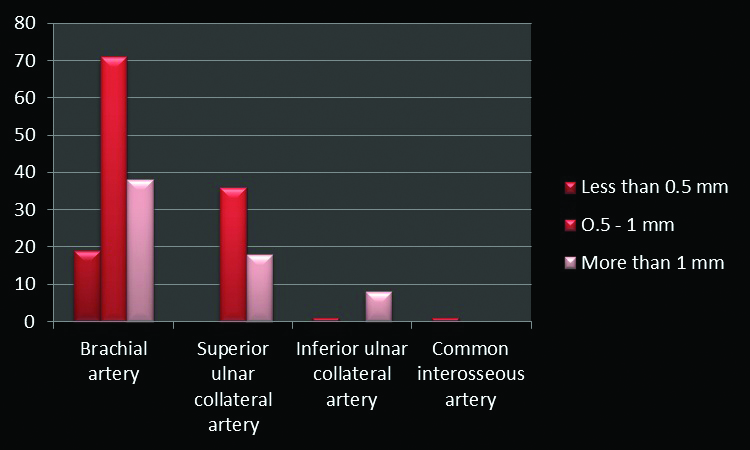
Dimensions of perforators: Out of 192 perforators, 21 (11%) had caliber less than 0.5 mm. 171 (89%) perforators had diameter more than 0.5 mm. Out of 171 perforators, 107 (56%) perforators were seen with diameter between 0.5 mm to 1.0 mm (suitable perforators) and 64 (33%) perforators had diameter more than 1.0 mm (ideal perforators). Almost, 19% (36) of suitable perforators and 9% (18) of the ideal perforators were seen arising from superior ulnar collateral branch. Length of perforators was observed to be 33.76±0.52 mm varying from 7 mm to 60 mm [Table/Fig-5b].
Distribution of perforators: 53.65% (103) of the perforators were located in the lower one third of arm; 28.6% (55) were observed in the middle one third of arm and rest 17.75% (34) in the upper one third of arm.
Suitable perforators (diameter between 0.5 and 1 mm)-30.7% (59) were present in the lower one third of arm, 20.8 % (40) in the middle one third and rest 4.2% (8) in the upper one third of medial arm region.
Ideal perforators (diameter >1 mm)–14.1% (27) perforators were located in the lower one third of medial surface of arm, 7.8% (15) in the middle one third and rest 11.46% (22) in the upper one third of medial surface of arm.
Direction and branching pattern of perforators–Perforators followed three types of branching patterns. 33% (64) perforators followed a straight course, without any branching along the region of supply. However, 45% (86) perforators further divided into two branches and 22% (42) perforators divided into more than two branches.
Direction of 49.2% (94) of the perforators was perpendicular to the main source vessel. However, 17.8% (34) of the perforators after perpendicular course, turned obliquely coursing either superiorly or inferiorly and 33% (64) followed only oblique course (11.5% superiorly and 21.5% inferiorly).
Distance of perforators from the standard bony landmark (medial epicondyle): Vertical distance of perforators from the Y axis (a horizontal line extending between the medial and lateral epicondyles) was observed to be 9.32±0.46 cm ranging from 0.44 to 16 cm. In 76% of the cases, this distance was 10 cm. However, in 6% of the cases, this distance was less than 1 cm and in rest of the cases it was variable. Mean horizontal distance from X axis (vertical line perpendicular to medial epicondyle, extending distally to proximally along the arm) was observed to be 4.4±1.72 cm.
Discussion
The medial arm has a complex and variable vascular anatomy. However, because of some characteristic properties of this region like ideal texture and thickness, hidden scar, low morbidity this region becomes the area of interest for flap surgeries. For increase success rate of flap surgeries in medial arm region, surgeons need to have precise knowledge of its vascular anatomy and incidence of variations in its vascularity.
Source Vessel
In the current cadaveric study, brachial artery was the main source vessel giving rise to medial arm region perforators in 67% of the cases, followed by 28% arising from superior ulnar collateral artery [Table/Fig-6,7] and very few from inferior ulnar collateral artery branch. Earlier studies also observed origin of medial arm perforators from axillary artery or deep brachial artery [7]. Authors in current study, very rare anomaly were observed in two cases, in which brachial artery gave rise to superficial ulnar artery at the level of proximal arm region. Reported incidence of superficial ulnar artery arising from brachial artery is 0.17% to 2% [7]. Previous literature have reported origin of superficial brachial artery in the axilla [8, 9]. If this anatomical variant is diagnosed preoperatively, a reliable flap with neurosensory potential can be designed over the superficial ulnar artery, which can be used for local reconstructive surgeries as well as reconstructive surgeries in other areas like head and neck, lower limb and even for coronary bypass surgeries, as also observed in other studies [5,10]. Moreover, it offers a pedicle with the wide arc of motion, which is a significant advantage over other regional and random-pattern flaps, which have a limited arc of rotation due to a distant vascular pedicle and the maintenance of a skin flap base, respectively [11].
Graphical representation of distribution pattern of perforators of various diameters arising from each source vessel i.e brachial artery, superior ulnar collateral artery, inferior ulnar collateral artery and common interosseous artery.
a) Figure showing perforators (MAP) arising from superior ulnar collateral artery (SUCA) in the middle and lower one third of arm region. These perforators are lying lying oblique to the source vessel; b) Figure showing perforators (MAP) originating from brachial artery (BA). In the figure, two main perforators are seen in the distal medial arm region. MAP–1 (Medial arm perforator–1) is located in the middle one third of arm region and is an ideal type (diameter > 1 mm) of perforator, while the distal perforator is of suitable type (diameter 0.5 mm–1 mm). Both these perforators are seen running obliquely along the brachial artery and then further bifurcate to give rise to several branches.
In above mentioned case, perforators were seen arising from common interosseous artery. Incidence of proximal origin of common interosseous artery is very low as described by previous literature [12,13]. Size and easy access of brachial artery at almost any level, particularly in the arm, makes it the artery of first choice for flap surgeries among plastic surgeons. Earlier report [14] also proposed the use of the medial arm skin flap based on the superior ulnar collateral artery. Flap surgeries based on superior ulnar collateral artery are still not very popular among surgeons, possibly because of variations in its vascular anatomy and sparse literature. In the current study, superior ulnar collateral artery was found to be the main source vessel supplying skin of medial arm region through its perforators in 28% cases. However, one of the previous studies [15] has reported quite a higher incidence (65%) of perforators arising from superior ulnar collateral artery. We further observed that 19% of suitable perforators and 9% of the ideal perforators were seen arising from superior ulnar collateral branch. Thus, it can be inferred that perforators arising from SUCA can be considered for various reconstructive perforator flap surgeries, especially local elbow region defects as they have relatively large calibre and mostly located in the distal medial arm region. Due to their location, their pedicle can be easily rotated for use in local reconstructive surgeries of elbow region.
Location of Perforators
The location and length of the perforator vessels will be factored into the design and size of the flap. This step is important for every flap. Exposure must be adequate to access a good length of recipient vessel.
Dimensions of Perforators
The length of perforator depends upon the depth and size of main vessel of origin along with the technique used during surgery [16]. In the current study, mean length of perforators was observed to be 33.76 mm varying from 7 mm to 60 mm. Similar results (maximum length upto 60 mm) were observed by authors in the previous study [10]. Preoperative knowledge of subcutaneous segment origin as well as its length facilitates accurate planning of surgery. The knowledge of size of the perforators and their anatomic and potential territories is necessary to be able to precisely approximate the safer dimensions of the flap as observed by Panse NS et al., [17]. The diameter of the vessels becomes larger as the flap vessels are dissected more proximally as reported by previous study [16]. In the current study, we observed the diameter of perforator vessels at the point of origin. We found an average of 56% perforators with a diameter > 0.5 mm, which were termed as suitable perforators and 33% of the perforators of diameter more than 1 mm (ideal perforators). As per literature [18] larger the diameter of the perforator lesser is the chance of necrosis of the flap due to better vascularisation. Thus, medial arm region offers one of the potential site for flap surgeries due to rich vascular supply being provided by large calibre perforators as large calibre vessels supply a greater volume of adipocutaneous tissue and represent better vascular pedicles.
Direction and Branching Pattern of Perforators
After their origin from the main source vessel, perforators take variable course. Some of them run perpendicular to the main vessel, while others either follow oblique course directly or after running perpendicular, follow oblique superior or inferior course. In the current study, majority of perforators (49%) were observed to follow perpendicular course in relation to the main vessel [Table/Fig-7]. Out of these, 17.8% of the perforators after running perpendicularly took oblique course. We further observed branching pattern of the perforators. Perforators running perpendicularly are easily accessible, whereas those following oblique course are difficult to locate as well as require meticulous dissection. Additionally, there are more chances of damage to perforators lying obliquely rather than those lying perpendicularly during surgery. We observed maximum (67%) incidence of single trunk dividing into two or more than two branches. However, it is suggested that perforators should not be dissected up to their branching level so as to avoid damage to them.
Regarding location of perforators, maximum concentration of perforators was observed to be in the lower one third of medial arm region. Most constant location for perforators was observed to be 9.32±0.46 cm from the Y axis and 4.4±1.72 cm from the X axis [Table/Fig-8]. Almost 53.7% perforators were located in lower one third of medial arm region.
a) To validate the results, a blind incision was given to locate the perforators on the medial arm region. Incision was given 10 cm proximal to the Y axis (horizontal line extending between the medial and lateral epicondyles) and 5 cm lateral to the X axis (vertical line perpendicular to the medial epicondyle, along the long axis of arm). A suitable type perforator was found (diameter 0.5 mm–1 mm), whose length was observed to be 2.52 cm. On the basis of this perforator, a flap is raised on the medial arm region. (b) This flap was rotated so as to see its usefulness for local reconstructive surgeries of elbow region. This flap could reach and cover the elbow region.
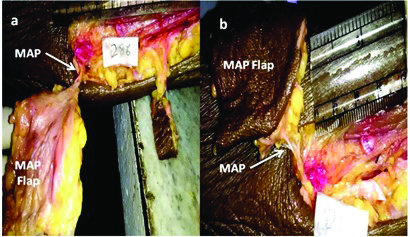
Knowledge of location of perforators can help in designing of flaps accordingly as it depends on position of the perforators. Other studies [7,19] also support our view that the perforators of the inner arm vessels are highly reliable, always present, could be easily located and have a wide enough diameter. Compared with posterior arm, scapular, pectoralis major flaps, the thoracodorsal artery perforator flap and the lateral thoracic fasciocutanous island flap, the donor site is well hidden and medial arm region provides excellent contour and texture matching for reconstructive surgeries in region of head and neck as well as axilla [20-22]. Thus, it can be inferred that medial arm region, with perforators of diameter more than 0.5 mm and length either 3 cm or more has the potential for use in various perforator flap reconstructive surgeries.
Limitation
Due to time constraint, the study could not be expanded further. But more studies like these should be conducted in future so as to explore other sites for flap surgeries.
Conclusion
In current study, authors found that almost 89% (171) of the perforators found in medial arm region have diameter more than 0.5 mm and mean length either 3 cm or more. Moreover, these perforators were found to be consistently located at 9.32±0.46 cm from the Y axis and 4.4±1.72 cm from the X axis. Due to comparatively large diameter of most of the perforators, there are less chances of necrosis of flap and consistent location of perforators helps in their easy location during surgeries. Thus, this region has the potential for future use in various perforator flap reconstructive surgeries.