Genital Tuberculosis: Coexisting Vulval and Endometrial Tuberculosis in a Multiparous Female
Shalini Bahadur1, Ruchi Rathore2, Ruchi Bansal3, Upasana Verma4, Namrata Nargotra5
1 Associate Professor, Department of Pathology, NDMC Medical College and Hindu Rao Hospital, Delhi, India.
2 Assistant Professor, Department of Pathology, NDMC Medical College and Hindu Rao Hospital, Delhi, India.
3 Senior Resident, Department of Pathology, NDMC Medical College and Hindu Rao Hospital, Delhi, India.
4 Medical Officer, Department of Obstetrics and Gynaecology, NDMC Medical College and Hindu Rao Hospital, Delhi, India.
5 Head, Department of Pathology, NDMC Medical College and Hindu Rao Hospital, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ruchi Bansal, 261, Aravali Apartments, Alaknanda, Delhi-110019, India.
E-mail: dr.ruchibansal@rediffmail.com
Vulval Tuberculosis (TB) is rare and is diagnosed in only about 0.2% cases of genital tract TB which itself constitutes 0.2 to 2% of all gynaecological cases. Clinically signs and symptoms are variable ranging from asymptomatic to infertility and chronic Pelvic Inflammatory Diseases (PID). Female genital tract is involved via haematogenous or lymphatic dissemination or from direct contiguity from a primary focus of infection elsewhere in the body. Diagnosis of vulval or endometrial TB is made on histopathological examination of lesions which show classical caseating granulomas. Demonstration of Mycobacterium is considered as gold standard. Authors in the past have found typical epitheloid granulomas but failed to obtain positive results on ZN staining. We hereby present a rare case of TB of vulva in an unsuspecting multiparous middle aged female who presented with two years amenorrhoea, burning micturition and difficulty in walking, backache and lower abdominal pain off and on and a popular ulceration on inner aspect of labia minora. The patient was clinically misdiagnosed as pelvic inflammatory disease. Investigations following diagnosis of vulval TB helped discover underlying co existent endometrial tubercular involvement as well. In present case Acid Fast Bacilli (AFB) were identified on ZN staining of the histopathology sections.
Endometrium, Granulomas, Mycobacterium, Vulva
Case Report
A 36-year-old multiparous female with history of amenorrhoea for two years presented with recent onset of burning micturition and difficulty in walking. She also had backache and lower abdominal pain off and on. Local examination showed papular ulceration of size 2x2 cm on inner aspect of labia minora with induration and mild discharge coating the ulcer surface. No palpable superficial inguinal lymphadenopathy was found. Cervix and vagina appeared healthy on a per speculum examination with anteverted cervix and retroverted uterus. Bilateral fornices were non tender. Discharge from ulcer had not been sent for microbiological evaluation. She had been on irregular treatment for (PID) for past one year. No past history suggestive of Anti-Tubercular Therapy (ATT) or family history of TB was found. VDRL and HIV1 and 2 were non reactive for syphilis and HIV respectively.
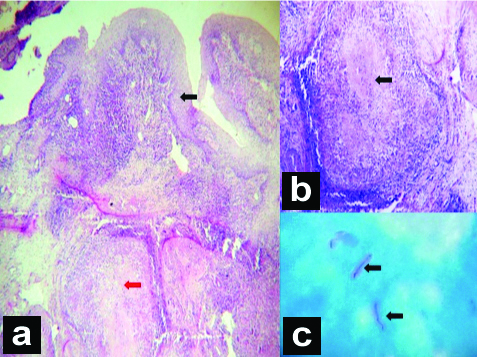
X-ray chest did not show any old or active lesions suggestive of TB. Vulval lesions were biopsied. Histopathology showed multiple granulomas with classical central caseous necrosis and peripheral rim of langhans giant cells, epithelioid cells, lymphocytes and plasma cells [Table/Fig-1]. AFB were detected on Ziehl-Neelsen stain (ZNS). Vulval TB was confirmed.
a) Vulval biopsy lined by stratified squamous epithelium (black arrow) showing multiple epitheloid cell granulomas (red arrow) (H&E 4X); b) Granuloma with central caseation and peripheral rim of langhans giant cells, epitheloid cells, lymphocytes and plasma cells (black arrow) (H&E 40X); c) AFB on ZN stained smear (black arrow) (ZN Stain 100X).
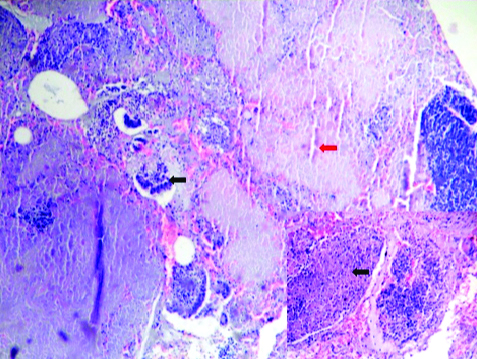
Subsequently on repeat evaluation a tiny lymph node was found palpable in right anterior mid cervical region. FNAC showed caseous necrosis yet again with detection of AFB on ZNS. On ultrasound pelvis, 8 mm of endometrial thickness was documented. This prompted an endometrial biopsy which showed predominantly caseous necrosis with few ill formed granulomas and occasional fragmented endometrial glands. AFB was demonstrated on ZN stained section and tubercular endometritis was reported [Table/Fig-2]. Mantoux was strongly positive. Patient was put on antitubercular treatment for nine months regime, with isoniazid, rifampicin, pyrazinamide and ethambutol for two months, isoniazid, rifampicin and pyrazinamide for subsequent one month followed by isoniazide and rifampicin for another six months.
Endometrial biopsy showing fragmented endometrial glands (black arrow) with areas of caseous necrosis (red arrow) (H&E 40X) Inset showing ill formed granuloma (black arrow). (H&E 40X).
Discussion
Vulval TB (TB) is rare, diagnosed in only about 0.2% cases of genital tract TB [1] which itself constitutes 0.2 to 2% of all gynaecological cases [2]. Characteristically upper female genital tract is frequently involved in women of reproductive age group who are either asymptomatic or present with infertility, complications of pregnancy, abnormal vaginal bleeding, discharge, menstrual irregularities and abdominal pain [2]. A variable age of presentation ranging from months to 85 years has been observed [3]. Lesions themselves are ulcerative, hypertrophic or seen as multiple discharging sinuses. Present case is an unusual one as TB of vulva was found to co-exist with endometrial TB in an unsuspecting multiparous middle aged female under evaluation for pelvic inflammatory disease. To the best of our knowledge after extensive search of literature we were not able to find a similar correlation.
TB is a common infectious disease prevalent in developing countries like India. It is relatively rarer in developed nations. The NTCP was launched in 1962 with the proposal to curtail it and subsequently revised in 1993, [4,5]. Genital tract TB accounts for 15% of all extrapulmonary cases of the disease [3]. Clinically signs and symptoms are variable ranging from asymptomatic to infertility and chronic PID [6].
Clinically, patients with genital TB may have no evidence or prior documentation of disease elsewhere in the body. Female genital tract is involved via haematogenous or lymphatic dissemination from a primary focus of infection elsewhere in the body. Spread by contiguity from intra-abdominal sites can take place to fallopian tubes [2]. Disease can be transmitted sexually from male partner suffering from TB of epididymis or seminal vesicles. This is extremely rare and unusual. Lesions on vulva by far are ulcerating with or without sinus tracts. Hypertrophic vulval TB is infrequent. Presence of nodules [2], fissures and polypoidal growths have also been documented by various authors [2-4]. Ulceration and suppuration may occur in draining inguinal lymph nodes.
Diagnosis of vulval or endometrial TB is reached upon by histopathological examination of lesions which show classical caseating granulomas. Demonstration of Mycobacterium is considered as gold standard. ZN staining requires presence of a large bacterial load (at least 105/mL) [7,8]. In present case AFB were identified on ZN staining of the histopathology sections. Reportedly one third of cases are culture negative [9]. Several authors in the past have found typical epitheloid granulomas but failed to obtain positive results on ZN staining [3,9].
Sarcoidosis, amoebiasis, foreign body granulomas, brucellulosis, tularemia and schistosomia are other conditions associated with formation of granulomas albeit without caseation and may be ruled out if hard tubercles are encountered in biopsy specimen. Vulval TB is a rare entity frequently misdiagnosed and treated as sexually transmitted disease, as occurred in present case. An estimated 5-10% infertility cases are attributed in females to genital TB. In present case infertility was not present. Secondary amenorrhea however, a common feature associated with genital TB was present and should have prompted investigations earlier in keeping with a high index of suspicion for tubercular involvement of endometrium or other any other part genital tract.
Surgery has limited role in management of vulval TB. Radical surgery in advertently leads to non healing wounds. Combined anti tubercular drug therapy is the mainstay for treatment, duration of which varies from six months to a year [10] with excellent cure rates and final outcome.
Conclusion
TB is a disease of myriad and varied presentations. TB of female genital tract is rare and its sequel can have profound effects on the affected female. The present case highlights its unusual presentation and subsequent diagnosis on involvement of vulva and endometrium in a multiparous, apparently immune competent patient.
[1]. WHO, Global Tuberculosis Control-Epidemiology, Strategy, Financing, World Health Organization, 2009 [Google Scholar]
[2]. Arakeri SU, Sinkar P, An unusual gross appearance of vulval tuberculosis masquerading as tumorCase Rep Obstet Gynecol 2014 2014:81540110.1155/2014/81540125298898 [Google Scholar] [CrossRef] [PubMed]
[3]. Iftikhar N, Kiyani S, A rare case of vulval tuberculosisISRA Med J 2015 7(2):111-13. [Google Scholar]
[4]. Kaur T, Dhawan S, Aggarwal A, Bansal S, Vulval tuberculosisJ obstet gynacol India 2012 62(4):450-51.10.1007/s13224-012-0131-223904710 [Google Scholar] [CrossRef] [PubMed]
[5]. Park K, Health programs in IndiaIn: Parks textbook of preventive and social medicine 2015 23rd edJabalpur(India)M/s Banarsi Das Bhanot Publishers:427 [Google Scholar]
[6]. Akhlaghi F, Hamedi A, Postmenopausal tuberculosis of cervix, vagina and vulvaInt J Gynaecol Obstet 2004 3:01-03.10.5580/15e6 [Google Scholar] [CrossRef]
[7]. Nabag WOM, Nur Hassan A, Sayed DM, EL Sheikh MA, Endometrial tuberculosis and secondary amenorrhoea: A report of three cases in SudanJ Minim Invasive Surg Sci 2012 1(1):30-33.10.17795/minsurgery-2056 [Google Scholar] [CrossRef]
[8]. Butt T, Ahmad RN, Kazmi SY, Afzal RK, Mahmood A, An update on the diagnosis of tuberculosisJ Coll Physicians Surg Pak 2005 13(12):728-34. [Google Scholar]
[9]. Nanjappa V, Suchismitha R, Devaraj HS, Shah MB, Anand A, Rahim SN, Vulval tuberculosis-An unusual presentation of disseminated tuberculosisJ Assoc Physicians India 2012 60:49-52. [Google Scholar]
[10]. Lam SK, Chan KS, Chin Robert: A rare case of vulval tuberculosisHong Kong J Gynaecol Obstet Midwifery 2007 7:56 [Google Scholar]