Penicillium roqueforti: A Rare Fungus Causing Infection in an Immunocompromised Host
Jisha Asokan1, Ajith Kumar Vellani Thamunni2, Rema Devi Surendran3
1 Senior Resident, Department of Microbiology, Government Medical College, Kozhikode, Kerala, India.
2 Professor and Head, Department of Paediatrics, Government Medical College, Manjeri, Kerala, India.
3 Professor and Head, Department of Microbiology, Dr. SMCSI Medical College, Thiruvananthapuram, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jisha Asokan, Chaithanya, 33/5580, Golf Link Road, Chevayur, Kozhikode, Kerala-673017, India.
E-mail: drjisha@rediffmail.com
Penicillium roqueforti is a fungus that widely exists in the environment and is often non-pathogenic to humans. However, in immunocompromised hosts, it may be recognized as a cause of systemic mycosis. We report a rare case of mycosis due to Penicillium roqueforti in six-year-old haemato-oncology patient.
Acute Lymphoblastic Leukaemia, North Kerala, Penicillium species, Systemic mycosis
Case Report
A six-year-old boy was admitted to haemato-oncology unit at a tertiary care centre in North Kerala with febrile neutropenia. He was a known case of Acute Lymphoblastic Leukaemia (ALL) on maintenance chemotherapy since two years. He revealed hepatosplenomegaly, moderate ascites and left sided pleural effusion. Computed Tomography Scan and Ultrasonography revealed grossly dilated gallbladder with minimal pericholecystal fluid suggestive of cholecystitis. He was a Hepatitis B carrier and had prolonged fever and persistent neutropenia. He was on broad spectrum antibiotics as per febrile neutropenia protocol since two weeks but was not responding to it [1].
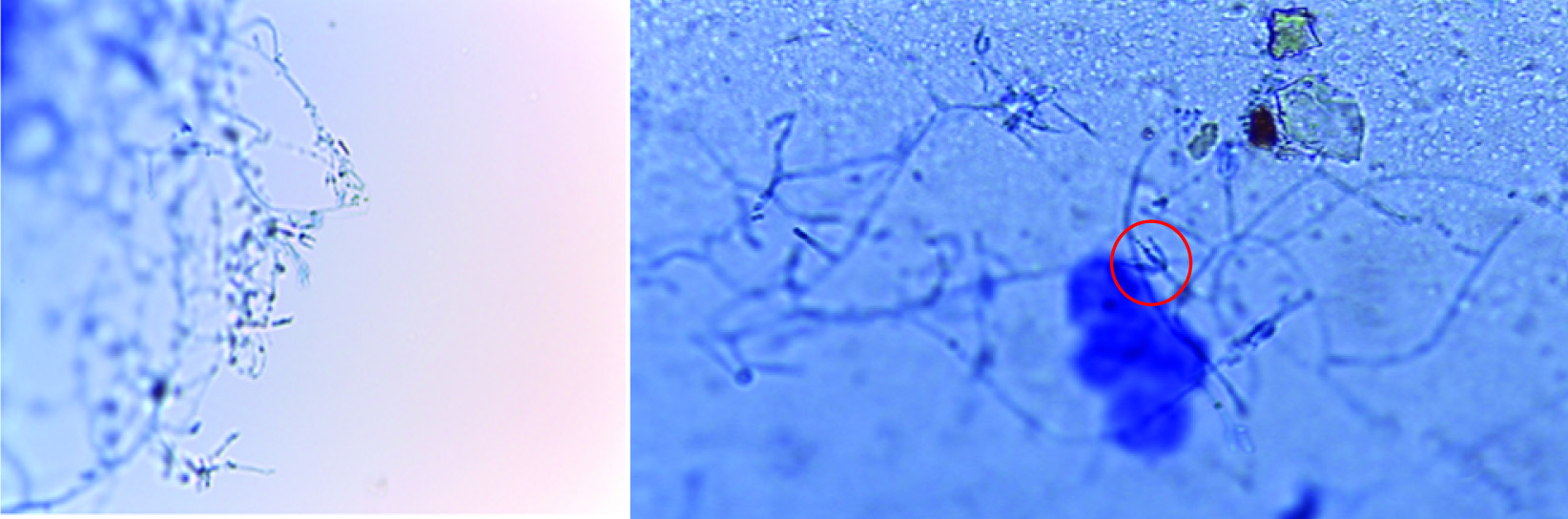
In his previous admission for maintenance chemotherapy, he complained of throat pain and mild difficulty in swallowing. He had fever with neutropenia; his absolute neutrophil count was 230 cells/μL. His blood sample was collected for routine blood culture in Brain Heart Infusion Broth (BHIB) and was incubated at 37°C for 24 hours. After 24 hours, it was subcultured onto Blood Agar (BA), MacConkey (MA) agar and Sabouraud’s Dextrose Agar (SDA) as a part of routine bacterial and fungal culture. On the fourth day, the fungal culture on SDA kept at room temperature (27°C), yielded growth of the fungi. By the end of one week, the BHIB and BA also showed similar growth. Microscopic examination using Lactophenol Cotton Blue (LCB) stain, showed hyaline fungi morphologically resembling Penicillium. Septate hyaline hyphae and branching conidiophores were seen. From the tip of the conidiophores, phialides grouped in brush like clusters were found which contain unicellular round to ovoid smooth conidia arranged in chains [Table/Fig-1a,b].
a) Lactophenol cotton blue (LPCB) mount of Penicillium roqueforti isolated from blood of haemato-oncology patient; b) LPCB mount of isolate showing Flask shaped phialides bearing unbranched round conidia (marked in the circle)
On further incubation, the SDA showed greenish pink, velvety colonies with woolly areal hyphae. Culture on reverse showed reddish brown pigment production [Table/Fig-2a,b].
a) Growth of Penicillium roqueforti on Sabouraud’s Dextrose Agar (SDA) showing greenish pink and yellow velvety colonies with woolly areal hyphae; b) Culture on SDA on the reverse side showing reddish brown pigment production.

This was thought to be a contaminant. The patient slightly improved with antibiotics; Vancomycin 1 gm (IV) BD and Piperacillin/Tazobactam 300 mg/kg/day (IV) 8th hourly and was put on prophylactic oral Fluconazole 100 mg/kg/day and was sent home. On subsequent admission, he continued having fever and neutropenia and hence, was started on broad spectrum antifungal amphotericin B. The average absolute neutrophil count was around 600 cells/μL. Blood culture report of his second and third sample too revealed the same fungus as that in the previous admission. Although, the child was put on Amphotericin B (IV) 60 mg/kg/day for two weeks, his condition kept deteriorating. Finally, (IV) Voriconazole was given 4 mg/kg 8th hourly, was used to treat the infection, for four days.
Since, all three samples from the immunocompromised child grew the same fungus, it was really significant. Speciation was done at Microbiological Laboratories Coimbatore by MALDI-TOF, where it was identified as Penicillium roqueforti. By the time the species identification was done, the patient deteriorated and succumbed to death on 29th day of admission.
Discussion
Invasive Fungal Infection (IFI) is among the major causes for morbidity, mortality and economic burden in haemato-oncology patients like those with Acute Lymphoblastic Leukaemia (ALL) [2].
Penicillium species are usually non-pathogenic to humans and are commonly found in the environment. However, they can be virulent pathogens and that can cause invasive infection and death in an immunocompromised hosts.
Penicillium roqueforti is a common saprophytic fungus that is used as a starter culture in the production of Roquefort cheese and other varieties of blue cheese containing an internal mould [3].
Penicillium roqueforti belong to the family Trichocomaceae. It is widespread in nature and can be isolated from soil, decaying organic matter and plants [4].
Though it gives colour and flavour to blue-veined cheeses, it is also a common spoilage organism in various food products [5]. It destroys large amounts of vegetables, fruits, and cereal grain, both pre- and post-harvest every year. The fungus produces allergenic spores and hazardous mycotoxins that cause reduced nutritional values of food and feed [6].
Penicillium species can cause opportunistic infections [7]. Patients with Penicillium species infections have been treated successfully with itraconazole [8] Amphotericin B or fluconazole [8,9]. However, some patients with conditions caused by Penicillium species have died despite treatment with Amphotericin B and Itraconazole [7,10]. In patients with nosocomial infections or infections complicating organ failure, higher mortality rates are seen when pulmonary infections are caused by fungi, including Penicillium species [11]. In a large retrospective study conducted among patients in Italy with haematologic malignancies, two-thirds of the 538 Invasive Fungal Infection cases were attributable to moulds out of which Penicillium caused only less than 2% of invasive infections [12]. In the present case, the patient must have acquired the pathogen from an environmental source, which, over a period of time, ended up in a fatal systemic infection.
P. roqueforti from multiple cultures combined with it being a relatively uncommon species in our institution, makes laboratory contamination less likely in our case. It is striking that all three blood culture report showed the same result in this patient. ALL with intensive chemotherapy imposes a far greater degree of an immunocompromised state for an opportunistic pathogen. Unlike the fatal pneumonia case caused by P.digitatum, an immunodiffusion testing for antibodies was not done here due to lack of facilities [7].
Conclusion
To the best of our knowledge, this is the first report of invasive infection with Penicillium roqueforti. The patient had no known history of exposure to cheese, but was likely to get it from soil or spores present in air. Moreover, chemotherapy was going on for ALL could have been one of the factors that might have facilitated the infection. In this case, antifungals were ineffective in treating the blood stream involvement. Although, human infections with P. roqueforti are considered rare, it appears that this organism can be very virulent and resistant to antifungals. Hence, further investigations are warranted to render diagnosis and treatment of such rare fungal infections.
[1]. Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of americaClin Infect Dis Off Publ Infect Dis Soc Am 2011 Feb 15 52(4):e56-93.10.1093/cid/cir07321258094 [Google Scholar] [CrossRef] [PubMed]
[2]. Bhatt VR, Viola GM, Ferrajoli A, Invasive Fungal Infections in Acute LeukemiaTher Adv Haematol 2011 2(4):231-47.10.1177/204062071141009823556092 [Google Scholar] [CrossRef] [PubMed]
[3]. Secondary Metabolites from Penicillium roqueforti, A Starter for the Production of Gorgonzola Cheese [Internet]. [cited 2017 May 25]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5076727/ [Google Scholar]
[4]. Gen Bio II, Chap 29 Vocab Flashcards | Quizlet [Internet]. [cited 2017 Aug 27]. Available from: https://quizlet.com/66597871/gen-bio-ii-chap-29-vocab-flash-cards/ [Google Scholar]
[5]. Gillot G, Jany J-L, Coton M, Le Floch G, Debaets S, Ropars J, Insights into Penicillium roqueforti Morphological and Genetic DiversityPLoS ONE [Internet] 2015[cited 2017 May 27] 10(6)Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4475020/10.1371/journal.pone.012984926091176 [Google Scholar] [CrossRef] [PubMed]
[6]. Druvefors UÄ, Passoth V, Schnürer J, Nutrient Effects on Biocontrol of Penicillium roqueforti by Pichia anomala J121 during Airtight Storage of WheatAppl Environ Microbiol 2005 71(4):1865-69.10.1128/AEM.71.4.1865-1869.200515812013 [Google Scholar] [CrossRef] [PubMed]
[7]. Mok T, Koehler AP, Yu MY, Ellis DH, Johnson PJ, Wickham NW, Fatal Penicillium citrinum pneumonia with pericarditis in a patient with acute leukemiaJ Clin Microbiol 1997 35(10):2654-56. [Google Scholar]
[8]. Gelfand MS, Cole FH, Baskin RC, Invasive pulmonary penicilliosis: successful therapy with amphotericin BSouth Med J 1990 83(6):701-04.10.1097/00007611-199006000-000292192469 [Google Scholar] [CrossRef] [PubMed]
[9]. Lyratzopoulos G, Ellis M, Nerringer R, Denning DW, Invasive Infection due to Penicillium Species other than P. marneffeiJ Infect 2002 45(3):184-95.10.1053/jinf.2002.105612387776 [Google Scholar] [CrossRef] [PubMed]
[10]. Hsu J-H, Lee M-S, Dai Z-K, Wu J-R, Chiou S-S, Life-threatening airway obstruction caused by penicilliosis in a leukemic patientAnn Haematol 2009 88(4):393-95.10.1007/s00277-008-0606-518797869 [Google Scholar] [CrossRef] [PubMed]
[11]. Chen KY, Ko SC, Hsueh PR, Luh KT, Yang PC, Pulmonary fungal infection: emphasis on microbiological spectra, patient outcome, and prognostic factorsChest 2001 120(1):177-84.10.1378/chest.120.1.17711451835 [Google Scholar] [CrossRef] [PubMed]
[12]. Pagano L, Caira M, Candoni A, Offidani M, Fianchi L, Martino B, The epidemiology of fungal infections in patients with haematologic malignancies: the SEIFEM-2004 studyHaematologica 2006 91(8):1068-75. [Google Scholar]