Intraosseous Collagenous Fibroma (Desmoplastic Fibroblastoma) Involving Maxillary Bone
Natália Galvão Garcia1, Silas Antonio Juvencio De Freitas Filho2, Cléverson Teixeira Soares3, Caio Márcio Figueiredo4, Denise Tostes Oliveira5
1 Postdoctoral Fellow, Department of Surgery, Stomatology, Pathology and Radiology, Area of Pathology, Bauru School of Dentistry, University of São Paulo, Bauru, São Paulo, Brazil.
2 PhD Student, Department of Surgery, Stomatology, Pathology and Radiology, Area of Pathology, Bauru School of Dentistry, University of São Paulo, Bauru, São Paulo, Brazil.
3 Pathologist, Department of Pathology, Lauro de Souza Lima Institute, Bauru, São Paulo, Brazil.
4 Professor, Section of Periodontology and of Implantodontology, Hospital for Rehabilitation of Craniofacial Anomalies, University of São Paulo, Bauru, São Paulo, Brazil.
5 Professor, Department of Surgery, Stomatology, Pathology and Radiology, Area of Pathology, Bauru School of Dentistry, University of São Paulo, Bauru, São Paulo, Brazil.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Denise Tostes Oliveira, Professor, Department of Surgery, Stomatology, Pathology and Radiology (Area of Pathology) Bauru School of Dentistry, University of São Paulo, Al. Dr. Octávio Pinheiro Brisolla, 9-75, CEP: 17012-901, Bauru, São Paulo, Brazil.
E-mail: denisetostes@usp.br
The collagenous fibroma (desmoplastic fibroblastoma) is a rare benign soft tissue tumour that can occur in the oral mucosa; intraosseous lesion is uncommon. A 43-year-old woman showed a well-circumscribed intraosseous radiolucency involving the maxillary edentulous area corresponding to 22 and 23 teeth. On intraoral examination, the edentulous ridge was covered by normal oral mucosa. The patient underwent an excisional biopsy and histopathological analysis revealed a tumour composed of spindle to stellate shaped cells scattered within a myxocollagenous stroma with invasion of skeletal muscle. The collagen bands showed strong positivity for Masson’s trichrome and the tumour cells showed focal positivity for HHF-35 and α-smooth muscle actin. The diagnosis was intraosseous collagenous fibroma according to both clinical and histopathological patterns. The patient was followed up for six months and there were no signs of recurrences. We report the second case of oral intraosseous collagenous fibroma and a critical review of English literature of the tumour in oral cavity.
Benign tumour, Intraosseous lesion, Oral cavity
Case Report
A 43-year-old woman who was using a removable partial prosthesis came with a request for placement of dental implants. During anamnesis, the patient reported agenesis of left maxillary lateral incisor and extraction of impacted maxillary left canine a few years ago. There was no pain and no history of trauma in that region. The radiographic records of the patient showed well-circumscribed radiolucency involving maxillary edentulous area corresponding to 22 and 23 [Table/Fig-1a]. The radiographic hypothesis was odontogenic cyst or tumour.
Radiographic and clinical manifestations: a) Radiographic features of the intraosseous desmoplastic fibroma involving the maxillary bone (arrow); b) Clinical characteristics of the alveolar ridge covered by normal oral mucosa in the lesion area; c) Surgical specimen of the lesion.
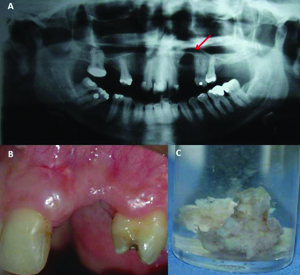
On intraoral examination, the edentulous ridge was covered by normal oral mucosa [Table/Fig-1b]. The patient underwent an excisional biopsy and, during the trans-surgical procedure, we detected that the lesion was solid mass and firmly adhered to the oral mucosa. In addition, the vestibular and palatine bone between 21 and 24 teeth were absent.
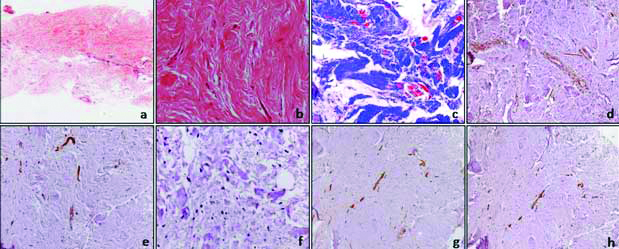
On gross examination we observed two fragments of smooth brown tissue measuring 2.0 x 1.5 x 0.5 cm, which were sent for histopathological analysis [Table/Fig-1c]. The diagnostic hypothesis was odontogenic lesion. Microscopically the tumour was composed of spindle to stellate shaped cells scattered within a myxocollagenous stroma with invasion of the skeletal muscle [Table/Fig-2a,b]. Neither cellular atypia nor mitotic figures were observed. Some areas of the tumour had collagen bands showing strong positivity for Masson’s trichrome [Table/Fig-2c]. The immunohistochemical staining was negative for S-100 [Table/Fig-2d], CD34 [Table/Fig-2e] and Ki-67 [Table/Fig-2f]. A focal positivity was observed for HHF-35 [Table/Fig-2g] and smooth muscle actin [Table/Fig-2h]. The diagnosis was collagenous fibroma according to both clinical and histopathological patterns. The patient was followed up for six months and there was no sign of recurrence.
a) Dense collagenous matrix in oral collagenous fibroma (H&E, 5X); b) Hypocellularity in dense fibrous area (H&E, 20X); c) Dense collagenous stroma (blue) and some positive areas for muscle (red) (Masson’s Trichrome, 20X); d) S-100 protein negative in neoplastic cells and positive in neural fascicles (Immunohistochemistry: S100, 10X); e) Negative for CD34 in neoplastic cells and positive in blood vessels (Immunohistochemistry: CD34, 10X); f) Negative for Ki-67 (Immunohistochemistry: Ki-67, 40X); g) Focal immunoexpression of HHF-35 in tumour cells and muscle fibers (Immunohistochemistry: HHF-35, 20X); h) Immunoreactivity for α-smooth muscle actin in few cells and in the blood vessels (Immunohistochemistry: smooth muscle actin, 10X).
Discussion
Since 1995 when Evans HL [1] described the collagenous fibroma only ten cases (PubMed and LILACS) were reported within the oral cavity as described in the [Table/Fig-3]. This tumour affects mainly soft tissue, however, although extremely rare, intraosseous manifestations, as described in the present case, can be found. Among the ten cases of collagenous fibroma of the oral cavity, only one described by Jaafari-Ashkavandi Z et al., [2] was intraosseous and located in the maxillary alveolar bone.
Clinical information on 11 cases of collagenous fibroma in the oral cavity.
| Authors (Year) | Age/sex | Location | Tumour size (cm) | Previous trauma | Follow up (months) |
|---|
| Jaafari-Ashkavandi Z et al., (2017) [2] | 58/F | Maxillary alveolar bone | 1.3 | No | No recurrence -12 |
| Mesquita RA et al., (2001) [3] | 37/F | Palate | 5 | No | No recurrence -6 |
| Pereira TSF et al., (2016) [4] | 56/M | Mandibular alveolar ridge | - | No | No recurrence -8 |
| Varghese T et al., (2014) [5] | 8/M | Buccal mucosa | 3 | No | No recurrence -12 |
| Nonaka CF et al., (2010) [6] | 87/F | Tongue | 0.7 | No | No recurrence -9 |
| Gonzalez-Moles MA et al., (2004) [7] | 55/F | Palate | 2 | No | Not treatment |
| Bhagalia S et al., (2012) [8] | 58/F | Gingiva | 2 | No | No recurrence -4 |
| de Sousa SF et al., (2011) [9] | 56/M | Buccal mucosa | 3.5 | No | No recurrence -12 |
| Cazal C et al., (2005) [10] | 42/F | Maxillary alveolar ridge | 1 | No | No informed |
| Shimoyama T et al., (2005) [11] | 49/F | Palate | 6 | No | No recurrence -48 |
| Present case | 42/F | Maxillary alveolar bone | 2 | No | No recurrence -6 |
Notes: pes of implan
F-Female
M-Male
Clinically, collagenous fibroma manifests as a painless, slow-growing mass, sessile or pedunculated, well circumscribed, with size varying from 1 to 6 cm [3-6]. This tumour occurs in a wide anatomical distribution but most lesions arise in the subcutaneous tissue or skeletal muscle [3,7,8]. In the present case during the trans-surgical procedure we observed that the lesion was firmly adhered to the oral mucosa and probably the tumour arise from the fibroblasts of the submucosa covering the adjacent maxillary bone.
In our case report, the radiographic examination showed well-circumscribed radiolucency involving the edentulous anterior maxillary bone area corresponding to 22 and 23 teeth and the clinical hypothesis was odontogenic lesion. The unique case of an intraosseous collagenous fibroma described in the English literature also showed a well-circumscribed rounded radiolucency; however the tumour was located in the periapical area associated with the root of right upper incisors [2].
Microscopically, in the present case, the tumour was composed of spindle to stellate shaped cells scattered within a myxocollagenous stroma with invasion of the skeletal muscle [Table/Fig-2a,b]. According to the literature, these microscopic findings are typical of collagenous fibroma, being of great importance for the establishment of diagnosis [4,9]. Immunohistochemistry for collagenous fibroma may contribute to exclude other similar lesions [2,9]. We performed immunohistochemical staining for S-100 protein, CD34, HHF-35, α-smooth muscle actin and Ki-67. Tumour cells showed focal positivity for HHF-35 [Table/Fig-2g] and α-smooth muscle actin [Table/Fig-2h], confirming the previous findings observed by Pereira TSF et al., [4]. However, variations of reactivity for HHF-35 and α-smooth muscle actin can be observed [9]. In addition, some studies claim that the neoplastic cells may also show immunoreactivity to vimentin and Factor XIIIa [1,3,4,9]. The tumour cells, in our case, were negative for S-100 [Table/Fig-2d], CD34 [Table/Fig-2e] and Ki-67 [Table/Fig-2f], discarding the possibility of neural or vascular origin.
The histological differential diagnosis for collagenous fibroma of the oral cavity include lesions such as traumatic fibroma, inflammatory fibrous hyperplasia and giant cell fibroma [3,8]. However, for cases with bone involvement, a scar, neurofibroma, solitary fibrous tumour, chondromyxoid fibroma, low grade fibromyxoid sarcoma, calcifying fibrous-pseudo tumour and still desmoplastic fibroma should be considered [2]. In our case, there was no history of previous trauma that could cause a reactive condition or scar. Neurofibroma and solitary fibrous tumour were excluded after immunohistochemical analysis for S-100 protein and CD34. Negative expression for Ki-67 and absence of chondroid and myxoid areas excluded chondromyxoid fibroma and fibromyxoid sarcoma, respectively. Furthermore, the absence of areas of calcification excluded calcifying fibrous-pseudo tumour. Desmoplastic fibroma was discarded due to hypocellularity and non-fascicular pattern.
The aetiology of collagenous fibroma is still uncertain, because usually no inciting neoplastic event is clinically mentioned, and no specific cause of a reactive condition is microscopically identified [1,3]. However, it has been suggested that a chromosomal abnormality in the same band of the long arm of chromosome 11, more specifically, a rearrangement of 11q12 may be associated with the lesion [5,10] As previously mentioned, in the present case, there was no history of previous trauma that could cause a reactive condition or scar. In addition, during the trans-surgical procedure was observed that the vestibular and palatine bone between 21 and 24 teeth were absent. Thus, our case reported, the maxillary bone loss and the invasion of the muscle fibers caused by lesion, reinforces the neoplastic profile of the collagenous fibroma.
Considering the cases reported in oral cavity, the collagenous fibroma in soft tissue seems to have an indolent behaviour and good prognosis without tumour recurrence [1,3,11]. Intraosseous tumours, as the present case, also showed similar behavior, presenting asymptomatic and small-sized lesions, without recurrence during the follow up [2]. Thus, the recommended treatment is total surgical excision for soft tissue or intraosseous lesions.
Conclusion
In conclusion, we reported the second case of oral intraosseous collagenous fibroma. Clinical and pathological information on new cases of oral collagenous fibroma are necessary for better knowledge of the lesion and elucidation of the aetiology.
Notes: pes of implan
F-Female
M-Male
[1]. Evans HL, Desmoplastic fibroblastoma. A report of seven casesAm J Surg Pathol 1995 19:1077-81.10.1097/00000478-199509000-00012 [Google Scholar] [CrossRef]
[2]. Jaafari-Ashkavandi Z, Shirazi MY, Assar S, Desmoplastic Fibroblastoma in Maxillary Alveolar Bone Mimicking An Odontogenic Lesion: A Novel Case Report with Review of LiteratureTurk Patoloji Derg 2017 [Epub ahead of print]10.5146/tjpath.2015.01355 [Google Scholar] [CrossRef]
[3]. Mesquita RA, Okuda E, Jorge WA, de Araújo VC, Collagenous fibroma (desmoplastic fibroblastoma) of the palate: A case reportOral Surg Oral Med Oral Pathol Oral Radiol Endod 2001 91(1):80-84.10.1067/moe.2001.10963811174576 [Google Scholar] [CrossRef] [PubMed]
[4]. Pereira TSF, de Lacerda JCT, Porto-Matias MD, de Jesus AO, Gomez RS, Mesquita RA, Desmoplastic fbroblastoma (collagenous fbroma) of the oral cavityJ Clin Exp Dent 2016 8(1):e89-92. [Google Scholar]
[5]. Varghese T, Pillai KS, Sarojini SB, Khosla E, Desmoplastic fibroblastoma (collagenous fibroma) in the oral cavityJ Indian Soc Pedod Prev Dent 2014 32(3):238-41.10.4103/0970-4388.13583425001444 [Google Scholar] [CrossRef] [PubMed]
[6]. Nonaka CF, Carvalho Mde V, de Moraes M, de Medeiros AM, Freitas Rde A, Desmoplastic fbroblastoma (collagenous fbroma) of the tongueJ Cutan Pathol 2010 37:911-14.10.1111/j.1600-0560.2009.01467.x19909389 [Google Scholar] [CrossRef] [PubMed]
[7]. Gonzalez-Moles MA, Ruiz-Avila I, Gil-Montoya JA, Collagenous fibroma (desmoplastic fibroblastoma) of the palate associated with Marfan’s syndromeOral Oncol EXTRA 2004 40:3910.1016/j.ooe.2003.12.004 [Google Scholar] [CrossRef]
[8]. Bhagalia S, Jain M, Pardhe N, Sireesha SK, Collagenous fbroma (desmoplastic fbroblastoma) of the oral cavityJ Oral Maxillofac Pathol 2012 16:277-79.10.4103/0973-029X.9908922923904 [Google Scholar] [CrossRef] [PubMed]
[9]. de Sousa SF, Caldeira PC, Grossmann Sde M, de Aguiar MC, Mesquita RA, Desmoplastic fibroblastoma (collagenous fibroma): A case identified in the buccal mucosaHead Neck Pathol 2011 5(2):175-79.10.1007/s12105-010-0239-621221866 [Google Scholar] [CrossRef] [PubMed]
[10]. Cazal C, Etges A, Almeida FC, de Souza SC, Nunes FD, de Arau jo VC, Collagenous fbroma (desmoplastic fbroblastoma) of alveolar bone: a case reportJ Br Pathol Med Lab 2005 41:185-88.10.1590/S1676-24442005000300008 [Google Scholar] [CrossRef]
[11]. Shimoyama T, Horie N, Ide F, Collagenous fbroma (desmoplastic fbroblastoma): a new case originating in the palateDentomaxillofac Radiol 2005 34:117-19.10.1259/dmfr/2242808315829696 [Google Scholar] [CrossRef] [PubMed]