Clear Cell Primary Seminal Vesicle Carcinoma in a Young Male-A Rare Case Report
Saurabh Gaur1, Bhavna Nayal2, Sunil B Pillai3, Padmaraj Hegde4, Arun Kumar Chawla5, Aseem Kapadia6
1 Registrar, Department of Urology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Udupi, Karnataka, India.
2 Pathologist, Department of Pathology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Udupi, Karnataka, India.
3 Associate Professor, Department of Urology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Udupi, Karnataka, India.
4 Professor, Department of Urology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Udupi, Karnataka, India.
5 Professor, Department of Urology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Udupi, Karnataka, India.
6 Registrar, Department of Urology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Udupi, Karnataka, India.
, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Padmaraj Hegde, Room No. 14, Urology OPD, Department of Urology and Renal Transplantation, Kasturba Medical College and Hospital, Manipal Academy of Higher Education, Manipal-576104, Udupi, Karnataka, India.
E-mail: padmaraj.hegde@manipal.edu
Primary malignancies of Seminal Vesicle (SV) are rare. When involved, it is most commonly due to secondaries or by contiguous spread from adjacent organs. Primary tumours that can arise in SV can be epithelial and mesenchymal. Adenocarcinoma is most common epithelial tumour, and the Clear Cell variant of Adenocarcinoma (CCA) so far has not been reported in literature. Primary SV malignancies like adenocarcinoma pose a diagnostic dilemma as it becomes difficult to differentiate it from secondaries or as involvement from other adjacent organs even with imaging, histopathology and Immunohistochemistry (IHC). Here we present a case of 34-year-old male who presented with occasional total painless haematuria for four years and was evaluated by Contrast Enhanced Computed Tomography (CECT) which revealed pelvic mass. After evaluation by biopsy, histopathology and IHC he was diagnosed as primary clear cell adenocarcinoma. Despite all investigations this malignancy is difficult to differentiate from mullerian duct cyst carcinoma.
Clear cell adenocarcinoma, Immunohistochemistry, Primary carcinoma
Case Report
A 34-year-old male came with complaints of occasional total painless haematuria for four years. He underwent enucleation of left eye for retinoblastoma at three years of his age. Patient also had childhood onset complex partial seizure disorder for which he was on oral anticonvulsant therapy (both phenytoin and phenobarbitone daily) for last 25 years. Digital Rectal Examination (DRE) disclosed a non tender mass bulging into the anterior wall, with overlying free rectal mucosa. To rule out prostate and colonic malignancies Serum PSA and CEA were done which were normal.
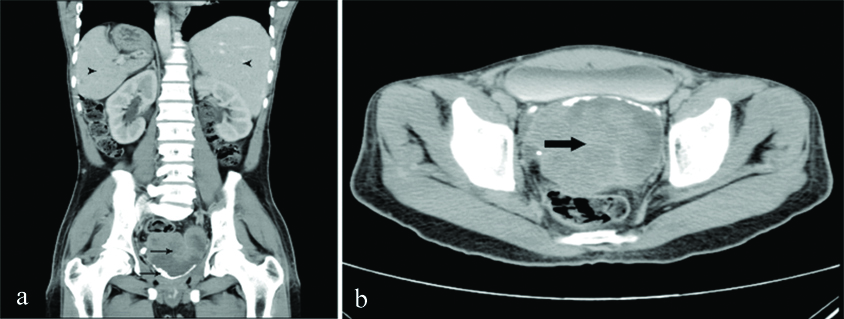
Initial evaluation with ultrasound abdomen and pelvis showed large mass in pelvis with mixed echogenicity which could not be separately delineated from prostate and SV. CECT abdomen and pelvis showed large lobulated heterogeneously mildly enhancing mass in retrovesicle region [Table/Fig-1a]. Prostate and SVs could not be separately visualized [Table/Fig-1b]. Situs inversus total is was noted on CECT [Table/Fig-1a]. MRI brain was done in background of past history of retinoblastoma and seizures which showed mesial temporal sclerosis with non specific white matter changes. EEG was normal. Sigmoidoscopy ruled out ant primary rectal or sigmoid colon growth. After taking consent, urethrocystoscopy was done which showed normal urethra and prostate with congested bladder and hyperemic areas in posterior wall and trigone of bladder without any obvious tumours. Transrectal Ultrasound (TRUS) guided biopsy and biopsy from the hyperemic areas in bladder both revealed nests and cords with intervening congested vessels, focal acinar pattern, lined by malignant columnar cells with moderate amount of clear cytoplasm, round to oval nuclei with anisonucleosis, prominent nucleoli, surrounded by fibrous stroma with mixed inflammatory infiltrate, areas of necrosis and haemorrhage, suggesting clear cell carcinoma [Table/Fig-2a,b].
On IHC, tumour cells were positive for CK7 [Table/Fig-2c], PAX8 [Table/Fig-2d] and negative for CK20, P63, CD10 and PSA, indicating its origin primarily from SV. All the options of treatment were explained to patient, and patient was planned for surgery and adjuvant treatment but was lost in follow up.
CECT abdomen and pelvis showed: a) large lobulated heterogeneously enhancing mass in retrovesicle region with linear calcifications in periphery (thin arrows), situs inversus totalis is seen with liver in left side and spleen on right (arrow heads); and b) Prostate and seminal vesicles are not separately visualised from the lesion (thick arrow).
Haematoxylin and Eosin staining showing clear cells in; a) low power (10X magnification); b) high power (40X magnification); c) Cytokeratin 7 (CK7) (40X); d) PAX8 immunoreactivity in tumour cells (40X).

Discussion
Primary malignancies are rare in SV. Commonly found tumours are usually secondaries from adjacent organs, most common being prostate [1]. Seminal Vesicle Carcinomas (SVC) include a variety of neoplasms ranging from sarcomas, and uncommon tumours comprising of stroma and mixed epithelial tissue. Although rare, in epithelial carcinomas, adenocarcinoma is the most common primary histotype [2], but a clear cell variant of adenocarcinoma is not reported in literature [3]. A case of CCA in the pelvic region in a young man with left renal agenesis has been reported but the organ of origin was not specified [2].
Since the first case of SVC was reported by Lyons O in 1925 [4], several diagnostic criteria have been laid for diagnosis of primary SVC. Criteria for diagnosis now contains, adenocarcinoma focus primarily in the SV with no associated tumour in prostate and the tumour in SV must be a papillary adenocarcinoma resembling the SV mucosa. In anaplastic SVC, production of mucous is essential to differentiate it from prostatic anaplastic carcinoma. Also negativity of SV malignancies for PSA, CEA and Prostatic Acid Phosphatase (PAP) helps to differentiate it from colorectal and prostate carcinomas [2,5].
PSVC can be observed in males of any age ranging from 13–90 years [5,6]. Obstruction of bladder outlet with or without haematospermia and haematuria is the most common symptom in SVC. Dysuria is also complained by about 35% of patients [3,7]. In about 30% of patients symptoms of obstruction are accompanied by painful sensation in the perineum and pelvis [7]. In our case a 34-year-old male presented with symptoms of occasional total haematuria for four years. DRE usually shows a palpable non tender tumour. Trigonal displacement or involvement is often detected at time of cystoscopy due to increased size of tumour [5]. However, about 30% of patients have no detectable abnormality on DRE and 20% have normal cystoscopic findings, here the lesion was found incidentally in Transurethral Resection (TUR) or during autopsy [7]. In our case patient had a non tender mass on DRE and cystoscopy revealed normal urethra and prostate but hyperemic areas were seen in bladder. On radiologic evaluation (CECT and TRUS), increase in gland size focally or a retrovesicle mass is found in almost all patients [5,7]. Our patient showed large lobulated heterogeneous mildly enhancing mass in retrovesicle region, from which prostate and SVs could not be separately visualized with normal sigmoidoscopic findings. To exclude carcinoma of rectum and for local staging sigmoidoscopy is highly recommended [7].
For histopathological diagnosis specimen can be collected by either TRUS guided fine needle biopsy or biopsy during endoscopic/open procedures [7]. IHC not only establishes the diagnosis of PSVC but also rules out tumours from adjacent organs [Table/Fig-3].
Immunohistochemical findings in adjacent organ carcinomas which may cause primary seminal vesicle adenocarcinoma and seminal vesicle.
| Immunohistochemical test | Seminal vesicleadenocarcinoma | Prostate cancer | Bladder cancer | Rectum cancer | Adenocarcinoma of theMullerian duct |
|---|
| CA 125 | + | - | - | - | +/- |
| Cytokeratin 7 | + | +/- | +/- | - | + |
| PSA | - | + | - | - | - |
| Cytokeratin 20 | - | +/- | +/- | + | - |
| CEA | +/- | - | - | + | +/- |
| PAX 8 | + | - | - | - | +/- |
PSA: prostate-specific antigen; CEA: carcinoembryonic antigen.
*Variations can be there in poorly differentiated or anaplastic tumours
Immunochemical staining, including a panel of CA-125, CK7, CK20, PSA, and PAP, are very useful in differentiating SVC from other tumours in that region, this is even more important when the only limited biopsy material is available for evaluation. Recently PAX8 and PAX2, because of their specific expression in tumours of wolffian, renal and Mullerian epithelial origins, are emerging as diagnostic markers for these tumours. PAX8 positivity in our case further supports our diagnosis. Despite this IHC malignant transformation in a mullerian duct cyst cannot be completely ruled out [8,9]. However, in our case the final diagnosis was based collectively on symptoms, clinical findings, imaging, histopathology, and IHC. The prognosis of SV adenocarcinoma is often poor due to delayed diagnosis and advanced presentation with survival rate less than 5% in three years [5,10,11]. Best chance of cure is offered by excision of the tumour with clear margins, approach for surgery can range from local excision of SV to more aggressive surgery, including retropubic prostaticovesiculectomy, cysto-prostaticovesiculectomy with urinary diversion and even pelvic exenteration [7].
Role of radiotherapy is in form of adjuvant treatment mainly in locally advanced disease or the presence of postoperative positive surgical borders or residual tumour [10,11]. There has been no definitive recommendation regarding the efficacy of chemotherapy and the chemotherapy regimen that should be used in primary SVC [5,7]. All the options of treatment were explained to patient, and patient is currently being planned for surgery and adjuvant treatment.
Conclusion
Primary SVC is a rare malignancy and CCA of SV is even rare and never been reported. The diagnosis is by combination of clinical, radiological, cystoscopic and histologic findings. IHC helped to distinguish it from other secondary malignancies and contiguous malignancies from adjacent organs. Though the prognosis remains poor, treatment for early PSVC is mainly complete surgical extirpation and RT/CT may have a role adjuvant and palliative setting.
PSA: prostate-specific antigen; CEA: carcinoembryonic antigen.
*Variations can be there in poorly differentiated or anaplastic tumours
[1]. Ramamurthy R, Periasamy S, Mettupalayam V, Primary malignancy of seminal vesicle: A rare entityIndian J Urol 2011 27(1):137-39.10.4103/0970-1591.7841721716878 [Google Scholar] [CrossRef] [PubMed]
[2]. Olivetti L, Laffranchi F, De Luca V, Cystosarcoma phyllodes of the seminal vesicle: a case report and literature reviewCase Reports In Urology 2014 2014:30270810.1155/2014/30270824639910 [Google Scholar] [CrossRef] [PubMed]
[3]. Santos GC, Silva SRMd, Faria EF, Coelho RDS, Scapulatempo Neto C, Pelvic clear cell adenocarcinoma in a young man: a case reportAppl Cancer Res 2009 :192-95. [Google Scholar]
[4]. Lyons O, Primary carcinoma of the left seminal vesicle1The Journal of Urology 1925 13(4):477-84.10.1016/S0022-5347(17)73588-4 [Google Scholar] [CrossRef]
[5]. Benson Jr RC, Clark WR, Farrow GM, Carcinoma of the seminal vesicleThe Journal of Urology 1984 132(3):483-85.10.1016/S0022-5347(17)49700-X [Google Scholar] [CrossRef]
[6]. Eken A, Izol V, Aridogan IA, Erdogan S, Acıkalın A, Tansug Z, An unusual cause of haematospermia: Primary adenocarcinoma of the seminal vesicleCanadian Urological Association Journal 2012 6(6):E259-E262.10.5489/cuaj.127 [Google Scholar] [CrossRef]
[7]. Thiel R, Effert P, Primary adenocarcinoma of the seminal vesiclesThe Journal of urology 2002 168(5):1891-96.10.1016/S0022-5347(05)64260-7 [Google Scholar] [CrossRef]
[8]. Warmann SW, Vogel M, Wehrmann M, Scheel-Walter HG, Artlich A, Pereira PL, Giant mullerian duct cyst with malignant transformation in 15-year-old boyUrology 2006 67(2):424:e3-e6.10.1016/j.urology.2005.09.00916461114 [Google Scholar] [CrossRef] [PubMed]
[9]. Tong G-X, Memeo L, Colarossi C, Hamele-Bena D, Magi-Galluzzi C, Zhou M, PAX8 and PAX2 immunostaining facilitates the diagnosis of primary epithelial neoplasms of the male genital tractThe American journal of surgical pathology 2011 35(10):1473-83.10.1097/PAS.0b013e318227e2ee21934480 [Google Scholar] [CrossRef] [PubMed]
[10]. Chhabra A, Bhullar S, Oberoi R, Chaturvedi A, Rao S, Primary adenocarcinoma of seminal vesiclesIndian Journal of Radiology and Imaging 2002 12(1):75-77. [Google Scholar]
[11]. Ormsby AH, Haskell R, Jones D, Goldblum JR, Primary seminal vesicle carcinoma: an immunohistochemical analysis of four casesModern Pathology 2000 13(1):46-51.10.1038/modpathol.388000810658909 [Google Scholar] [CrossRef] [PubMed]