Anastomotic urethroplasty and augmented urethroplasty are well established treatment for bulbar urethral strictures. Johanson’s staged urethroplasty is a time tested technique for managing penile, penobulbar and panurethral strictures. However, a reconstructive surgeon refines and evolves his technique with regular intervals, in the field of urethroplasty, through an audit of his results. We too reviewed our results and techniques and refined them where found lacking.
Materials and Methods
A retrospective review of records from 2012 to 2016 was done. A total of 90 patients underwent urethroplasty for anterior urethral strictures, of which 76 were available for follow up.
Twenty nine men underwent EEU and 14 underwent DO augmented urethroplasty for bulbar strictures while 33 underwent staged urethroplasty for penile/penobulbar/panurethral strictures. The surgeries were performed by multiple surgeons of the institute.
They were followed for a mean period of 21 months (range 1 to 48 months) with the help of RGU, MCU and UFR at three months, six months and one year. Cystoscopy was reserved for those who had recurrent symptoms or RGU/UFR was suspicious of recurrent stricture. There is a lack of consensus on follow up after any urethroplasty in literature. This protocol for follow up was chosen by us as it is minimally invasive, can be done on Out Patient Department (OPD) basis and had minimum cost bearing for our patients.
Success was defined as no obstructive symptoms and no recurrence in RGU, UFR or cystoscopy.
This being a retrospective analysis of pre-established surgical techniques and not an experimental trial, there are no ethical issues. Patient consent for using data and intraoperative images were taken. We have ensured that patient’s identity is not revealed anywhere in the article.
Results
Mean age of urethroplasty patients in all groups (on basis of urethroplasty types) was between 32 and 37 years (35.2 years). Score or Gartland and Werley demerit score.
Cause of Stricture
Stricture was of idiopathic cause in 32, due to straddle injury in 12, hypospadias surgery/instrumentation in 16, due to traumatic catheterisation in nine and lichen sclerosus in seven.
Site of Stricture
Most common site was bulbar urethra (43), less common was penobulbar/panurethral region (18) and least common was in penile region (15).
Length of Stricture
Stricture length was measured initially with RGU and confirmed intraoperatively. Average stricture length was 1.8 cm for EEU, 3 cm for augmented and 4.5 cm for staged urethroplasty.
Grafts
Buccal Mucosa (BMG) was used in all dorsal onlay (augmented urethroplasty) patients. Four patients with staged urethroplasty had prepucial grafts placed, while two had BMG placed, during Stage 1. One of the patients, who had a prepucial graft placed during Stage 1, had a BMG placed as inlay during tubularisation.
Success Rate
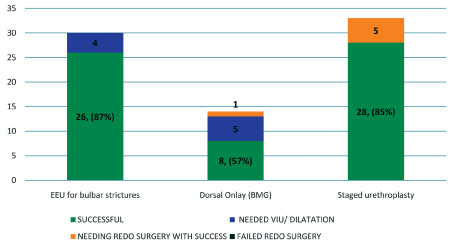
Success rate for EEU was 87%; 85% for staged urethroplasty and 57% for augmented urethroplasty [Table/Fig-1].
Graphical demonstration of success rate in each group.
Complications
Superficial Wound infection was seen in three patients and 5/33 (15%) stage urethroplasty patients developed urethrocutaneous fistulas.
Discussion
The term ‘Urethral stricture’ is specifically used for narrowing or obliteration of lumen of anterior urethra due to scarring of urothelium and/or corpus spongiosum [1]. Posterior urethral stricture is not included in the definition of ‘urethral stricture’. It is actually a distraction defect caused by avulsion secondary to pelvic fracture or radical prostatectomy and is called ‘Distraction Defect’ [1].
The mean age of stricture in males is third and fourth decade in most studies [1-4]. In the present study too, the mean age of patients in each group was between 32 and 37 years.
The most common causes of strictures in all recent studies are idiopathic and trauma. In the era of antibiotics, gonococcal infection as a cause of urethral stricture is infrequent [5]. Other causes include iatrogenic injury (traumatic catheterization, hypospadias surgery, instrumentation) and Lichen sclerosus [1,5]. The present study, too had similar observations.
Management of Bulbar Urethral Strictures
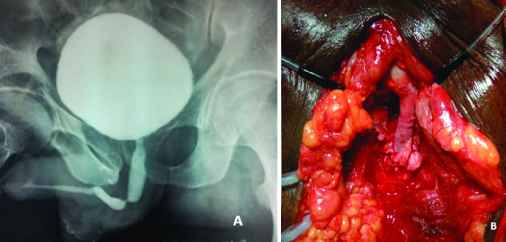
Anastomotic Urethroplasty (End-to-End Urethroplasty): Excision of scar and end-to-end anastomosis of bulbar urethra (anastomotic urethroplasty, EEU) is an accepted technique for management of strictures of 1-2 cm length [Table/Fig-2] [1,5].
a) Micturating cysytogram showing 1 cm tight stricture in proximal bulbar region; b) Anastomotic urethroplasty after excision of the stricturous segment.
However, many authors have successfully used EEU for strictures upto 4 to 5 cm long [1,5-7]. This can be accomplished by mobilisation of corpus spongiosum distally upto penoscrotal junction and if required, crural separation which straightens the curvature of bulbar urethra and bridges gap of upto 3 to 4 cm. In general, the closer the stricture is to membranous urethra, the longer it can be and still reconstructed by EEU [1]. It should be noted that excessive length of resection puts the patient at risk of penile shortening and cordee, which in turn affect the sexual function [1,5,6]. In the present study, average length of stricture in the group which underwent anastomotic urethroplasty was 1.8 cm which correlates with 1.8 cm mean length in study by Eltahawy EA et al., [4].
In the present study, success rate was comparable with that of Andrich DE et al., Kessler TM et al., and Martínez-Piñeiro JA et al., (p<0.05, Chi-square test) [Table/Fig-3] [9-11].
Comparison of our EEU results with other studies.
| Author | No. of patients | Avg. length | Success rate (%) |
|---|
| Eltahawy EA et al., [4] | 213 | 1.9 cm | 98.5 |
| Barbagli G et al., [8] | 20 | <2 cm | 95 |
| Andrich DE et al., [9] | 82 | - | 86 |
| Kessler TM et al., [10] | 40 | - | 86 |
| Martinez Piñeiro JA et al., [11] | 69 | <3 cm | 88 |
| Present Study | 29 | 1.8 cm | 86 |
We used Polyglactin 3/0 or 4/0 for anastomosis, depending upon the quality of tissue and space available, over 16 F silicon Foley’s catheter, with the knots on outer side. Some authors even describe taking knot inside the lumen [6]. Other sutures that can be used include PDS, Poliglecaprone and of size varying from 3/0 to 6/0 according to surgeon’s choice. Mucosal apposition is essential for successful outcome. All the four patients who had recurrence could be managed successfully with single Laser (Ho:YAG) Visual Internal Urethrotomy (VIU).
We exclusively use Laser VIU for recurrent post urethroplasty strictures. It has at least two advantages–a comparatively smaller (<21F) sheath can be used for Laser VIU and better tissue cuts.
Augmented Urethroplasty
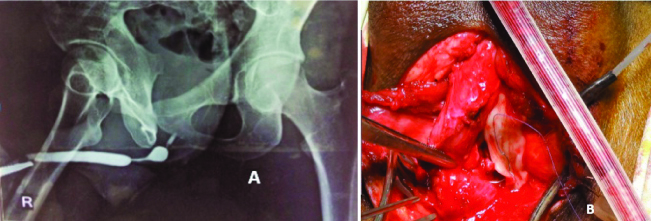
To overcome the shortcomings of EEU for long strictures, augmented and augmented anastomotic urethroplasty techniques are good options for strictures more than 2 cm long (average 3 cm in the present study) [Table/Fig-4] [5,6].
a) RGU showing a 2-2.5 cm stricture in mid bulbar urethra. Rest of the urethra appears normal. Contrast is seen proximal to the stricture; b) Augmented urethroplasty– stricturous bulbar urethra opened dorsally and Buccal Mucosal Graft sutured to the edges after fixation to corpora.
However, augmented urethroplasty is preferred only when there is minimal spongiofibrosis and patent urethral lumen of minimum 6 French (F) [5,6]. The stricturous urethra is opened either dorsally or ventrally (according to surgeon’s choice) and a graft is sutured to the defect to augment the urethral circumference. Equivalent success rates have been seen in most studies irrespective of which side the graft is placed, But ventral onlay of graft should be an option only when spongioplasty is possible [Table/Fig-5] [1,5,6,12,13].
Results of ventral vs. dorsal BMG augmentation urethroplasty.
| Study | Graft Location | No. of patients | Success rate |
|---|
| Barbagli G et al., [12] | Ventral | 17 | 83% |
| Dorsal | 27 | 85% |
| Abouassaly R et al., [13] | Ventral | 100 | 92% |
| Dorsal | 6 | 83% |
At our institute, we did a Dorsal Onlay in all cases of augmented urethroplasty and opened only the stricturous urethra without extending the incision for 1 cm into the healthy urethra.
Buccal mucosal graft is preferred by most surgeons as it has been found to have minimal donor site morbidity and good take [5,6]. Other alternatives are lingual mucosa (not preferred as thin graft obtained), retroauricular skin, prepucial or penile skin, and even bladder or colon mucosa [5,14]. The skin should be hairless or made so with the help of lasers because growth of hair inside the lumen causes obstruction and recurrent urinary infection. In the present study, buccal mucosa was used in all cases.
Dorsal onlay has been preferred by us as the graft is supported by corpora cavernosa and minimal mobility of graft is ensured [1]. The present study success rate with augmented urethroplasty was 57% (8 of 14 patients). The 4 (29%) patients with recurrent short segment stricture could be treated successfully with single Laser VIU bringing the long term success to 86%. The 1 (7%) patient had to undergo repeated laser VIU and the remaining 1 patient had to undergo redo augmented urethroplasty. All recurrences occurred within a year of surgery. Studies show that most recurrences in augmented urethroplasty, occur in the first two years of surgery [15-17].
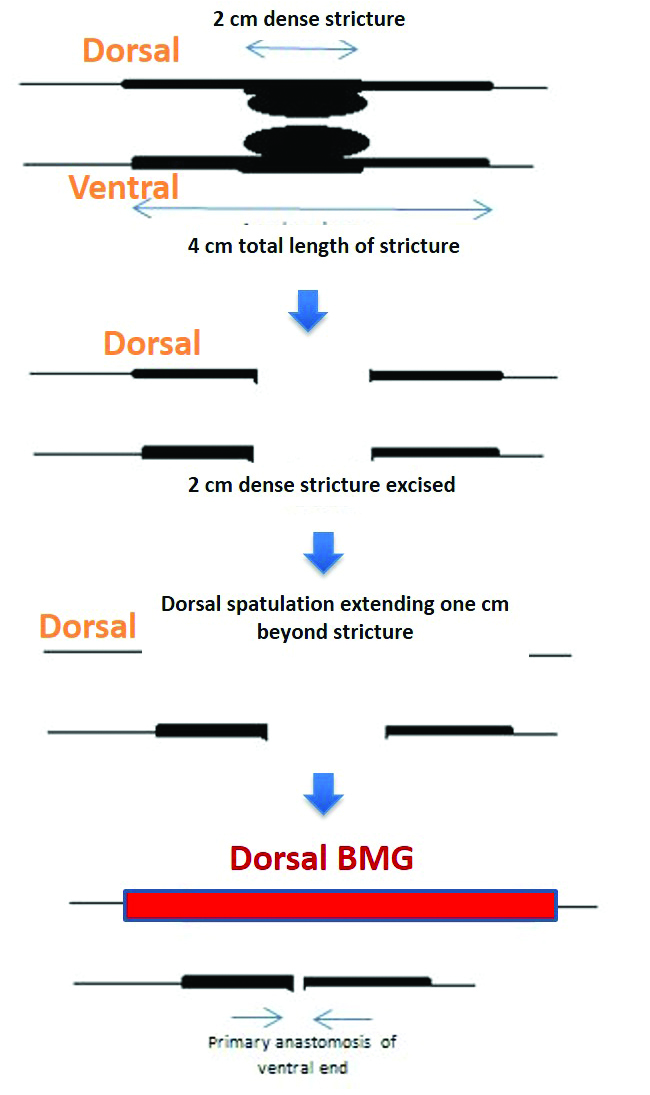
On retrospective analysis, literature also reflected similar findings. In 2004, Delvecchio FC et al., proposed that plain augmentation by dorsal onlay of buccal mucosa is less likely to be successful either because of deterioration of the transferred tissue exposed to urine or due to the fact that the onlay is performed in a densely spongiofibrotic area, which is unsuitable for simple onlay grafting [18]. He proposed using augmented anastomotic technique whenever possible for better results [12,18]. It involves resecting up to 2 cm of most scarred segment and spatulating the relatively less severe stricture proximally and distally on dorsal aspect. Primary anastomosis is done ventrally and a BMG placed dorsally as in augmented urethroplasty [Table/Fig-6].
Augmented anastomotic urethroplasty.
In 2006, Barbagli G et al., retrospectively reviewed their data and found that augmented urethroplasty had a relatively low primary success rate of 79% (75 of 95 patients) [12]. Furthermore, they concluded that there was formation of anastomotic ring strictures at the proximal and distal ends of graft because of graft retraction, ischemia, disease progression or suture material. This is the most frequent site of recurrence in augmented BMG urethroplasty and less common in the mid part [7,15]. An 80% such ‘ring recurrences’ in the present study 4/5 recurrences could be successfully treated with single VIU in the present study, bringing the success rate after single Laser VIU to 86%. In Barbagli’s study too, the success rate increased to 89.5% post VIU [12]. On statistical analysis, the primary success rate was significantly lower in the present study compared to Barbagli’s rates. (p=0.056) But after a single laser VIU, the difference in secondary success rate between present studies was not statistically significant. (p=0.75, Chi-square test) [Table/Fig-7].
Comparison of our augmented BMG urethroplasty results with that of Barbagli G et al., [12].
| Study | Primary Successn (%) | Failure | Success of single VIU in ring recurrences | Success rate after single VIU |
|---|
| Complete graft failure | Anastomotic ring strictures |
|---|
| Barbagli G et al., [12] (n=95) | 75 (79%) | 11 (11.6%) | 10 (10.5%) | 7/10 (70%) | 85/95 (89.5%) |
| Present study (n=14) | 8 (57%) | 1 (7%) | 5 (35.7%) | 4/5 (80%) | 12/14 (86%) |
VIU– Visual internal urethrotomy
Thus, successful treatment of ‘ring recurrences’ with single VIU increases the success rate of augmented urethroplasty in most series (94-100%) [8,16]. Rest of the patients requires redo urethroplasty retrospectively, we believe that extending the dorsal spatulation for 1 cm into the healthy urethra proximally and distally (to reduce ‘ring recurrences’ at proximal and distal ends) and using augmented anastomotic urethroplasty, instead of plain augmentation, in patients with severe spongiofibrosis, would have given us higher initial success rate. Abouassaly R et al., reported success rate of 90% with augmented anastomotic urethroplasty in 69 patients over eight years [19].
Management of penile and peno-bulbar strictures with staged urethroplasty
A staged urethroplasty is done for managing penile and penobulbar/panurethral strictures including lichen sclerosus patients (7 patients). Average length of stricture was 4.5 cm in the present study [Table/Fig-8].
a) Laid open peno-bulbar urethra after stage 1 (lay opening); b) Stage 2 (BMG inlay with Tubularisation) Urethral plate (24-28 mm) marked and incised; c) Urethral plate dissected free from surrounding skin. Dissection should not be carried deep to the urethral plate (medially), so as to maintain its vascularity. Urethral Plate is then incised in the midline. Incision is extended proximally into the neo- meatus; d) BMG placed as inlay; e) Final appearance of urethral plate after inlay; f) Tubularisation of urethral plate over 16 F Silicon Foley’s catheter.
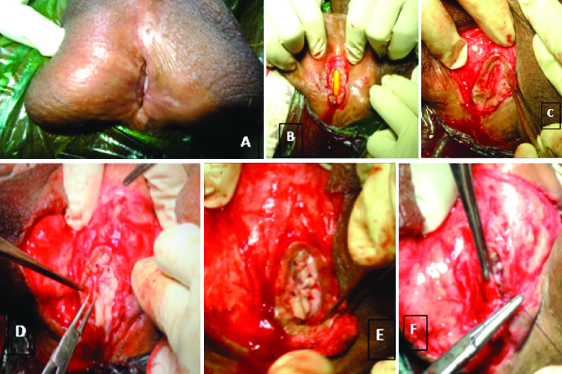
It involves laying open the stricturous urethra with an option of placing a graft when the unhealthy urethral tissue has to be excised (buccal mucosa or prepucial skin). After at least six months, once the urethral plate is healthy, it is tubularised over a silicon catheter (Johanson urethroplasty). We keep the width of urethral plate 22 mm. Kulkarni SB et al., have described a one stage pan urethral repair using BMG with a success rate of 91% in patients with mild to moderate Lichen sclerosus [20]. Asopa HS et al., has described a novel technique of dorsal free graft urethroplasty for urethral stricture by ventral sagittal urethrotomy approach in 2001 [21].
Though, recurrent stricture occurred in none, urethrocutaneous fistula/suture line dehiscence developed in 5/33 (15%) staged urethroplasty patients within six months of catheter removal. This was comparable with 13% rate in the study by Mori RL et al., the to found that fistula and suture line dehiscence were the most common complications seen in such cases [22].
All the patients were managed successfully with excision of fistula and urethral closure, which was covered with dartos and then skin.
The success rate of our staged urethroplasty was comparible with that of Mori RL and Angermeier KW and Kozinn SI et al., (p=0.26, chi square test) [Table/Fig-9] [22,23].
Our stage urethroplasty results in comparison to those of Mori RL and Angermeier KW and Kozinn SI et al., [22,23].
| Series | N | LS* (%) | Hypo^ (%) | Tub^^ (%) | >2 stages (%) | Recurrent stricture (%) | Urethrocutaneous fistula/dehiscence of suture line (%) |
|---|
| Kozinn SI et al., [23] | 91 | 31.9 | 45.1 | 56 | 26.4 | 9.9 | 0 |
| Mori RL and Angermeier KW [22] | 78 | 39.7 | 52.6 | - | 10.3% | 3.8 | 13 |
| Our study | 33 | 7 (21.2) | 24 | 100 | 9 | 0 | 15 |
Superficial wound infection, limited to skin and subcutaneous tissue, occurred in two patients. Both could be successfully managed with regular dressings and antimicrobials according to culture sensitivity report.
Patients in the present study, undergoing buccal mucosa grafting did not have any oral complications or symptoms.
Conclusion
Our results with EEU and staged urethroplasty are comparable with international studies; however augmented urethroplasty had lower success rates. Introducing augmented anastomotic urethroplasty instead of just augmentation for dense spongiofibrosis and extending dorsal spatulation into healthy urethra may improve our primary success for long bulbar strictures.