Laryngoscopy and endotracheal intubation is associated with transient increase in BP and HR due to reflex autonomic activity associated with stimulation of pharyngeal and laryngeal structures [1-3]. This reflex increase may be tolerated by a healthy individual, but in patients who are old and who already have previous Cardiovascular Diseases (CVD), sudden myocardial ischaemia or cerebrovascular accident may be precipitated [4]. Thus, it is important to blunt this reflex sympathetic activity during intubation.
Many drugs such as opioids, topical lignocaine, alpha and beta blockers, nitroglycerine and various airway management techniques have been tried which have been successful to some extent [5-12]. Studies have also been done on oral clonidine, given as premedication before surgery [13]. However, none of the above stated measures were fully successful in blunting the haemodynamic response to intubation completely. So, we decided to use intravenous clonidine in bolus form, before intubation, hoping that the peak effect of clonidine might be able to blunt the response. No previous study had tried to analyse the effect of intravenous clonidine in bolus form may be because of the fear of its adverse effects like bradycardia and hypotension.
Lignocaine is antiarrhythmic and clonidine has central sympatholytic action. Both have potentially promising effects in controlling the vasopressor response to laryngoscopy and intubation [13-15]. We gave these two drugs as intravenous premedication and measured BP and HR before and after intubation and compared the haemodynamic response. We also evaluated side effects associated with the use of these drugs (e.g., bradycardia and hypotension) and need for any rescue drugs.
Materials and Methods
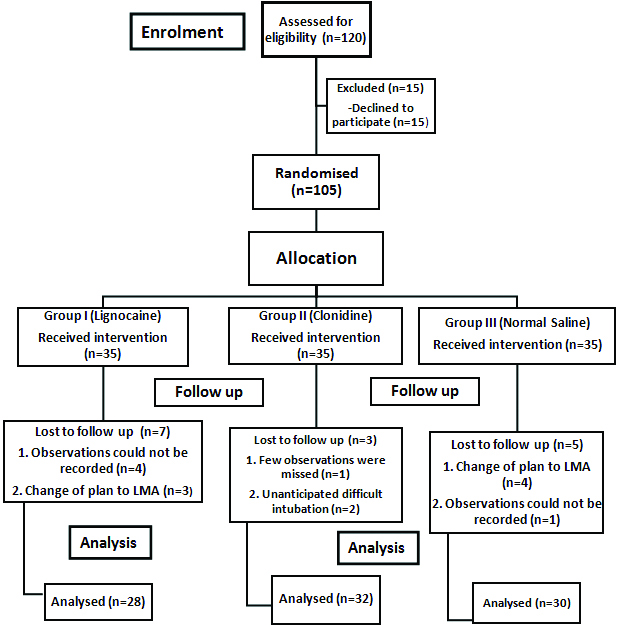
The study was a randomised controlled parallel trial with allocation ratio of 1:1. After the trial was commenced there was no change in methodology. The study was undertaken in the OT of Indian Spinal Injuries Centre, New Delhi, India (between March 2009 to April 2011). After performing routine preanaesthetic check-up, patients who met the eligibility criteria and the exclusion criteria were counselled regarding the study and those who gave the consent were included in the study. Inclusion criteria were, patients between the age group of 18-65 years, of either sex, ASA Grades I and II and Mallampati classes I and II, those scheduled for elective surgery and requiring oral intubation. Exclusion criteria were, patients of cervical spine injury, renal, hepatic, haematological diseases, patients with history of CVD such as brady or tachyarrhythmias, congestive heart failure and with history of cerebrovascular insufficiency. Patients having drug history of tricyclic antidepressants, chlorpromazine intake and those on clonidine, beta blockers, Calcium Channel Blockers (CCB) and those having temperature more than 98.6°F preoperatively and anticipated difficult airway were also excluded. The participant flow diagram is shown in [Table/Fig-1].
Flow diagram of participant flow.
Sample size was determined with the help of statistical software G-power. Alpha was taken as 0.05, minimum power as 80%, and effect size f as 0.4 (representing large difference in postintubation Mean Arterial Pressur (MAP) readings of NS, clonidine and lignocaine groups). The total sample size for three groups combined was calculated to be 66. Nevertheless, we initially enrolled 120 patients in the study and final outcome was noted in 90 patients.
The participants were randomised with the help of computer generated random number table and allocation concealment was done with sealed envelopes. These envelopes had a paper slip inside them, which had the group written on them. On the outside patient number was mentioned. Once the participant was received in the operating complex, the numbered envelope was handed over to an anaesthesiologist who was not a part of the study. He opened the envelope and prepared and administered the drugs according to the allotted group. Intubation and observations were recorded by a second anaesthesiologist.
The patient and the observer were blinded to the intervention given. The participants were divided into three groups; a) Lignocaine (Group-I) received 1.5 mg/kg of lignocaine iv. 90 seconds before laryngoscopy and intubation; b) Clonidine (Group-II) patients received clonidine 2 μg/kg iv. 30 minutes before laryngoscopy and intubation; c) Group-III (Control Group) participants received NS and served as control. All patients received 500 mL of NS 15 minutes before induction. General anaesthesia was induced with Inj. Thiopentone 5 mg/kg iv and muscle relaxation was achieved with Inj. Vecuronium 0.1 mg/kg iv. Inj. Fentanyl 2 μg/kg was given after intubation. Intubation was performed by a senior anaesthesiologist of at least five years experience to avoid bias. Anaesthesia was maintained using 66% Nitrous Oxide (N2O) and 33% of oxygen and 0.6% isoflurane.
The primary outcome of the study were Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), MAP and HR measured at baseline, preinduction and postintubation and the secondary outcomes were any instance of bradycardia and hypotension and need for any rescue drugs. Baseline readings i.e., at the time of shifting to OT complex were considered to be ‘0’ readings. Then after shifting to OT room and before the induction drugs were administered preinduction ‘1’ readings, thereafter, when the induction drugs were given–post-induction ‘2’ readings, then one minute after the laryngoscopy and intubation had been done postintubation ‘3’ readings, then at three minutes, five minutes and 10 minutes which were ‘4’, ‘5’, ‘6’ readings respectively.
Statistical Analysis
The SBP, DBP, MAP and HR within each group were analysed by Paired t-test. The intergroup comparison was done by ANOVA and DUNCAN multiple range test. SPSS version 22.0 was used to analyse the results. p-value of ≤0.05 was considered significant and value of ≤0.01 was considered very significant denoted by (*) and (**) respectively.
Results
A total of 120 patients initially gave their consent for participation in the study. However, on the day of surgery, 15 patients refused for enrolment. Subsequently, 105 patients were randomised into three groups. However, in lignocaine group outcome of seven patients was not analysed as in four patients, all observations were not recorded and in three patients, plan of anaesthesia was changed to Laryngeal Mask Airway (LMA). Similarly, in clonidine group three patients had to be excluded as observations were not recorded. Two patients had unanticipated difficult airway and intubation took lot of time. In control group four patients had a change of plan to LMA, and in one patient few observations were missed. So, they had to be excluded [Table/Fig-1]. The demographic profile of the patients who were finally analysed in the study has been shown in [Table/Fig-2].
| Comparison of two groups at baseline |
|---|
| Study group | Group I(Lignocaine) | Group II (Clonidine) | Group III (Control) |
|---|
| Age in years, (mean±SD) | 35.4±14.9 | 39.7±11.2 | 39.9±14.0 |
| Sex | Male | 18 (64.3%) | 24 (75%) | 16 (53.3%) |
| Female | 10 (35.7%) | 8 (25%) | 14 (46.7%) |
| ASA grade | I | 15 (53.57%) | 17 (53.1%) | 14 (46.7%) |
| II | 13 (46.42%) | 15 (46.9%) | 16 (53.3%) |
ASA: American Society of Anaesthesiologists
Systolic blood pressure: Upon analysing the SBP among the three groups, in Group III (control) the rise from baseline to postintubation at one minute, was from 123.26 to 160.66. Whereas, in clonidine group the rise was from a mean of 125.68 to 146.25. After clonidine administration, there was a slight fall in SBP for some time, however, intervention was not required in any patient. In lignocaine group, it was from 120.57 to 137.64. The difference was statistically significant and p<0.05. The [Table/Fig-3] shows the intergroup comparison of SBP and difference between baseline and postintubation readings at one minute for the three groups.
Comparison of systolic blood pressure among the three groups.
| SBP | Group 1 (Ligno) | Group 2 (Clon) | Group 3 (NS) | G1 Vs G2 | G1 Vs G3 | G2 Vs G3 | p-value |
|---|
| Mean±SD | Mean±SD | Mean±SD |
|---|
| SBP 0 | 120.5±14.94 | 125.6±14.07 | 123.2±11.64 | -- | -- | -- | 0.59 NS |
| SBP 1 | 123.0±15.86 | 117.5±12.56 | 133.6±15.01 | -- | -- | * | 0.01 S |
| SBP 2 | 114.3±13.92 | 113.7±15.75 | 121.2±8.07 | -- | -- | -- | 0.22 NS |
| SBP 3 | 137.6±20.47 | 146.2±19.47 | 160.6±17.95 | -- | * | * | <0.001 S |
| SBP 4 | 124.4±15.17 | 131.6±26.00 | 131.1±15.19 | -- | -- | -- | 0.55 NS |
| SBP 5 | 106.21±14.84 | 117.1±18.33 | 116.7±19.04 | -- | -- | -- | 0.032 S |
| SBP 6 | 103.21±16.34 | 106.06±16.64 | 107.4±12.84 | -- | -- | -- | 0.75 NS |
(Intergroup comparison) by Duncan’s multiple range test and ANOVA
‘*’ or ‘S’ denotes significant difference at p=0.05, NS: Normal Saline, SBP: Systolic Blood Pressure
Similarly, for DBP the rise in NS (control) group was from mean of 73.46 to 103.1. For lignocaine, it was from 73.64 to 87.5 postintubation. For clonidine, it was 79.43 at baseline readings. There after DBP fell in clonidine group to 73.37 after induction, till intubation when it rose again to 92.62. The rise in DBP was significantly higher in control group than with lignocaine and clonidine and p-value was 0.02 [Table/Fig-4].
Comparison of diastolic blood pressure among the three groups.
| DBP | Group 1 | Group 2 | Group 3 | G1 vs G2 | G1 vs G3 | G2 vs G3 | p-value |
|---|
| Mean±SD | Mean±SD | Mean±SD |
|---|
| DBP 0 | 73.64±8.72 | 79.43±8.55 | 73.46±11.01 | -- | -- | -- | 0.15 NS |
| DBP 1 | 74.14±13.46 | 71.37±11.36 | 73.80±10.12 | -- | -- | -- | 0.77 NS |
| DBP 2 | 72.35±10.58 | 73.37±15.42 | 72.40±11.97 | -- | -- | -- | 0.96 NS |
| DBP 3 | 87.50±16.26 | 92.62±14.28 | 103.06±13.97 | -- | * | -- | 0.02 S |
| DBP 4 | 78.07±13.39 | 82.25±21.75 | 80.26±10.66 | -- | -- | -- | 0.78 NS |
| DBP 5 | 64.14±15.31 | 71.87±17.17 | 69.06±21.04 | -- | -- | -- | 0.50 NS |
| DBP 6 | 61.57±16.20 | 67.37±19.05 | 60.46±13.27 | -- | -- | -- | 0.45 NS |
(Intergroup comparison) by Duncan’s multiple range test and ANOVA
‘*’ or ‘S’ denotes significant difference at p=0.05 DBP: Diastolic Blood Pressure, NS: Normal Saline
Similar trends were observed in MAP. The rise in MAP, one minute after intubation, in control group was much higher than both lignocaine and clonidine [Table/Fig-5].
Comparison of mean arterial pressure among the three groups.
| MAP | Group 1 | Group 2 | Group 3 | G1 vs G2 | G1 vs G3 | G2 vs G3 | p-value |
|---|
| Mean±SD | Mean±SD | Mean±SD |
|---|
| MAP 0 | 89.28±10.09 | 94.85±9.76 | 90.06±10.65 | -- | -- | -- | 0.072 NS |
| MAP 1 | 90.45±13.12 | 86.87±11.03 | 93.75±10.73 | -- | -- | -- | 0.071 NS |
| MAP 2 | 86.35±10.16 | 86.83±15.27 | 88.68±9.33 | -- | -- | -- | 0.85 NS |
| MAP 3 | 104.2±16.54 | 110.50±15.35 | 122.26±14.74 | -- | * | * | 0.01 S |
| MAP 4 | 93.52±13.46 | 98.70±22.54 | 97.22±11.46 | -- | -- | -- | 0.69 NS |
| MAP 5 | 78.16±14.63 | 86.97±16.83 | 84.95±19.71 | -- | -- | -- | 0.61 NS |
| MAP 6 | 75.45±16.02 | 80.27±17.76 | 76.11±12.20 | -- | -- | -- | 0.65 NS |
(Intergroup comparison) by Duncan’s multiple range test and ANOVA
‘*’ or ‘S’ denotes significant difference at p=0.05, MAP: mean arterial pressure, NS: Normal Saline
In case of HR, in NS and lignocaine groups it showed increasing trend from baseline till intubation and then gradually returned to normal. Clonidine was given 30 minutes before induction. At baseline level, it was 76.75 with σ17.05. Just after its administration, HR fell down. In four patients, it fell to below 50 beats/minute and 0.3 mg of atropine had to be administered to counter the fall. However, in no case any other intervention was required. Patients were sedated after clonidine administration and a gentle tap on the shoulder awoke them up and brought back the HR. The minimum HR that was seen was 42 beats/minute and that was seen in one patient. After intubation also, HR remained under control and no episode of bradycardia was seen in any patient [Table/Fig-6,7].
Comparison of heart rate among the three groups.
| HR | Group1 | Group2 | Group3 | G1 vs G2 | G1 vs G3 | G2 vs G3 | p-value |
|---|
| Mean±SD | Mean±SD | Mean±SD |
|---|
| HR 0 | 88.85±22.52 | 76.75±17.05 | 80.33±11.13 | -- | -- | -- | 0.027 S |
| HR 1 | 87.71±22.21 | 80.31±15.91 | 84.33±14.52 | -- | -- | -- | 0.274 NS |
| HR 2 | 98.07±22.09 | 89.37±13.59 | 96.80±12.27 | -- | -- | -- | 0.29 NS |
| HR 3 | 106.00±20.62 | 94.25±14.72 | 104.80±12.13 | -- | -- | -- | 0.009 S |
| HR 4 | 100.71±19.89 | 93.81±13.85 | 103.66±15.34 | -- | -- | -- | 0.057 NS |
| HR 5 | 98.92±18.92 | 88.37±12.31 | 93.46±11.83 | -- | -- | -- | 0.15 NS |
| HR 6 | 95.92±20.91 | 82.87±12.20 | 87.86±13.82 | * | -- | -- | 0.09 NS |
(Intergroup comparison) by Duncan’s multiple range test and ANOVA
‘*’ or ‘S’ denotes significant difference at p=0.05, HR: Heart Rate, NS: Normal Saline
Intergroup comparison of change in haemodynamic parameters.
| Group 1 | Group 2 | Group 3 | G1 vs G2 | G1 vs G3 | G2 vs G3 | p-value |
|---|
| Mean±SD | Mean±SD | Mean±SD |
|---|
| (SBP 0-SBP 3) | 17.07±17.31 | 20.56±20.71 | 37.40±11.98 | -- | ** | ** | 0.005S |
| (DBP 0-DBP 3) | 13.85±16.73 | 13.18±13.05 | 29.60±12.77 | -- | ** | ** | 0.003S |
| (HR 0-HR 3) | 17.14±13.45 | 17.50±12.92 | 24.46±14.69 | -- | -- | -- | 0.26NS |
| (MAP 0-MAP 3) | 14.92±16.27 | 15.64±14.42 | 32.20±11.12 | -- | ** | ** | 0.002S |
comparison done by DUNCAN multiple range test and ANOVA
‘**’ and ‘S’ signify significant difference at 0.01 level. HR-Heart rate; SBP-Systolic blood pressure; DBP-Diastolic blood pressure; MAP-Mean arterial pressure, NS: Normal Saline
Another important observation of the study was that after the initial rise of haemodynamic parameters in lignocaine and clonidine groups, the vitals returned to baseline levels earlier as compared to control group.
Postoperatively patients were observed for 24 hours and they remained stable. No case of hypotension, bradycardia and rebound hypertension was seen.
Discussion
Laryngoscopy and intubation are stressful noxious stimuli, which lead to reflex sympathetic activity and release of adrenaline and noradrenaline [1-3]. This sudden increase in neurotransmitter activity, leads to increase in BP, HR and tachyarrhythmia. In normal patients, who do not have cardiovascular or cerebrovascular diseases these responses can be tolerated, but in sick patients with CVD, such events may cause cerebral haemorrhage, left ventricular failure, and even myocardial ischaemia [4].
Studies have also been done on local anaesthetic lignocaine as iv agent as well as topical spray. It has antagonistic action on sodium channels of nerve fibres which decreases pain transmission to brain as well as has antiarrhythmic action by antagonising phase IV depolarisation in Purkinje fibres and ventricular muscles [14]. Clonidine on the other hand has central sympatholytic action. It acts on presynaptic alpha-2 receptors in Central Nervous System (CNS) and causes less release of sympathetic substances. This causes decreased vasopressor response during intubation. It also has slight sedative effect which contributes to its action.
In this study, we compared clonidine with lignocaine. There are many studies on these two drugs individually but a study comparing these two drugs alone are few [13,15]. Most of them have used a combination with other drug like fentanyl [16]. Secondly in most of the studies clonidine premedication has been given either as oral drug or as IV infusion. Although, both forms have shown good results to some extent, none of them have been fully successful. In our study, we used clonidine as IV bolus drug, in anticipation that we may get maximum effect in this form.
In a study done by Routray SS et al., a combination of intravenous fentanyl and clonidine (FC group) was compared to fentanyl-lignocaine (FL group) on attenuating intubation response. They enrolled total 40 patients with controlled hypertension. They found that haemodynamic parameters like HR and systolic, diastolic, and mean arterial blood pressure were altered to a similar level in both the groups before intubation and at one, three, and five minutes after intubation and they found that both the combinations were effective in decreasing the vasopressor response [16]. In the present study, also although BP and HR did increase after intubation but the rise was much less in comparison when neither of the two agents were employed (i.e., in NS control group). The reason for rise in BP and HR could be, that in our study we compared baseline readings noted in preoperative room with post intubation readings at first minute after intubation and there after up to 10 minutes. After the initial rise in haemodynamics post-intubation, the BP and HR quickly settled to normal [Table/Fig-3,4,5 and 6]. Secondly, in our study we used either lignocaine or clonidine alone and fentanyl was not used before induction, so that we could study the effect of either of them, since, fentanyl has been separately shown in studies to be capable of blunting the haemodynamic response [5-8]. In the above study, they have used combination of fentanyl with clonidine and lignocaine, which could have resulted in lower HR and BP readings. Also, in their study clonidine was administered just before induction and induction was done with propofol which reduces HR and BP, while in our study clonidine was administered 30 minutes before induction and induction was done by thiopentone and vecuronium which have minimal effect on BP and HR. However, the rise in parameters was much less in comparison to NS control group.
Another study comparing lignocaine and clonidine was done by Mohammadi SS et al., they compared clonidine 0.2 mg given orally 90 minutes before induction and intravenous lignocaine 1.5 mg/kg given just before induction. They also used fentanyl before induction, and induction was done by thiopentone and atracurium. They reported that, while HR was reduced in clonidine group, BP rose after intubation in both the groups, although the difference was statistically insignificant [17]. In the present study, we administered clonidine by iv route 30 minutes before induction and as previously mentioned fentanyl was not used before induction. This could be the reason for difference in HR response with clonidine in the present study. Other changes in vital parameters in both drugs were approximately similar to results of the present study and as previously stated clonidine and lignocaine produced almost similar results.
Marulasiddappa V and Nethra HN also compared the two drugs and they gave both the drugs by iv route just before induction. Lignocaine 1.5 mg/kg and clonidine 2 μ/kg. However, they reported significant attenuation of BP and HR response to intubation in clonidine group and reported better results in comparison to lidocaine [18].
Study done by Joshi VS et al., also had similar results. They also reported effective response from both clonidine and lignocaine [19].
Limitation
The major limitation of the present study was that, during induction, N2O or inhalational agents were not used. Neither any IV narcotics administered. Intubation was done three minutes later. This might have affected the intubation response. However, this methodology was used in all patients including NS control group, so we can say that intergroup comparison between lignocaine and clonidine is still valid. Secondly, BP was measured non-invasively. However, since present patients were ASA Grade I and II and were undergoing minor or moderate surgeries, we found it ethically unjustifiable to put arterial cannula in such patients and expose them to unnecessary pain.
In the future, studies can be done on dexmedetomidine, which is very similar to clonidine in action. It has sedative and analgesic effects apart from producing central sympatholysis.
Conclusion
Both clonidine and lignocaine can be used in routine anaesthesia practice for blunting the haemodynamic response. Lignocaine maintains haemodynamics around baseline better than others, but if adequate monitoring is available, clonidine can be also used freely. Every possible effort should be made to maintain haemodynamic stability during laryngoscopy and intubation.
ASA: American Society of Anaesthesiologists
(Intergroup comparison) by Duncan’s multiple range test and ANOVA
‘*’ or ‘S’ denotes significant difference at p=0.05, NS: Normal Saline, SBP: Systolic Blood Pressure
(Intergroup comparison) by Duncan’s multiple range test and ANOVA
‘*’ or ‘S’ denotes significant difference at p=0.05 DBP: Diastolic Blood Pressure, NS: Normal Saline
(Intergroup comparison) by Duncan’s multiple range test and ANOVA
‘*’ or ‘S’ denotes significant difference at p=0.05, MAP: mean arterial pressure, NS: Normal Saline
(Intergroup comparison) by Duncan’s multiple range test and ANOVA
‘*’ or ‘S’ denotes significant difference at p=0.05, HR: Heart Rate, NS: Normal Saline
comparison done by DUNCAN multiple range test and ANOVA
‘**’ and ‘S’ signify significant difference at 0.01 level. HR-Heart rate; SBP-Systolic blood pressure; DBP-Diastolic blood pressure; MAP-Mean arterial pressure, NS: Normal Saline