Idiopathic Retroperitoneal Fibrosis (RPF) is a disease of unknown aetiology, characterised by extensive periaortic sclerosis. A subset of idiopathic RPF is found to be associated with Immunoglobulin G4-Related Disease (IgG4-RD) which is also designated as Multisystem Fibro Inflammatory Disease (MFID). IgG4-RD is an emerging immune mediated disorder of unknown aetiology being increasingly appreciated in recent times. This disorder encompasses a spectrum of disorders involving more than one organ system and shares a common pool of clinical, serological and pathological features. There are few clinical, radiological, pathological and treatment response differences found between the subset of idiopathic RPF that is associated with IgG4-RD and the rest without IgG4-RD association. Here we present a case of MFID with a rare combination of idiopathic RPF causing bilateral ureteral encasement, large bowel obstruction and gross pericardial effusion.
Benign, Ceroid, Malignant, Retroperitoneal fibrosis
Case Report
A 35-year-old female presented to the surgery outpatient department with complaints of abdominal distension, reduced appetite and fatigue since last six months. On examination, the abdomen was distended, with no tenderness or palpable mass. Laboratory tests showed microcytic hypochromic anaemia and leucocytopenia.
Contrast Enhanced Computed Tomography (CECT) of the patient was performed with Multislice CT Machine (16 slice Brilliance-DS Philips Machine, Netherlands).
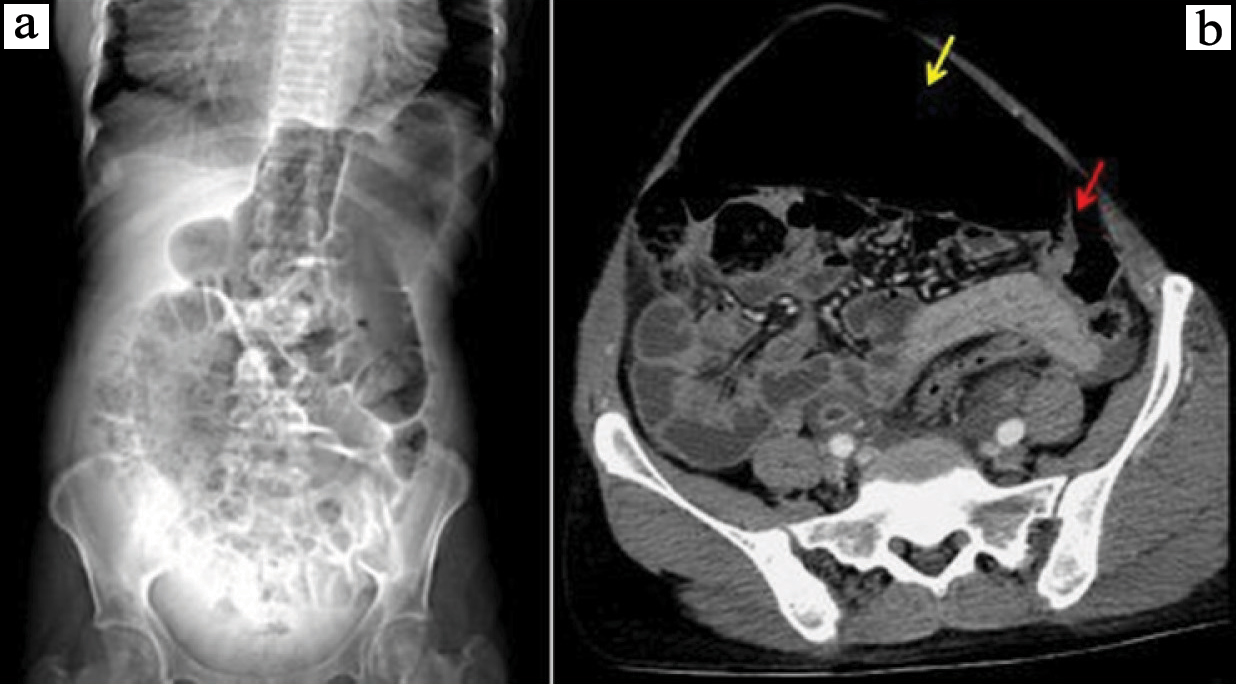
It was a triple phase helical CT study done with 100 mL of low osmolar contrast agent with 350 mg iodine/mL, injected at 4 mL/sec, with pitch of 1.375:1, thickness of 5 mm and 120 kV. Multiplanar reconstruction was done in 3 mm thickness. The study showed bilateral symmetrical retroperitoneal soft tissue density lesions with minimal contrast enhancement on 15 minutes delayed scans, extending from the level of renal hilum down till vesicoureteric junction, encasing the ureters and iliac vessels on both the sides. Thin strip of lesion was bridging the bilateral periureteral lesions anteriorly at the level of aortic bifurcation. Mild bilateral hydronephrosis and hydroureters were noted with thickened and enhancing walls of pelvicalyceal system and ureters which are likely secondary to distal obstruction by periureteral lesion and possible superimposed infection. Diffusely thickened and irregular urinary bladder wall was seen probably representing chronic cystitis [Table/Fig-1,2,3 and 4].
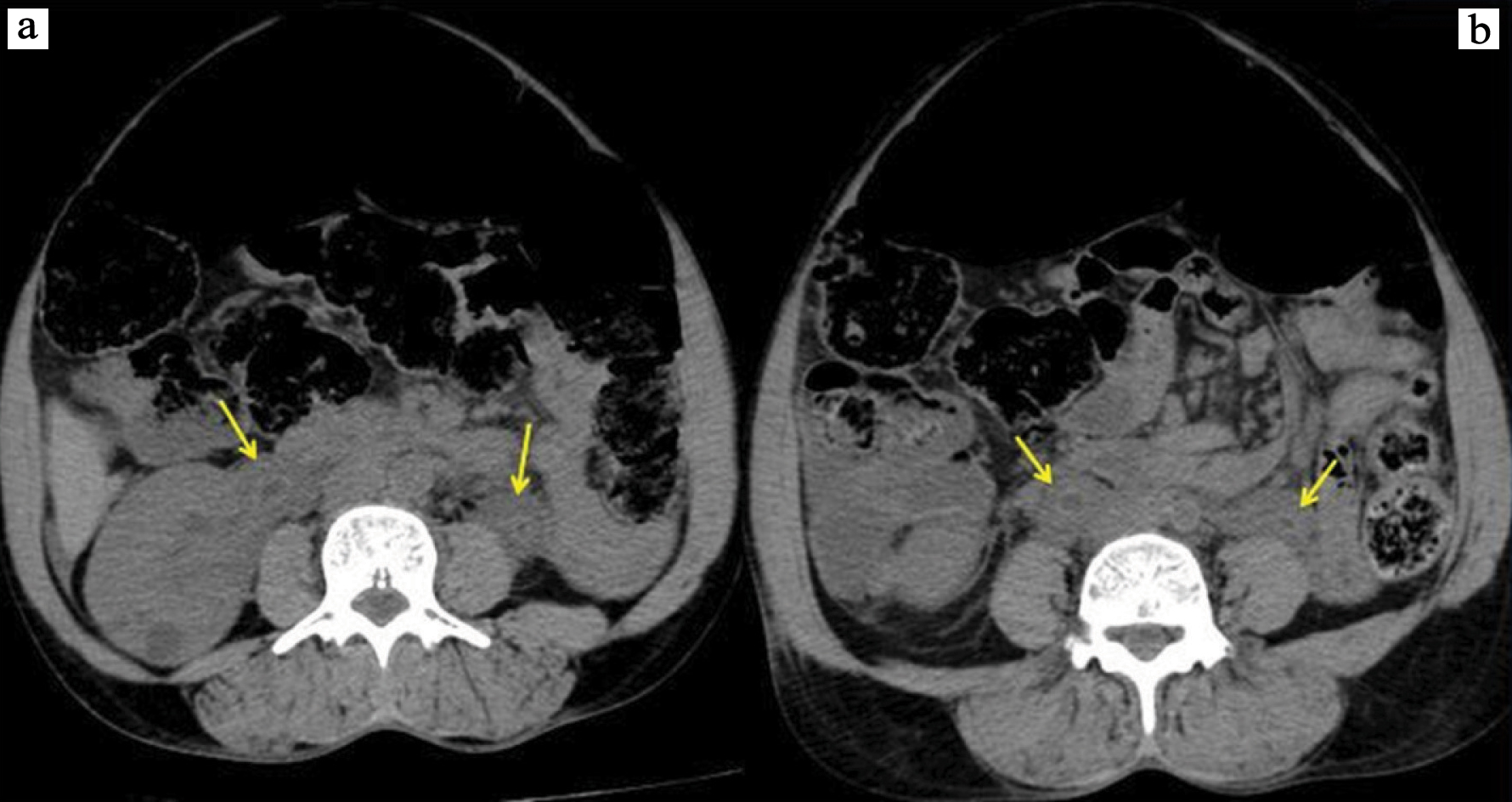
a) Non contrast abdominal CT axial view, showing bilateral periureteric soft tissue density lesion (yellow arrow) at the level of renal hilum; and b) mid ureter.
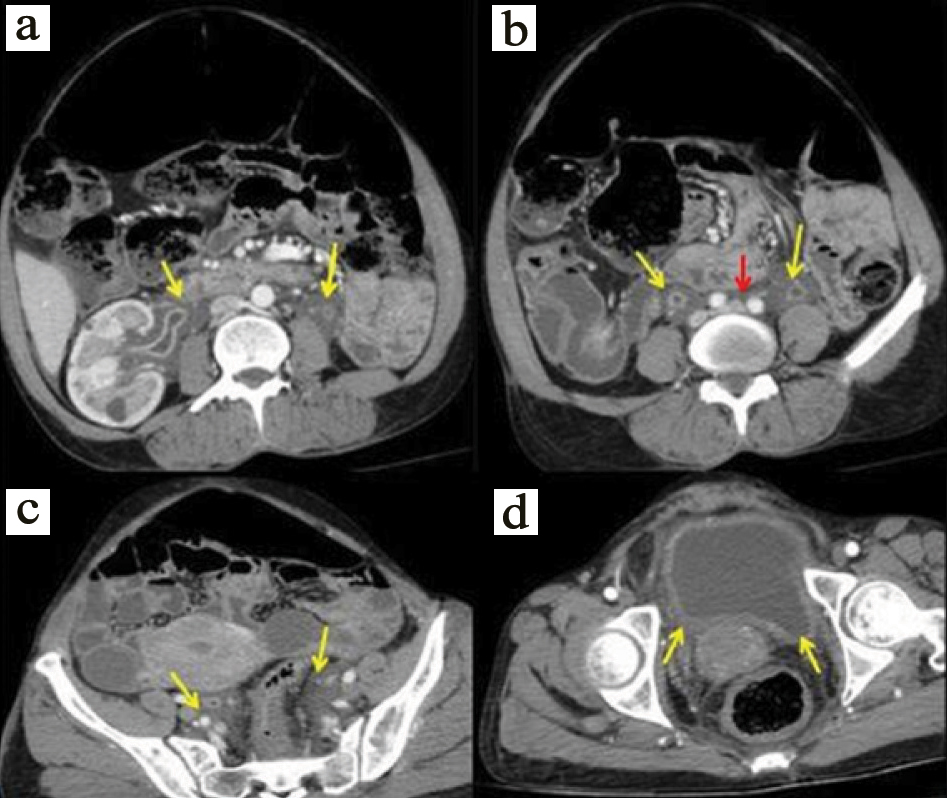
a) Post contrast abdominal CT axial view in venous phase showing non- enhancing soft tissue density lesion surrounding bilateral renal pelvis and ureters showing enhancing wall (yellow arrow) at the level of renal hilum; and b) mid-ureter with thin rim of bridging tissue anterior to aorta (red arrow); c) partial encasement of iliac vessels; and d) diffusely thickened urinary bladder wall.
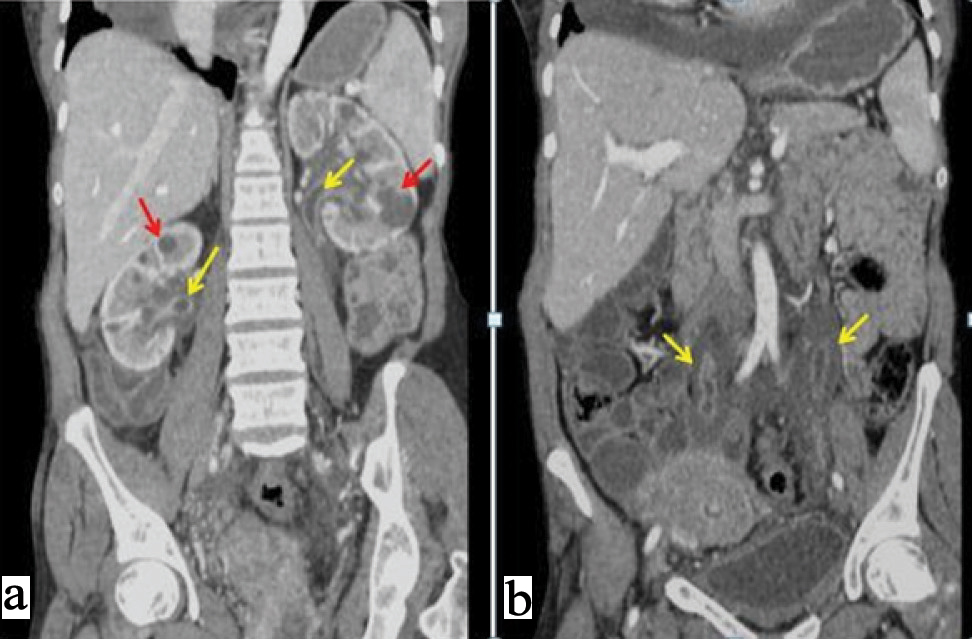
a) Post contrast abdominal CT coronal view in venous phase showing non enhancing soft tissue density lesion surrounding bilateral renal pelvis and ureters showing enhancing wall (yellow arrow) at the level of renal hilum; b) mid-ureter and multiple bilateral renal cysts (red arrows).
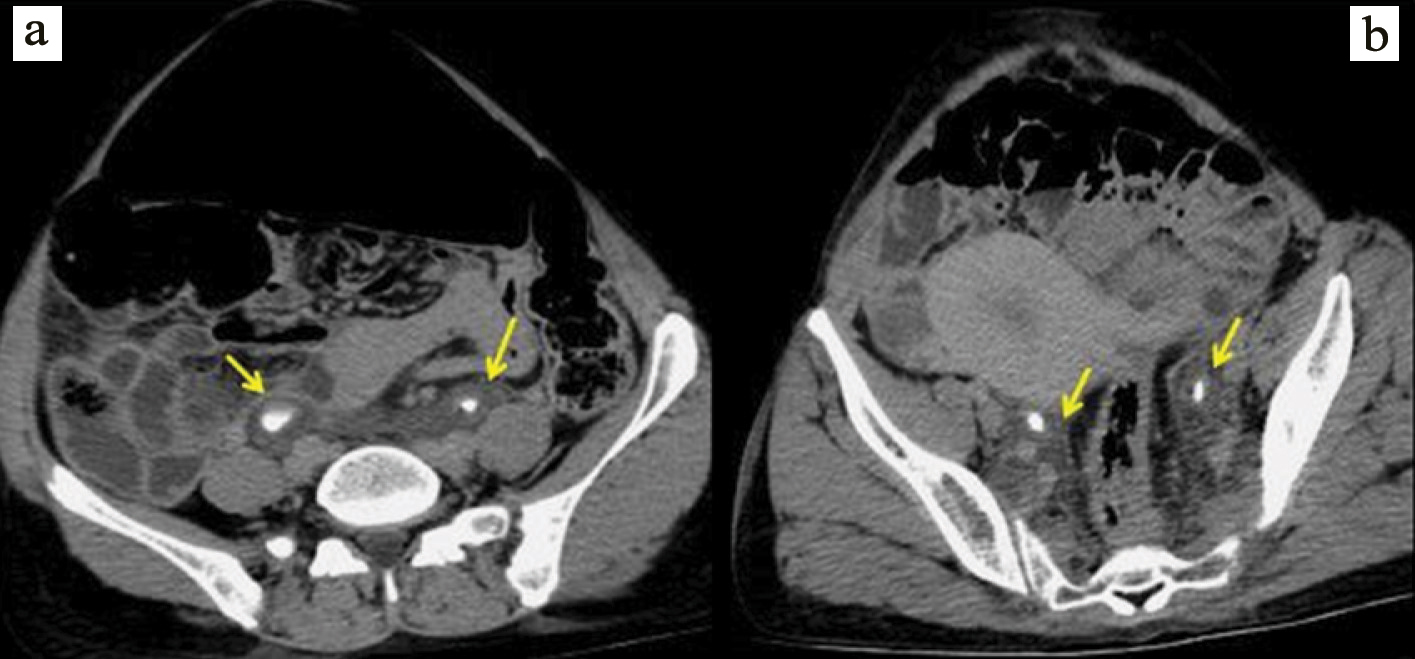
a) Post contrast abdominal CT, 15 minutes delayed scan axial view showing minimal inhomogeneous enhancement of soft tissue density lesion surrounding bilateral renal pelvis and ureters (yellow arrow) at the level of renal hilum; b) mid-ureter.
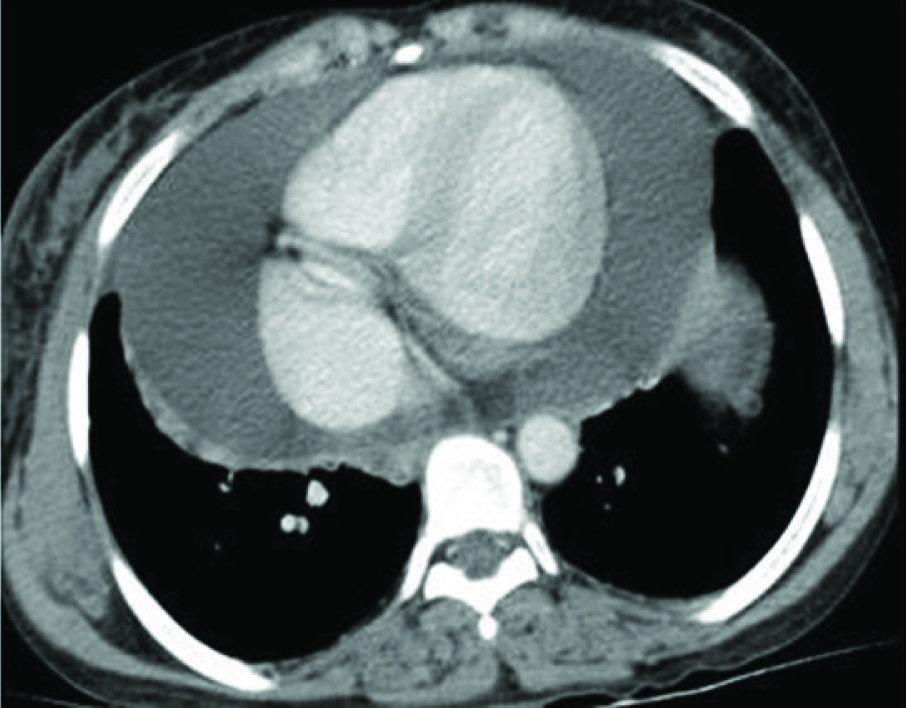
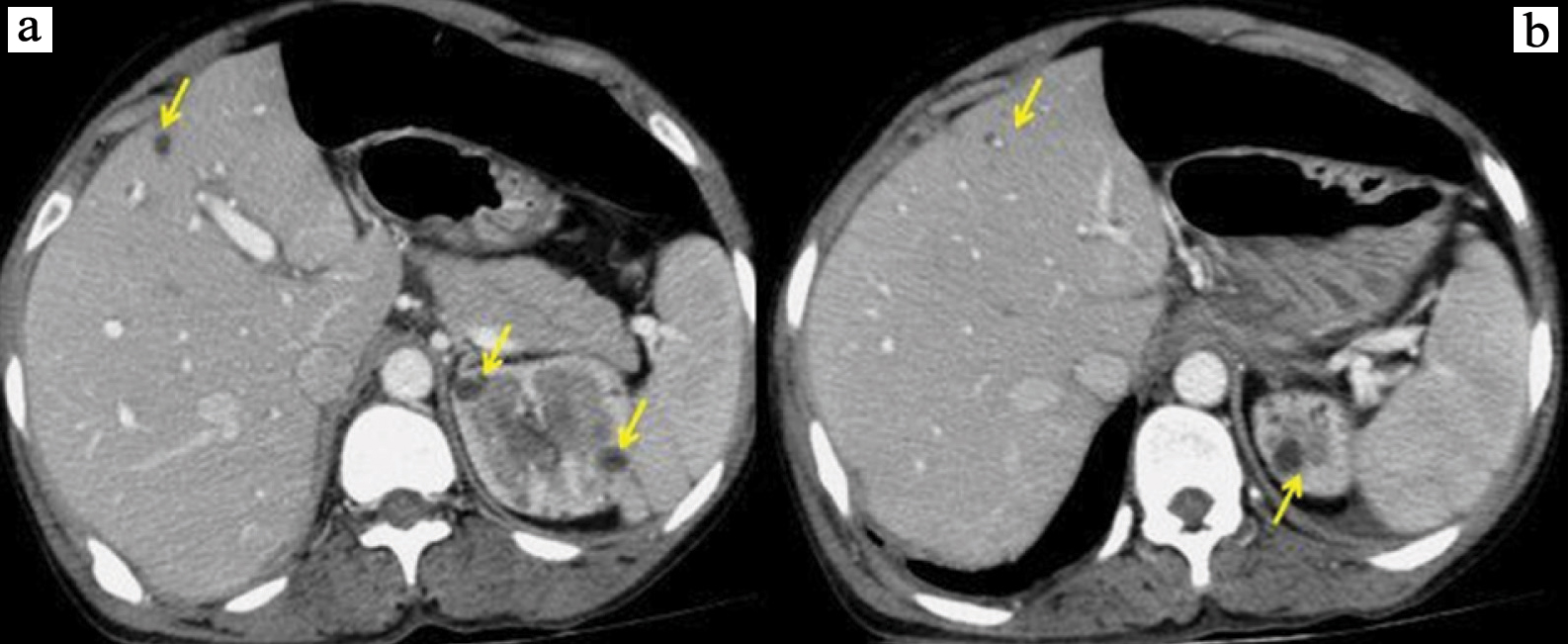
Abnormal distension of ascending colon and transverse colon with gross dilatation of the transverse colon were seen with a short segment circumferential smooth wall thickening of distal end of transverse colon causing partial luminal narrowing [Table/Fig-5a,b]. Gross pericardial effusion with diffusely thickened pericardium [Table/Fig-6], multiple simple hepatic and renal cysts [Table/Fig-3a,b,7a,b], minimal ascites and bulky uterus was noted.
a) Scanogram showing grossly dilated transverse colon; b) Post contrast abdominal CT axial view in venous phase showing grossly dilated transverse colon (yellow arrow) and a short segment circumferential wall thickening of distal end of transverse colon (red arrow).
Post contrast chest CT axial view showing gross pericardial effusion with thickened pericardium.
(a,b) Post contrast abdominal CT axial view in venous phase depicting multiple small, non enhancing hepatic and renal cysts.
Differential diagnosis considered was benign or malignant RPF, perianeurysmal fibrosis and primary amyloidosis. In case of malignant type of “RPF”, the mass is commonly seen posterior to aorta and inferior vena cava causing mass effect and displacing them anteriorly. The margin of the lesion usually show nodular pattern and the superior extent of the lesion is higher than the renal hilar level. Lesion always shows enhancement with contrast. In contrast, the benign or idiopathic type of RPF shows sparing of retroaortic region, smooth margin of the lesion, common infra renal hilar involvement and presence of enhancement only in the early and active stages, as seen with this patient.
Though the extent, density and enhancement of the lesion in perianeurysmal fibrosis are same as benign RPF, it was ruled out as there was no dilatation of the involved aortic segment, which is commonly seen in this entity. The other condition which could present with the similar CT findings, namely primary amyloidosis was ruled out as the patient did not have any other manifestations of primary amyloidosis.
Since, there was extra-retroperitoneal involvement of large bowel and pericardium, MFID was considered; patient’s serum IgG4 was done, which was found to be abnormally high. As the patient was hesitant to undergo any invasive test, biopsy could not be performed for confirmation of the same. Final diagnosis made was Idiopathic RPF with possible association of IgG4 related immune mediated disease, i.e., MFID.
As the patient was not willing for surgical management, she was started on steroids for fibrosis and antibiotics for urinary infection.
Discussion
Multisystem fibro-inflammatory disease, a synonym of IgG4-RD, is an emerging immune mediated disorder of unknown aetiology. This disorder encompasses a spectrum of disorders involving multiple systems and shares a common pool of clinical, serological and pathological features [1,2]. Common presentations of IgG4-RD includes Type-1 autoimmune pancreatitis, sclerosing sialadenitis, involvement of lacrimal gland and major salivary glands, earlier known as Mikulicz syndrome, isolated submandibular gland enlargement previously named as Küttner’s tumour, orbital pseudo-inflammatory disease and RPF. IgG4-RD commonly manifests in male gender in middle to old age, though the disease of head and neck is seen equally in both gender [2].
The IgG4-RD is diagnosed on Histopathology (HP) and immunohistochemistry. IgG4-positive plasma cells and lymphocytes infiltration, storiform pattern of fibrosis with eosinophilia and obliterative phlebitis are found on HP. Raised serum IgG4 levels, (>135 mg/dL) is a characteristic but not a diagnostic finding. Increased blood plasmablast concentration is more convincing finding than raised IgG4 levels in making the diagnosis and also in assessing the activity of the disease process [1,2].
The RPF is one of the common components of IgG4-RD, where there is extensive fibrosis throughout the retroperitoneum. Common presentation of RPF is pain in abdomen and back, weight loss and constipation. Inflammatory reaction to the ceroid and lipoproteins in the plaques of atherosclerosis has been proposed as the underlying pathogenesis of RPF [3]. Methysergide intake is the well established cause of RPF, however majority are idiopathic in origin, which are now a part of IgG4 related disease. The subset of idiopathic RPF associated with IgG4-RD are found to present with other organ system involvement, though Idiopathic RPF also occurs as isolated entity. Characteristic HP features of IgG4-RD and relatively good response to glucocorticoids are also observed with this entity in comparison with the RPF without IgG4 association [1,2].
In case of RPF with or without IgG4-RD association, radiological investigations have been found to depict the condition and its extent. Fibrosis in RPF is generally seen to be caudal to the aortic bifurcation from the renal hilum to the vesicoureteric junction showing enhancement with contrast in acute stages and no enhancement in chronic stages [4,5]. CT is found helpful in finding the thoracic manifestations of systemic fibro-inflammatory disease i.e., a subset of idiopathic RPF with positive IgG4-RD. Commonly reported thoracic manifestations are pleural effusion and evidence of chronic pericarditis with gross pericardial effusion. Very few cases of idiopathic RPF associated with IgG4-RD have been reported with either small or large bowel obstruction secondary to bowel wall fibrosis [6].
The management of MFID is based on the organs involved and the presenting features. Initially conservative management is considered and glucocorticoids play the main role. Generally in few weeks the response is clinically evident and the steroid is tapered over time. In situations where patient has contraindication to usage, poorly responsive or not responding to gucocorticoids and for patients who show relapse after discontinuation of steroids, B cell depletion therapy with rituximab is being tried. However, a randomised trial for rituximab usage in patients with IgG4-RD is still awaited. In patients whose symptoms are not relieved by medical management or severe enough to demand an immediate intervention, minimally invasive surgical treatments done based on the organ system involved [2]. In case of patients presenting with RPF, the aim of management is to cease the symptoms caused due to encasement of the ureters and the procedures employed are ureteric stenting and ureterolysis. For large bowel obstruction if not relieved with medications, laproscopic/open surgery is recommended. Non responding pericardial effusions are managed with therapeutic tapping.
The present case was unique with predominant periureteric involvement by RPF with resultant bilateral hydroureteronephrosis and the copresence of massive pericardial effusion and large bowel obstruction rising the suspicion of MFID i.e, IgG4 related RD. In the best of our knowledge, this is the first case with this kind of combined presentation in the literature.
Conclusion
Multisystemic fibro-inflammatory disease/IgG4 RD is an emerging entity, which connects the multiple organ and system diseases through common clinical, serological and pathological features. A subset of idiopathic RPF is associated with IgG4 RD and is found to be differing from rest of cases by showing relatively good response to medical treatment. Recognition of this entity is essential to identify patients, who will show better response to medical treatment and to prevent poor outcome due to disease progression.
[1]. Arezou K, Carruthers M, Stone J, Shinagare S, Sainani N, Hasserjian RP, Rethinking ormond’s disease “idiopathic” RPF in the era of igg4-related diseaseMedicine 2013 92(2):82-91.10.1097/MD.0b013e318289610f23429355 [Google Scholar] [CrossRef] [PubMed]
[2]. Moutsopoulos HM, Fragoulis GE, Stone JH, Overview of IgG4-related diseaseUpToDateAvailable in: http://www.uptodate.com/contents/overview-of-igg4- related-disease#. Last updated: August 16, 2016. (Accessed on 03 Aug 2017) [Google Scholar]
[3]. Parums DV, Brown DL, Mitchinson MJ, Serum antibodies to oxidized low density lipo-protein and ceroid in chronic peri-aortoritisArch Pathol Lab Med 1990 114(4):383-87. [Google Scholar]
[4]. Cronin CG, Lohan DG, Blake MA, Roche C, McCarthy P, Murphy JM, RPF: a review of clinical features and imaging findingsAm J Roentgenol 2008 191(2):423-31.10.2214/AJR.07.362918647912 [Google Scholar] [CrossRef] [PubMed]
[5]. Caiafa R, Vinuesa A, Izquierdo R, Brufau B, Colella J, Molina C, Retroperitoneal fibrosis: role of imaging in diagnosis and follow-upRadiographics 2013 33(2):535-52.10.1148/rg.33212508523479712 [Google Scholar] [CrossRef] [PubMed]
[6]. Aziz F, Conjeevaram S, Phan T, RPF: a rare cause of both ureteral and small bowel obstructionWorld J Gastroenterol 2006 12(43):7061-63.10.3748/wjg.v12.i43.706117109508 [Google Scholar] [CrossRef] [PubMed]