Balanced anaesthesia comprises of muscle relaxation as an essential component in addition to analgesia, amnesia and areflexia. The beginning of use of muscle relaxants and understanding their pharmacology heralded a new era in the growth of fields of anaesthesia and surgery [1]. Non depolarising muscle relaxants competitively bind to the alpha subunit of acetyl choline receptors at the neuromuscular junction to produce muscle paralysis [2]. Long acting relaxants like pancuronium used by Baird WL and Reid AM as well as intermediate acting agents like vecuronium and atracurium brought about a revolution in the field of anaesthesia [3,4].
Monitoring of neuromuscular function is a significant advancement in the world of muscle relaxants. It is recommended by authors due to varied responses to relaxants and narrow dose ranges [5]. Studies have shown that without the use of neuromuscular monitoring upto 42% of patients show signs of inadequate reversal in the recovery room [6]. Atracurium has been in clinical use since 1980 [4]. It is a bis benzyl tetrahydroisoquinoline which is eliminated by Hofmann degradation. The marketed product has 10 isomers which include cis-cis, cis-trans, trans-trans depending upon configuration. Atracurium has a significant advantage over other neuromuscular blocking drugs due to its spontaneous degradation and non-organ dependent elimination leading to its safety in geriatric and organ failure patients. However, histamine release and haemodynamic instability are its major limiting factors [7,8]. Cisatracurium, introduced in 1995, however has minimal propensity to release histamine and has a higher autonomic stability. It constitutes 15% of the commercially available atracurium mixture and produces three to four times more potent block than atracurium [9]. In the present study, primary aim was to compare the onset time, duration of block and recovery index of the two drugs. The secondary aim was to compare the haemodynamics and monitor signs of histamine release.
Materials and Methods
A randomised prospective observational study was conducted in the Department of Anaesthesia, Government Medical College, Amritsar, Punjab, India (from December 2016 to March 2017 on 60 ASA). American Society of Anaesthesiologists (ASA) Grade I and II patients between the age group of 18-65 years who were scheduled for elective laproscopic cholecystectomies. After approval from the Institutional Ethical Committee, an informed written consent was obtained and a thorough preoperative evaluation of the patients was done. Patients who were less than 18 years or above 65 years, had an ongoing pregnancy, ASA grade III or more, had Body Mass Index (BMI) >30 kg/m2, with anticipated difficult airway, had a history of neuromuscular diseases, had to undergo emergency surgeries and who refused for consent were excluded from the study.
All patients underwent thorough preoperative checkup through relevant history, general physical examination, systemic examination and airway assessment. Demographic data including age, sex, weight, height, ASA status and BMI were collected. Patients were randomly divided into two groups of 30 each, Group C and Group A. Group C received 0.1 mg/kg cis atracurium while patients in Group A received 0.5 mg/kg atracurium as neuromuscular blocking agent. Computer generated programme was used to generate sample size in both the groups. Relevant investigations were done after which routine fasting guidelines and anti aspiration prophylaxis were given.
In the operating room all the multiparameter monitoring including Heart Rate (HR), Non-Invasive Blood Pressure (NIBP), Oxygen Saturation (SpO2), Capnography (EtCO2) and Temperature (T) probe were attached to the patient. A baseline HR, BP and oxygen saturation were recorded. Intravenous access (i/v) was established and fluids started. All the patients were premedicated with injection butorphanol 1 mg IV and 0.03 mg/kg midazolam IV. After preoxygenation with 100% oxygen general anaesthesia was induced with 2 mg/kg propofol. For neuromuscular blockade Group C received 0.1 mg/kg cis atracurium as loading dose while Group A received 0.5 mg/kg of atracurium. Neuromuscular blocker was given intravenously diluted in isotonic normal saline over 10 seconds followed by a fluid rush. Patients were intubated with an appropriate size polyvinyl chloride Endotracheal Tube (ETT). The ETT placement was confirmed using capnography. Anaesthesia was maintained with 50% N2O in O2 and isoflurane 0.6-1%. On completion of surgery, patient was reversed with injection neostigmine 0.05 mg/kg and 0.4 mg glycopyrrolate.
Neuromuscular Monitoring
For neuromuscular monitoring a TOF-SX monitor was used. Two electrodes were attached on internal aspect of the wrist on the surface of the skin along the course of the ulnar nerve to monitor the response of Adductor Pollicis (AP) muscle. Acceleration transducer was attached with tape on the internal aspect of the thumb. Hand and wrist were padded with cotton and bandage to avoid hypothermia. After loss of eyelash reflex, baseline supramaximal stimulus of 0.2 ms square wave at 50 milliamperes was given and TOF response was noted on neuromuscular monitor, after administering loading dose of neuromuscular blocker to the patient in either group. The ulnar nerve was stimulated at the wrist with a stimulus of 0.2 ms duration in TOF mode at 2 Hz every 12 seconds. Intubation was done when TOF count of zero was achieved. TOF counts were regularly monitored and maintenance doses of 1/10th of the total loading dose were repeated when TOF count of one was achieved. Reversal of the neuromuscular blockade was initiated when the TOF Ratio (TOFR) was 75% after the last maintenance dose of the neuromuscular blocker. Trachea was extubated when the TOFR of 0.9 was achieved. The demographic profile including age, sex, height, weight, BMI, ASA grade status of the patients were recorded. The haemodynamics recorded were Mean Arterial Pressure (MAP) and HR.
Onset time was defined as the time from completion of the injection of the neuromuscular blocker till the TOF count was zero. Similarly, duration of action was taken as time from completion of injection of the loading dose till the TOF count one was achieved. To compare the recovery profile of the two study drugs recovery index was used which was the mean with standard deviation time interval in minutes from TOF 25-75% after the last maintenance dose. Signs of histamine release like hypotension, tachycardia, skin rash or erythema and bronchospasm were also observed.
Statistical Analysis
Sample size was calculated keeping in view at most 5% risk, with minimum 85% power and 5% significance level (significant at 95% confidence interval). Raw data was recorded in a Microsoft excel spread sheet and analysed using Statistical Package for the Social Sciences (SPSS version 22.0). Continuous data were presented as mean with standard deviation (mean±SD). Number of patients and/or percentage of cases expressed discrete categorical data. Categorical variables and normally distributed continuous variables were analysed using Pearson’s chi-square test and the independent sample t-test, respectively.
Results
The results were recorded as follows:
The demographic profiles of both the study groups including age, sex, BMI, ASA status and Mallampati Grades (MPG) were found to be comparable (p-value=0.053; non-significant) [Table/Fig-1].
| Variables | Group A | Group C | p-value |
|---|
| Age (years) | 35.60±8.93 | 39.33±11.90 | 0.175 |
| Sex (M/F) | 15/15 | 14/16 | |
| BMI (kg/m2) | 24.82±4.51 | 25.52±3.91 | 0.526 |
| ASA class (I/II) | 18/12 | 17/13 | |
| MPG grade (I/II) | 15/15 | 14/16 | |
M- Male, F- Female, ASA- American Society of Anaesthesiologists, BMI- Body Mass Index, MPG-Mallampati Grades
(p-value non significant)
The time of onset of neuromuscular block with atracurium (Group A) was found to be 168.60±13.44 seconds and with cisatracurium (Group C) was 181.03±21.76 seconds. The result was statistically significant with a p-value of 0.01 [Table/Fig-2].
Onset, duration of action and recovery index.
| Group | Onset time | Duration of action | Recovery index |
|---|
| Group (A) Atracurium | 168.60±13.44 seconds | 37.12±7.62 minutes | 14.63±1.84 minutes |
| Group (C) cisatracurium | 181.03±21.76 seconds | 40.37±7.04 minutes | 15.30±1.96 minutes |
| p-value | 0.01* (significant) | 0.092 (non significant) | 0.181 (non significant) |
*p-value <0.05 is considered statistically significant
The duration of neuromuscular block was 37.12±7.62 minutes in Group A while in Group C it was found to be 40.37±7.04 minutes which was comparable and non-significant (p-value=0.092) [Table/Fig-2].
The recovery indices in both the groups were also comparable to each other. Group A, patients showed a recovery index of 14.63±1.84 minutes after administering the last maintenance dose of atracurium while Group C patients had a recovery index of 15.30±1.96 minutes. These were found to be not significant (p-value=0.181) [Table/Fig-2].
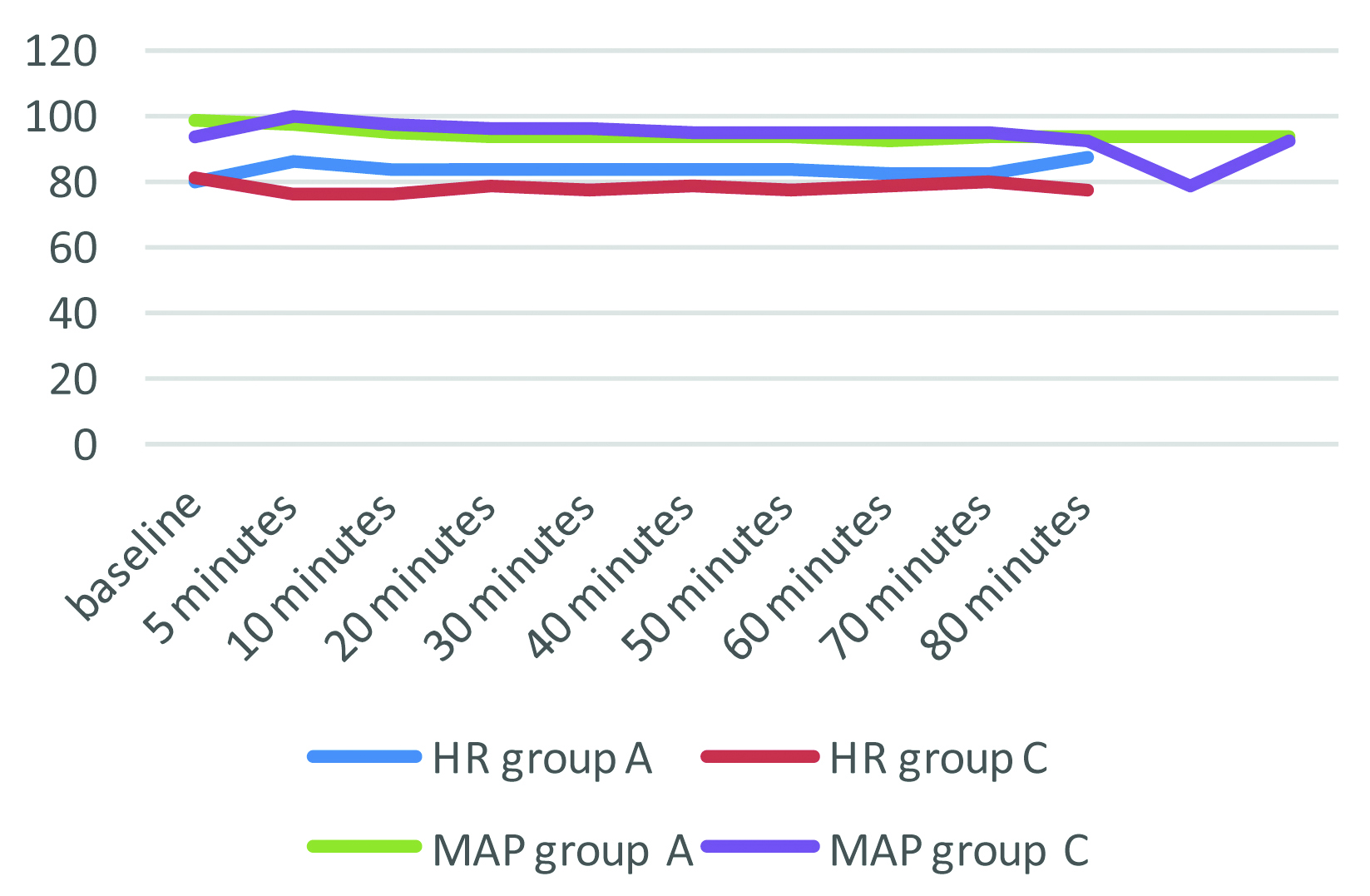
The haemodynamic profile (HR, MAP) of both the study groups was observed and recorded. It was found to be comparable with no significant differences. These recordings were measured at baseline, five minutes, 10 minutes and then every 10 minutes till the end of surgery. The p-values were non statistically significant (p>0.05) [Table/Fig-3].
Haemodynamics profile.
MAP- Mean Arterial Pressure, HR- Heart Rate
The signs of histamine release including hypotension, tachycardia, bronchospasm, erythema or skin rashes were observed clinically. No patient in both the groups had any of these signs.
Discussion
Neuromuscular blocking drugs are extensively used by anaesthesiologists in the operating room and in the intensive care units. Among the array of muscle relaxants available, the most important concern of an anaesthesiologist after their administration, is the complete recovery of the muscle function post-surgery. Atracurium and cisatracurium have a significant advantage over other non depolarising muscle relaxants due to their non-organ dependent metabolism. This implies that postoperative recovery of muscle power is more predictable and ensures patient safety especially in the elderly as well as in patients with compromised organ functions. However, the major undesirable effect of this group of drugs is histamine release leading to anaphylactic or anaphylactoid reactions [10]. In addition, postoperative residual curarisation is also a possibility with all muscle relaxants in cases of excessive dosage or incorrect timing of the repeat dose. It has been seen that there is variable response to neuromuscular blockers in different patients that might lead to a varying degree of residual block present at the end of anaesthesia [11,12].
Traditionally, patients are reversed on the basis of clinical parameters only which generally include adequate tidal volume, sustained hand grip, head lift, bending of legs and protrusion of tongue. However, studies have shown that respiratory function may not be a reliable indicator of muscle strength. Kopman AF et al., have reported that volunteers with TOF ratio <0.5 are able to maintain a five second head lift and have a strong handgrip. According to their opinion, the ability to oppose the incisors and maintain a tongue blade between them is a better clinical indicator of return of adequate muscle strength. As most of the volunteers in their study could not perform this task till the TOF ratio, the maximum they returned to was 0.85. They also stated that clinical as well as instrumental parameters both can be used to assess the residual paralysis in Post Anaesthesia Care Unit (PACU). However, the clinical tests require awake and cooperative patient. The residual effects of other anaesthetic drugs may interfere with the evaluation of neuromuscular function clinically. This gives an edge to the neuromuscular monitoring over clinical assesment [13]. Debaene B et al., recommend mandatory use of quantitative TOF assessment at the end of surgery to evaluate the residual neuromuscular block [14].
All the above instances prompt the anaesthesiologist to use drugs which have predictable recovery and undergo complete elimination after reversal of anaesthesia, removing the possibilities of residual effects, if any.
In the present study, both the study groups were comparable in terms of demographic profile which included age, weight, gender, BMI and the ASA status of the patients [Table/Fig-1]. This rules out the possibility of differences in the dosages based on weight, age group and BMI.
On recording the onset time of neuromuscular block, which was the time from the end of injection of the muscle relaxant till the TOF count of zero was achieved, we found a significant difference between the two study groups (p-value=0.01). The TOF count of zero was taken to ensure that all the acetyl choline receptors were blocked. The onset time recorded in Group A was 168.60±13.44 seconds and in Group C was 181.03±21.76 seconds showing lesser onset time taken in the patients who received atracurium as the muscle relaxant [Table/Fig-2]. This difference has been quoted to be due to the higher potency of cisatracurium as compared to atracurium which produces slower onset at the laryngeal muscles [15]. In a study conducted by El-kasaby AM et al., the efficacy of atracurium was compared with different doses of cisatracurium for general anaesthesia. The authors found that the time of onset with 0.5 mg/kg atracurium (3.24±0.55 minutes) was significantly lower than that with 0.1 mg/kg of cisatracurium (4.37±0.46 minutes), resonating similar results as in present study [16]. They concluded that at equipotent doses atracurium is more effective neuromuscular blocking agent than cis atracurium while at higher doses cis atracurium provides a more effective and faster onset as compared to atracurium. Similar findings were also reported by Mellinghoff H et al., in their study that compared the onset and recovery of cis atracurium and atracurium after a bolus dose and subsequent infusion in equipotent doses. In their study, the onset time of atracurium was found to be 2.3±1.1 minute and 3.1±1.0 minute for cisatracurium, showing shorter onset for atracurium [17]. This too is in concordance with present study. Bluestein LS et al., also reported a longer time of onset for cisatracurium (4.6±0.3 minutes as compared to atracurium 4.0±0.3 minutes) in equipotent doses [9]. In the present results are also supported by studies done by Carroll MT et al., Adamus M et al., and Xiabio F et al., Donati FC et al., proposed a model to explain the reverse onset and potency relationship [18-21]. The neuromuscular blocker with low potency has more number of molecules which diffuse to the central compartment causing a rapid onset. Potent non depolarising muscle relaxants reach slowly and bind strongly and also repeatedly to the acetyl choline receptors causing slower onset and longer duration of action [21]. The slower onset of cis atracurium is also due to delayed and lower peak concentration of cis atracurium at the effector site because of slower biophase equilibrium [20]. For a shorter onset of action higher doses of cis atracurium are needed at the cost of a significantly longer duration of action of the neuromuscular blocakade [16].
We recorded the mean duration of the neuromuscular block in Group A was 37.12±7.62 minutes while in Group C was 40.37±7.04 minutes. Similar results were observed in the study conducted by El-kasaby AM et al., who concluded that cis atracurium and atracurium have comparable duration of action at equipotent doses (2xED95 i.e., 0.5 mg/kg atracurium and 0.1 mg/kg cis atracurium); 44.4±4.13 and 43.6±4.15 minutes respectively [16]. In another study conducted by Bluestein LS et al, the duration of action of atracurium (45.6±2.6 minutes) and cis atracurium (45.2±2.0 minutes) in 2xED 95 doses was found to be statistically non significant [9]. Carroll MT et al., have also noted the median duration of effect of atracurium to be 43 minutes and of cis atracurium to be 41 minutes, with no statistical significant difference [18].
The recovery index was recorded as the time interval between the last maintenance doses till the TOF ratio of 0.7 was achieved. The recovery index in the cisatracurium group was found to be 14.63±1.84 minutes and in atracurium group to be 15.30±1.96 minutes (statistically non-significant; p-value=0.181) showing that at equipotent doses, cisatracurium and atracurium have comparable recovery profiles. Mellinghoff H et al., also quoted similar findings in their study showing the spontaneous recovery intervals 25-75% of 18±11 minutes and 18±8 minutes for cisatracurium and atracurium respectively [17]. Bluestein LS et al., in their study while comparing equipotent doses of cisatracurium with atracurium also found a comparable recovery indices of both these drugs (13.4±0.9 and 12.8±0.7 minutes respectively) [9]. Despite cisatracurium being four times more potent than atracurium these findings can be attributed to the fact that hoffmann elimination may have a greater role in the elimination of cisatracurium as compared to atracurium [22]. Xiabio F et al., compared onset and recovery profiles of cisatracurium with rocuronium in elderly patients under total; intravenous anaesthesia. They concluded that cisatracurium shows comparable recovery profiles in adults (18-64 years) as well as elderly (≥65 years) patients. The recovery index was 15.30±2.55 minutes in adult group and 15.50±2.28 minutes in elderly group. This makes cisatracurium an agent of choice for procedures and patient conditions requiring predictable and rapid recovery [20]. The more predictable recovery index also ensures patient safety and decreases the incidence of postoperative respiratory complications.
On comparing the haemodynamic profile which included the HR and MAP, the results were found to be statistically non-significant (p-value>0.05). The occurrence of tachycardia and hypotension were specifically noted to monitor the effects of histamine release. No episodes of hypotension or tachycardia were noted in any of the groups. This could be ascribed to the slow intravenous injection of the study drug in each group. However, various studies have reported that hypotension may occur with atracurium administration which could be due to histamine release [7,23-25]. However, studies that monitored histamine levels after atracurium administration contradict this and report minimal haemodynamic changes due to atracurium injection [26]. In addition, the decrease in systemic vascular resistance due to induction agents may be a confounding factor in the haemodynamic changes. The lowering of MAP due to induction agents may be erroneously attributed to atracurium [25,26].
On observing the signs of histamine release, we observed that none of the patients in any group had episodes of flushing, erythema, hypotension, bronchospasm, tachycardia or urticaria. This histamine release may be prevented or minimised by injecting the neuromuscular blocker slowly over 30-60 seconds [27]. Hosking MP et al., have stated that by using H1 and H2 receptor blockers before administering large dose atracurium (six times ED95), the haemodynamic manifestations of histamine release can be effectively prevented. They used diphenhydramine 1 mg/kg and cimetidine 4 mg/kg 30 minutes before giving 1.5 mg/kg atracurium intravenously and found that atracurium induced reduction in MAP was decreased by 30 mmHg [28]. Hughes R and Chapple DJ that despite a 10-20 times increase in the plasma histamine levels atracurium is not vagolytic and does not block the innervation by autonomic ganglia [29]. In a study conducted by Kumar A et al., the frequency of urticaria after administration of atracurium was assessed. They concluded that in conventional doses atracurium is not associated with formation of urticarias although significant changes in haemodynamics may occur [30].
Limitation
We were unable to measure the plasma histamine levels due to non-availability of this facility in Government Medical College, Amritsar, Punjab, India.
Conclusion
Atracurium is superior to cisatracurium in equipotent dose in terms of its faster onset. However, the duration of action and recovery profiles of both drugs are similar showing that atracium and cisatracurium in an equipotent dose of 2xED95 provides similar recovery profile. Hence, cisatracurium can replace atracurium in the routine clinical practice.
M- Male, F- Female, ASA- American Society of Anaesthesiologists, BMI- Body Mass Index, MPG-Mallampati Grades
(p-value non significant)
*p-value <0.05 is considered statistically significant