Adequate, accurate and timely communication among healthcare providers is crucial for continuity of care. Written communication has several advantages like easy and fast retrieval, portability etc., as compared to face-to-face communication and it is also important from legal point of view. Discharge summaries and discharge letters are widely used for communication among different healthcare facilities [1,2]. It is essential to have clear and concise discharge summary with all pertinent details required for further management of the patient. In fact, deficient discharge summaries may lead to re-hospitalisation, adverse events, unsatisfied patients and clinicians, and suboptimal use of resources [1,3].
Even though an important document, significant deficiencies in discharge summaries were reported almost 20 years back [4,5]. The trend appears to be continued to date [1,2]. Four broad domains viz., ‘discharge diagnosis’, ‘treatment received’, ‘result of investigations’ and the ‘follow up required’ have been identified as essential components of discharge summaries [6]. Further ‘relevance’, ‘accuracy’, ‘clarity’ and ‘presentation’ have been proposed as key quality indicators for each component of the discharge summaries [7]. Suggested strategies to improve written communication include structured approach, early introduction in medical curriculum, feedback and continuous evaluation and changing processes [1].
In a teaching hospital, discharge summaries are generally prepared by less experienced junior doctors without any specialised education in immaculate documentation [8]. Considering them as future leaders and role models, it is imperative to empower them with importance and methods of proper documentation. Our experience and the worldwide evidence suggest that educational intervention with feedback can improve the core competencies in documentation [7-12].
We assessed the effect of educational intervention in improving quality of discharge summaries.
Materials and Methods
The present educational interventional study was carried out during August to September, 2013 in Department of General Medicine of Shree Krishna Hospital, Karamsad, Anand, Gujarat, India. The discharge summaries are usually prepared by residents. All the 18 residents working in the department during the study period were included in the study. The study was approved by the Institutional Ethics Committee.
All discharge summaries of patients getting discharged 48 hours after admission under Department of Medicine before (August 2013) and after (October 2013) educational intervention were evaluated in the study. The discharge summaries were audited by two consultants from Medicine department after blinding patient particulars. It was not feasible to evaluate each discharge summaries by both of them. Both of them attended the educational intervention session conducted for the residents as described below.
The consultants were thoroughly oriented about the process and audited 10 discharge summaries prepared in September 2013 independently (not included in the analysis). The minor discrepancies were discussed with the senior consultant to arrive at a consensus. This exercise was conducted to reduce the inter-rater variability between two consultants, each of whom audited nearly half of the 426 discharge summaries.
Study Population and Intervention
During the intervention (September 2013), all the residents were invited for a structured discharge summary curriculum conducted by a senior consultant having experience in medical education. The educational intervention session of 120 minutes included following activities:
Initial brief interactive power point presentation on ‘One Sentence Summary’: ‘One sentence summary’ defining a specific case in abstract terms is one of the early steps in creation of mental abstraction or ‘problem representation’ in clinical medicine [13]. This was followed by hands on experience of writing one sentence summary from a written patient story in four small groups of 4-5 residents in each group.
Brief interactive power point presentation on ‘Qualities of a Good Discharge Summary’: Following this presentation, residents in four small groups analysed two different discharge summaries for strengths and weaknesses. ‘Qualities of a good discharge summary’ included details about components of a discharge summary based on evaluation instrument from READ workshop as described below [14].
Following the educational intervention, the senior consultant randomly checked few discharge summaries prepared by medicine residents and provided feedback during departmental meetings in September 2013.
Study Tool
There is no structured format to evaluate discharge summaries specific to India. A good evaluation strategy is proposed by Talwalkar JS et al., which is amalgamation of pertinent guidelines available from different authentic sources and has a good inter-rater reliability [11]. Talwalkar JS et al., developed ‘READ’ workshop for internal medicine residents to improve documentation skills. The IFF for discharge summary used in this workshop is a more comprehensive and objective version that we found suitable for such evaluation.
The form evaluated information on seven pertinent domains and an overall impression of the discharge summary. The ‘Basic Information’ had seven dichotomous items (coded as Yes=1 and No=2). The ‘History’ (four items), ‘Physical Examination’ (one item), ‘Lab Data’ (two items), ‘Hospital Course’ (seven items) and ‘Discharge Plan’ (two items) were evaluated on Likert scale (strongly agree=one, agree, neutral, disagree and strongly disagree=five) for positively worded statements about discharge summary. The ‘Discharge Plan’ contained three dichotomous items (coded as Yes=1 and No=2). This scheme of coding implied that lower scores (individual or mean) indicate better quality. Finally, the overall impression (five items) of the discharge summary was assessed using the same Likert scale but with two negatively worded statements viz. ‘More detail is needed in this note’ and ‘too much detail is provided in this note’.
We used the same format but with following modifications:
The two dichotomous items of the ‘Discharge Plan’ viz., ‘mention of how information was/will be communicated to Personal Medical Doctor (PMD)’ and ‘complimentary copy to treating physicians’ were deleted as these questions were not very relevant to Indian academic settings.
Statistical Analysis
Descriptive statistics {mean±SD, frequency (%)} were used to depict pertinent characteristics of the data. Independent sample t-test was used to gauge the effect of educational intervention in different domains assessed on five point Likert scale as well as for total score. Chi-square test was applied to assess the effect on categorical variables used in ‘basic elements’. For ease of understanding, the Likert scale items were classified as ‘acceptable’ (strongly agree and agree) and ‘unacceptable’ (neutral, disagree and strongly disagree). For two negatively worded statements of ‘Overall Impression’ the classification was reversed. (Strongly disagree and disagree as ‘acceptable’ and neutral, agree and strongly agree as ‘unacceptable’). Chi-square test was used to portray the effect of intervention for this classification. The analysis was performed using STATA (14.2).
Results
All the 18 residents participated in the study. A total of 614 discharge summaries were prepared in the month of August 2013 (pre intervention) and October 2013 (post intervention). One hundred seventy discharge summaries (92 and 78 from pre and post intervention periods respectively) were excluded as they were generated for patients admitted for less than 48 hours. We could not trace 18 discharge summaries (10 and 8 from pre and post intervention periods respectively) from medical records at the time of audit. Thus, 426 discharge summaries (223 and 203 from pre and post intervention periods respectively) were audited. Furthermore, hard copy of one discharge summary from post intervention period was spoiled and we could examine basic elements only from this summary. A total of 29 individual components of discharge summary under headings of basic elements, history, physical examination, hospital course, laboratory and diagnostic data, discharge plan and overall assessment were audited.
The mean±SD scores decreased significantly in all the domains of discharge summary viz., history, physical examination, diagnostic data, hospital course and discharge plan as well as composite score (Total Score) of all these domains [Table/Fig-1,2].
Comparison of pre and post intervention quality of discharge summaries.
| Particulars | Pre intervention n=223 (mean±SD) Frequency (%) of “Acceptable” | Post intervention n=202 (mean±SD) Frequency (%) of “Acceptable” | p-value |
|---|
| History: The note contains |
| A succinct summary of the key events leading to hospitalisation. | 2.39±0.81179 (80.3) | 2.06±0.37195 (96.5) | <0.001<0.001 |
| The past medical history. | 2.14±0.55207 (92.8) | 2.06±0.37195 (96.5) | 0.10.09 |
| Pertinent elements of the social history. | 5.00±0.000 (0.00) | 4.79±0.7614 (6.9) | <0.001<0.001 |
| Pertinent elements of the family history. | 4.96±0.312 (0.90) | 4.75±0.8417 (8.40) | <0.001<0.001 |
| Total (History) (mean±SD) | 14.49±1.17 | 13.67±1.45 | <0.001 |
| Physical Exam: Documented in the physical exam are |
| Findings (positive or negative) pertinent to history elements. | 2.52±0.91166 (74.4) | 2.14±0.53188 (93.1) | <0.001<0.001 |
| Diagnostic Data: The note contains |
| Pertinent (normal and abnormal) laboratory data. | 2.01±0.13222 (99.6) | 2.06±0.35194 (96.0) | 0.030.02* |
| Pertinent results of diagnostic studies (e.g., CXR, EKG). | 2.89±0.90102 (45.7) | 2.31±0.52146 (72.3) | <0.001<0.001 |
| Total (Diagnostic Data) (mean±SD) | 4.90±0.90 | 4.37±0.61 | <0.001 |
| Hospital Course: The note contains a |
| Summary statement pertaining to the principal diagnosis. | 2.68±0.98150 (67.3) | 2.10±0.46192 (95.0) | <0.001<0.001 |
| Problem list that parallels the diagnoses listed above. | 2.40±0.81179 (80.3) | 2.08±0.42194 (96.0) | <0.001<0.001 |
| Separate paragraph dedicated to each problem listed. | 4.11±0.361 (0.4) | 4.02±0.170 (0) | <0.001NA |
| Brief discussion of the evaluation of each problem. | 3.49±0.8957 (25.6) | 2.13±0.50188 (93.1) | <0.001<0.001 |
| Brief discussion of the treatment of each problem. | 3.34±0.9574 (33.2) | 2.14±0.51187 (92.6) | <0.001<0.001 |
| Brief discussion of the outcome of each problem. | 4.01±0.8425 (11.2) | 2.14±0.51187 (92.6) | <0.001<0.001 |
| Specific follow-up plan for each relevant problem. | 5.00±0.000 (0) | 4.82±0.638 (4) | <0.0010.002* |
| Total (Hospital Course) (mean±SD) | 25.03±2.81 | 19.45±1.73 | <0.001 |
| Discharge Plan: A plan is outlined regarding |
| Future physician’s visits scheduled (or to be scheduled). | 2.29±0.74192 (86.1) | 2.22±0.63180 (89.1) | 0.290.35 |
| Specific studies that require follow-up. | 2.57±0.81140 (62.8) | 2.23±0.55169 (83.7) | <0.001<0.001 |
| ^A list of discharge medications (names, doses, and frequency). | NA223 (100) | NA202 (100) | ----NA |
| Total (Discharge plan) (mean±SD) | 4.86±1.14 | 4.45±0.82 | <0.001 |
|
| Composite Score of all domains: Mean (SD) | 51.81±3.89 | 44.08±2.64 | <0.001 |
*Fisher’s exact test was used.
^Classified as Yes=1/No=0, Frequency of Yes is provided. Not included in composite score.
NA: Not Applicable
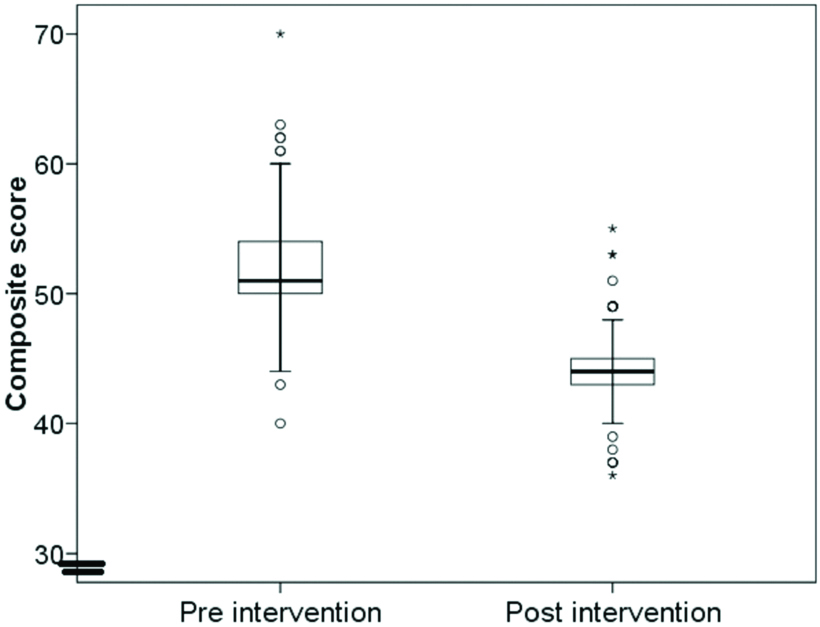
Box plot depicting comparison of composite scores.
O: Outlier, *: Far Outlier
The decrease in the mean score was associated with improvement in documentation as explained in the methods section. This improvement was evident even after categorising the Likert scale as ‘acceptable’ and ‘unacceptable’. Despite these improvements, serious lapses in social and family history were observed [Table/Fig-1].
The documentation of ‘Basic elements’ improved significantly except for ‘date of admission’. It was not possible to judge the improvement in the domain ‘procedures performed during hospitalisation’ due to the number of records to which this parameter is applicable [Table/Fig-3].
Pre and post intervention quality of basic elements of discharge summary.
| Particulars | Pre intervention n=223 Frequency (%) | Post intervention n=203 Frequency (%) | p-value |
|---|
| Basic Elements: The following basic elements were present: |
| Date of admission | 220 (98.7) | 203 (100) | 0.25* |
| Date of discharge | 194 (87.0) | 200 (98.5) | <0.001 |
| Disposition location (eg, home, ECF, short-term rehab) | 175 (78.5) | 185 (91.1) | <0.001 |
| Principal diagnosis for hospitalisation | 209 (93.7) | 200 (98.5) | 0.01* |
| Secondary diagnoses addressed during hospitalisation | 76 of 111 (68.5) | 69 of 79 (87.3) | 0.003 |
| Procedures performed during hospitalisation | 3 of 7 | 0 of 1 | NA |
| Consultants | 213 (95.5) | 203 (100) | 0.002 |
*Fisher’s Exact Test was used.
The mean±SD scores decreased significantly for all the three positively worded individual items of ‘Overall Impression’ of the discharge summary. The mean±SD scores improved significantly for negatively worded item ‘more detail is needed in this note’ but fared similarly for the item ‘too much detail is provided in this note’. Similar trend was noted even after categorising the variables [Table/Fig-4].
Pre and post intervention quality of overall impression of discharge summary.
| Particulars | Pre intervention n=223 mean±(SD) Frequency (%) of “Acceptable” | Post intervention n=202 mean±(SD) Frequency (%) of “Acceptable” | p-value |
|---|
| This is an effective note. | 3.0±0.99105 (47.1) | 2.13±0.49189 (93.6) | <0.001<0.001 |
| More detail is needed in this note.* | 1.99±0.426 (2.7) | 2.24±0.6524 (11.9) | <0.001<0.001 |
| Too much detail is provided in this note.* | 3.98±0.16220 (98.7) | 4.0±0.07202 (100) | 0.060.25 |
| The length of this note is appropriate for the complexity of the visit. | 2.51±0.87165 (74.0) | 2.21±0.61180 (89.1) | <0.001<0.001 |
| If I didn’t know this patient, this note would help me care for him/her. | 2.63±0.66102 (45.7) | 2.19±0.52173 (85.6) | <0.001<0.001 |
*: a negatively worded statement. Higher score on this item indicate better quality
Discussion
The quality of discharge summaries was suboptimal before the educational intervention. It improved significantly after the intervention but serious lapses in social and family history were observed even after the intervention.
The evolution of Indian health system was greatly influenced by Bhore committee report of 1946. With an emphasis on health for all, preventive care approach, rural healthcare delivery and training of social physicians, India was able to develop indigenous healthcare models without copying western curative models [15]. The medical education in India was developed in line with the needs of health delivery system. For example, community medicine departments were created to provide social context to medical education [16]. Unfortunately; like the health delivery system, the education system also lacked pertinent and timely reforms and became stagnant and outdated for the contemporary needs. A recently published article in ‘Lancet’ provides a balanced critique of downfall of Indian health system as well as the education system [17].
The medical education in India traditionally focussed on theoretical knowledge and clinical skills in the past. Albeit the soft skills like communication skills (breaking bad news, counselling etc.), documentation, ethics etc., were identified as important constituents of medical education time and again, they failed to get adequate attention in the curricula [17-20].
Emergence of medical education technology and hue and cry suggesting urgent need towards reforms in medical education in the last decade had some positive impact. Medical Council of India (MCI) proposed reforms in both undergraduate and postgraduate medical education through different expert committees but the recommendations are still pending approval in the parliament [17, 19-21].
Various methods have been tried successfully to improve the quality of discharge summaries but with varied assessment tools [7,8,11,12]. It is thus difficult to compare different interventions for their impact on quality of discharge summaries. However, the bottom line is that various interventions were successful in improving the quality of the discharge summaries. These studies once again endorse DA Cook’s statement–“If you teach them, they will learn” [22]. The training module used in the current study included construction of ‘one sentence summary’ from given patient story followed by critique of written discharge summaries in small group. It was felt important to articulate this concept and explain how one can transform patient specific data into abstract terms and prepare one sentence summary. We believe that this exercise would have helped residents to conceptualise the discharge summary mentally before they document it precisely. This educational intervention revealed that the required documentation skills can be imparted by simple but structured workshop followed by supportive supervision for a short period.
The box plot revealed that not only the performance improved but also became consistent [Table/Fig-2]. While significant improvement in the documentation skills after the educational intervention was noted, some key issues in conceptualisation of medical care were noted.
Though, mean±SD scores provide a useful information on measuring change, it does not provide enough information on attainment of acceptable level. The classification of the Likert scale variables revealed serious lapses in social and family history even after the intervention. Social and family history are important for deciding current treatment regimen as well as for continuity of treatment. Carelessness in documenting detailed history indicates the attitude of treating the disease rather than treating the patient holistically. For example, one of the authors visited an extension centre of the hospital where junior doctors handle the day to day operations. A girl of about three-year-old presented with a minor wound accompanied by her mother. Without even checking for her height, weight, etc.. the treating physician just completed the dressing and asked her to revisit only if needed. The girl clearly appeared undernourished with pale hair and face. The treatment for the same is free. Further the vaccination drive by the state Government was due in the next week. The physician missed the opportunity to treat/advice about undernourishment and ensure that the girl gets the free vaccines. This also indicates the inability of community medicine departments to provide social context to medical care at undergraduate level and should be addressed with priority. This appears to be a universal phenomenon [8,11].
Replication of this module in other departments is due before a generalised framework for such curriculum can be developed. Further, a comprehensive and standardised assessment tool with an inbuilt option viz., ‘Not Applicable (NA)’ could be developed to test efficacy of different educational interventions across disciplines. Some preliminary efforts in this direction by developing a score card to audit hospital discharge summary and including the option ‘NA’ were made but both the studies were conducted in Internal Medicine Department [23,24].
An informal discussion with the residents by one of the authors (statistician) revealed that the residents understood the importance of immaculate documentation and the organisation of a good discharge summary. Most of them expressed their willingness to master the art of writing good and useful discharge summaries but also expressed their concerns mainly ‘lack of time’ to perform this task. Some of them suggested exploring automation through computerisation to transfer the available patient data to discharge summary that will minimise their work.
Automation using technology as well as standardised proforma were successfully tried to improve discharge summaries in emergency medicine departments [25,26]. The ‘systems’ department of the hospital came up with an internal system viz., ‘SOLACE’ (Shree Krishna Hospital On Line Application for Clinical Excellence) that allows the residents/consultants to perform real time data entry through tablets. The further refinement of the system to automate discharge summary process is being developed to facilitate completeness and accuracy of documentation despite busy schedules. However, it should be noted that mere automation does not improve the communications unless supplemented by right processes [27].
Limitation
Although, the residents were not informed about the assessment to minimise the ‘Hawthorne’ effect (An improvement in human behaviour or performance in response to their awareness of being observed), the retention of acquired skills was not tested. Further, this is a single centre study and the findings may not be generalised.
Conclusion
The quality of discharge summaries were suboptimal before the educational intervention. It is possible to instill soft skills like communication, documentation etc., through innovative curriculum. Conducting such studies across India will help determine the current scenario and formulate necessary interventions to improve it.
*Fisher’s exact test was used.
^Classified as Yes=1/No=0, Frequency of Yes is provided. Not included in composite score.
NA: Not Applicable
*Fisher’s Exact Test was used.
*: a negatively worded statement. Higher score on this item indicate better quality