Measurement of Sacral Parameters of Surgical Importance in North Indian Population
Shabnam Arora1, Minakshi Verma2, Sohinder Kaur3, Sudha Chhabra4, Priyanka Jain5
1 Senior Resident, Department of Anatomy, Lady Hardinge Medical College, Delhi, India.
2 Associate Professor, Department of Anatomy, Lady Hardinge Medical College, Delhi, India.
3 Director Professor and Head, Department of Anatomy, Lady Hardinge Medical College, Delhi, India.
4 Ex Head and Senior Professor, Department of Anatomy, Pt. BD Sharma PGIMS Rohtak, Rohtak, Haryana, India.
5 Statistician, Institute of Liver and Biliary Sciences, Vasant Kunj, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shabnam Arora, House No.1114, Sector 4, Gurugram-122001, Haryana, India.
E-mail: shabb84@gmail.com
Introduction
Posterior screw placement on sacrum is done in various conditions. Screws are inserted into the body of first/second sacral vertebra. So, Linear parameters form the basis for adequate fixation of bone and to avoid injury to neurovascular structures. Detailed information about sacral parameters will be helpful for surgeons performing dorsal screw placement, Anterior Lumbar Interbody Fusion (ALIF), Posterior Lumbar Interbody Fusion (PLIF) with better prognosis and lesser complications.
Aim
To measure and compare various linear parameters of sacrum in males and females.
Materials and Methods
In the present study, 48 dry sacra (24 males and 24 females) were taken. Linear parameters of upper sacrum like sacral length, sacral breadth, first sacral anteroposterior and transverse diameter, sacral canal anteroposterior and tranverse diameter, posterior pedicle height, pedicle depth, pedicle width, vertical and transverse diameter of auricular surface were manually measured with digital, vernier caliper. The data were analysed, using SPSS version 16.0 and compared using Student’s t-test with p value <0.05 taken as significant.
Results
Statistically significant gender difference was observed in sacral length, values were more in males (10.57±0.95 cm), than in females (8.56±0.49 cm) with p<0.05 and second sacral body height was found to be more in males (2.55±0.23 cm) than in females (2.16±0.20 cm) with p<0.05. Sacral canal anteroposterior diameter values were more in males (2.31±0.33 cm) than in females (2.07±0.36 cm) with p<0.05. Vertical diameter of auricular surface values on right side were more in males (5.43±0.40 cm) than in females (5.07±0.37 cm) with p<0.05.
Conclusion
Precise measurements of dry sacra and gender comparison will be helpful for the surgical intervention in sacral region. The values obtained can be used as a baseline data for making population specific prosthesis and during implant insertion.
Dorsal screw placement, Pedicle width, Posterior pedicle height, Sacral body height, Sacral length
Introduction
Sacrum is the site for screw placement in many clinical conditions like sacral fractures, neoplasm of sacrum, spinal disorders, and sacroiliac joint disruption [1]. In conditions like sacroiliac disruptions and sacral fractures lateral to foramina, screw fixation runs from S1 pedicle to iliac wing [2].
Sacrum is flat triangular bone formed by the fusion of five vertebrae. It is larger in males than in females, whereas width of ala is more in females than in males [3]. Instrumentation on sacrum always carries the risk of injuries to important neurovascular structures lying adjacent to sacrum, due to complex anatomy of first sacral vertebrae [4-6].
Screw placement depends on entry point and direction of screws. Entry point lies inferolateral to facet joint between fifth lumbar and first sacral vertebra, then screw runs through pedicle, either to promontory in anteromedial direction or either to sacral ala in anterolateral direction. Screw placement is also influenced by biomechanical strength, which should met with screw anti extraction force requirement [7]. Vital structures like ureter, elements of lumbosacral plexus, branches of common iliac artery and cauda equina are vulnerable during posterior screw placement [8]. Placement of pedicle screws into first sacral vertebrae is a difficult surgical procedure [9]. Due to variable anatomy of first sacral vertebra, sometimes screws can also be inserted into second vertebral body to strengthen lumbosacral junction [10]. Most accurate information on measurements of sacrum is provided by CT scans. CT scans of upper sacrum showed that the junction of pedicle and vertebral body is an optimal area for bony purchase as this avoids foramina and structures adjacent to it [11]. In present study, linear data was obtained from direct measurements on the sacrum with digital calliper.
Materials and Methods
Prospective morphometric study was done on 48 dry sacra, procured from Department of Anatomy of Lady Hardinge Medical College, Delhi, India from October 2016 to January 2017. On the basis of sacral index, sacra were grouped as male and female.
Sample size selection was done on the basis of sacral breadth with reference to the research paper by Basaloglu H et al., Morphometry of sacrum for clinical use (n=48, α=5%, power=90%) [12].
Bones with fractures, trauma and deformities of any kind were excluded from the study. Total 13 linear parameters were measured as described below. The Student’s t-test was used to make comparison between male and female subjects and also between right and left sides. All the parameters were measured with the help of digital vernier caliper.
Linear Parameters
Sacral length (AB): Point A was taken as the midpoint on sacral promontory to Point B on the midpoint of apex [Table/Fig-1a].
a) Point A-mid-point on sacral promontory, point B-mid-point on apex; b) Point C and D-maximum distances between alar surfaces.
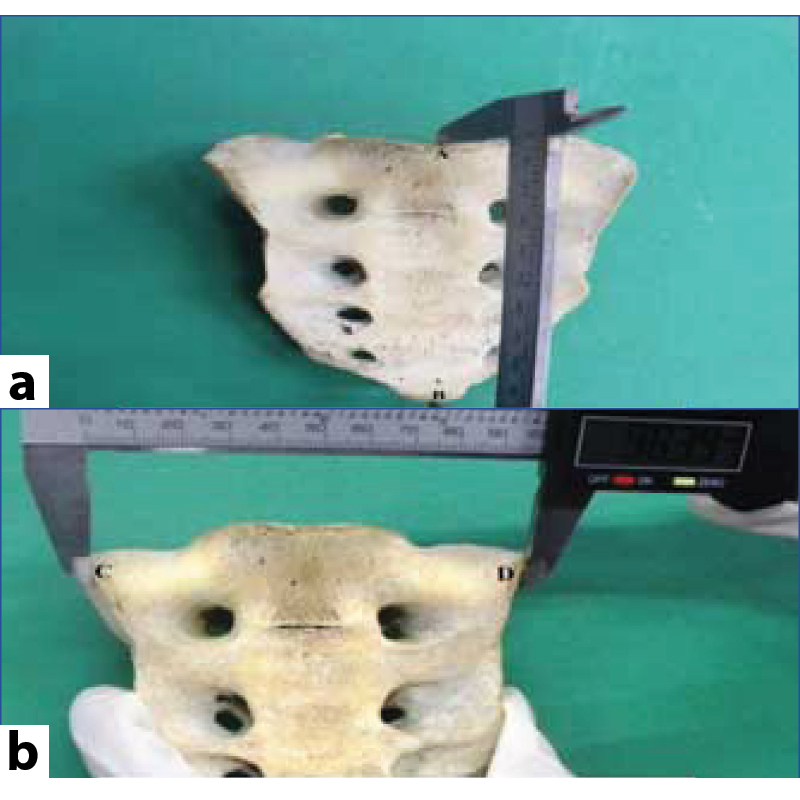
Sacral breadth (CD): Maximum distance between ala on pelvic surface of sacrum [Table/Fig-1b].
First sacral body height (EF): Distance measured from Point E on the midpoint of sacral promontory to the Point F on the midpoint on first transverse ridge on pelvic surface [Table/Fig-1c].
c) Point E-mid-point on sacral promontory, point F-mid-point on first transverse ridge; d) Point G-mid-point on first transverse ridge, point H-mid-point on second transverse ridge.
Second sacral body height (GH): First point G was taken as midpoint on the first transverse ridge and second point H as midpoint on second transverse ridge on pelvic surface [Table/Fig-1d].
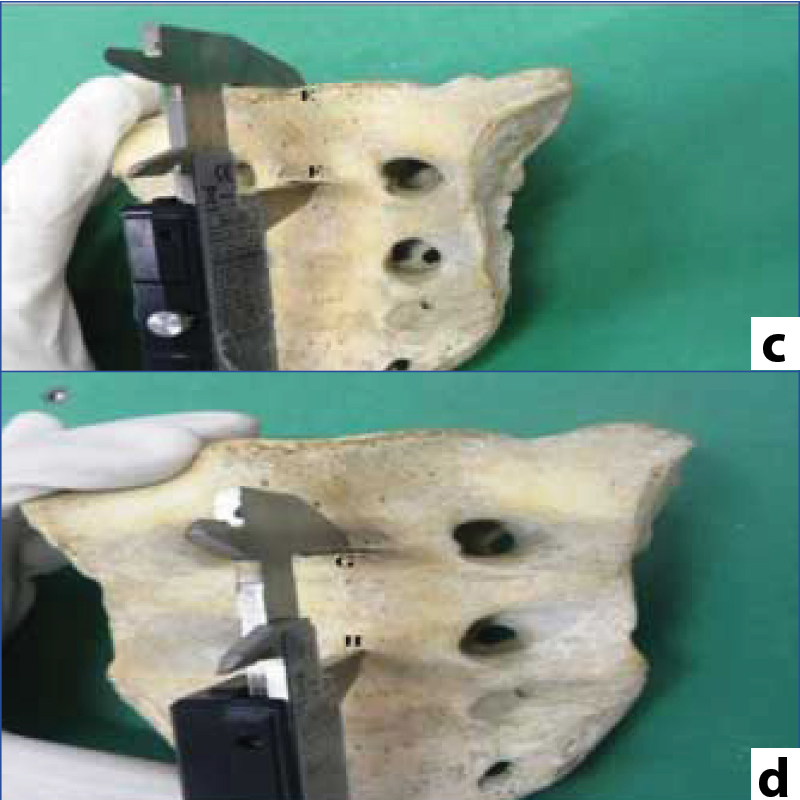
First sacral body anteroposterior diameter (IJ): Point I was taken as midpoint on sacral promontory and Point J taken as midpoint on posterior border of first sacral vertebra [Table/Fig-1e].
e) Point I-mid-point on sacral promontory, point J-mid-point on posterior border of first sacral vertebra; f) K and L-maximum transverse distance of first sacral body on base of sacrum.
First sacral body transverse diameter (KL): Maximum transverse distance of first sacral body on base of sacrum [Table/Fig-1f].
Sacral canal anteroposterior diameter (MN): Distance from Point M taken was midpoint on sacral promontory to Point N was taken on upper border of sacral canal at the level of first spinous process [Table/Fig-1g].
g) Point M-mid-point on sacral promontory, point N-upper border of sacral canal at level of first spinous process; h) Point O and P-maximum transverse diameter of sacral canal at level of first sacral vertebra.
Sacral canal Transverse Diameter (OP): Maximum transverse diameter of sacral canal at the level of first sacral vertebra on the base of sacrum [Table/Fig-1h].
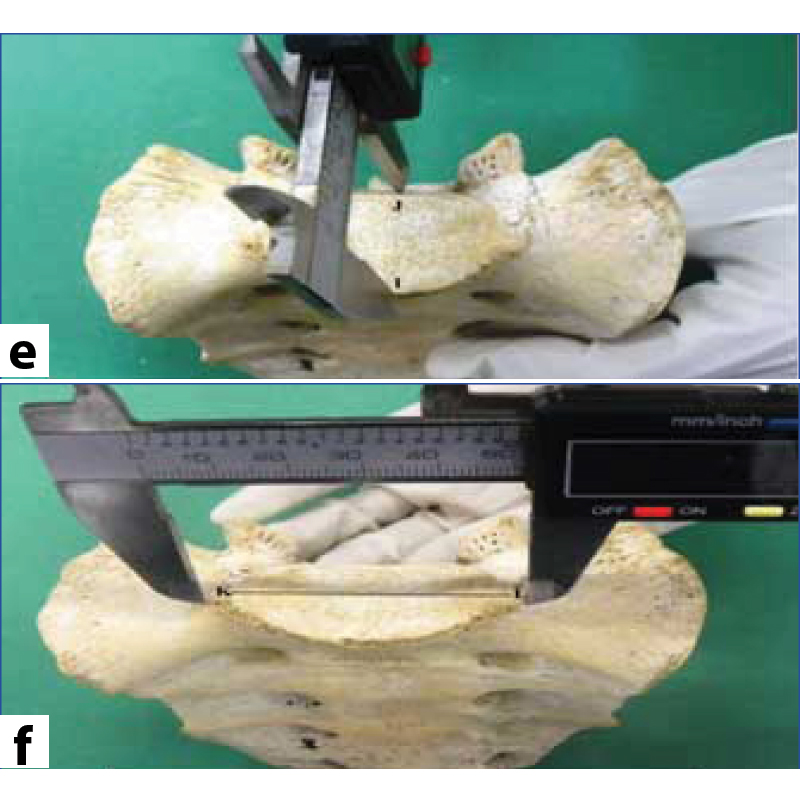
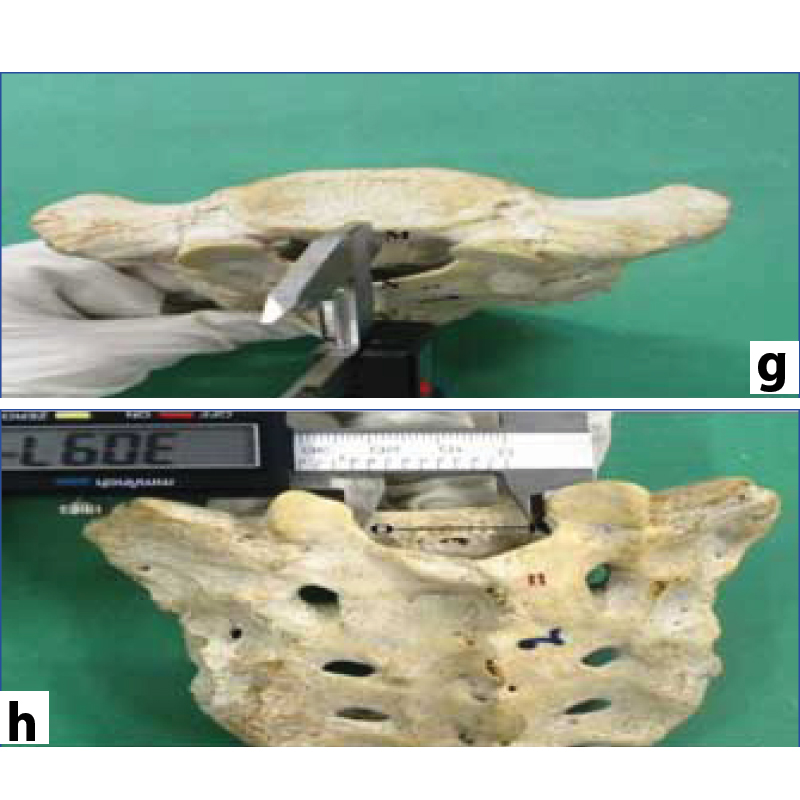
Posterior pedicle height (QR): Distance between the Point Q was taken on pedicle lateral to superior articular process and Point R was taken as midpoint on superior border of first sacral foramen, measured with the help of vernier caliper on both sides [Table/Fig-1i].
i) Point Q-pedicle lateral to superior articular process, point R-mid-point on superior border of first sacral foramen; j) Point S-anterior limit of pedicle, point T-posterior limit of pedicle.
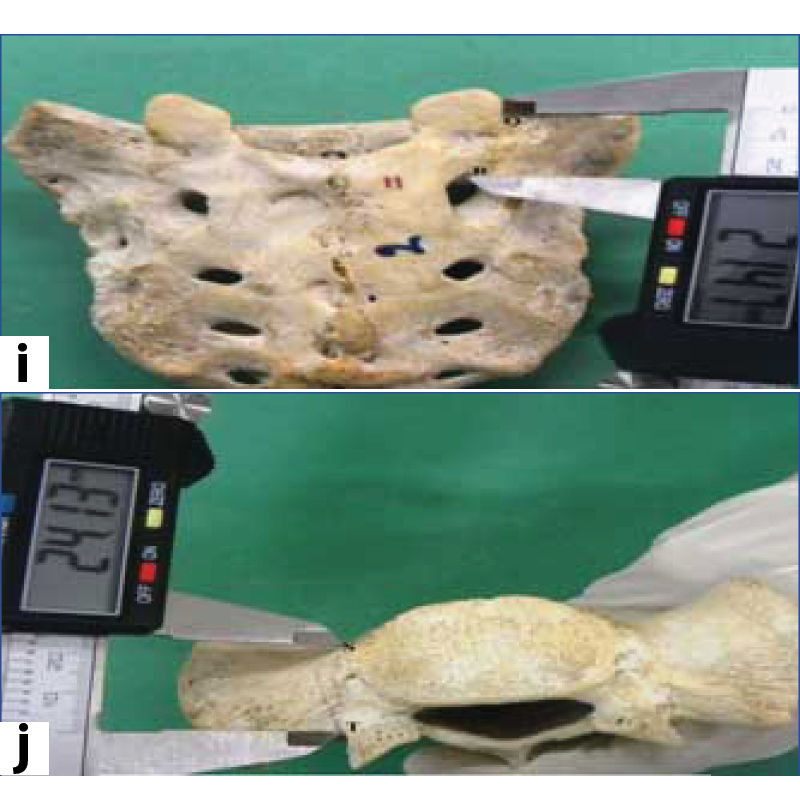
Pedicle depth (ST): Maximum distance between Point S and T on the anterior and posterior limits of pedicle, on base of sacrum on both sides [Table/Fig-1j].
Pedicle width (UV): Draw a line from the anterolateral edge of S1 body to lateral edge of first sacral articular process; take midpoint was taken as Point U, then draw a perpendicular line up to sacral canal on base of sacrum, measured on both sides [Table/Fig-1k].
k) Point U-mid-point of line drawn from anterolateral edge of first sacral body, point V-perpendicular drawn from point U upto upper border of sacral canal; l) Point X and Y-vertical diameter of auricular surface.
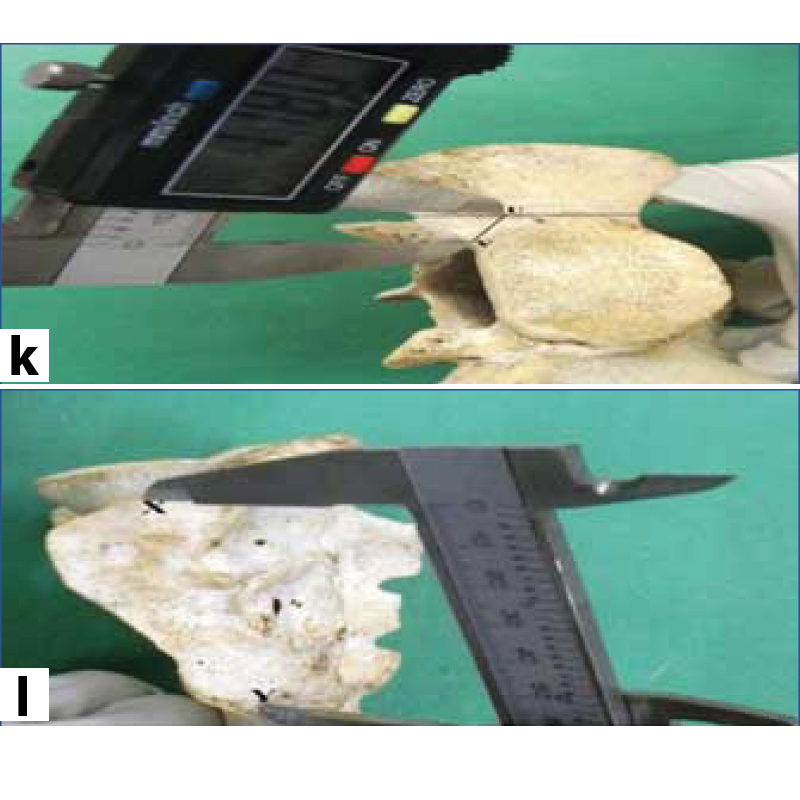
Vertical diameter of auricular surface (XY): Maximum vertical diameter of auricular surface measured on both sides [Table/Fig-1l].
Transverse diameter of auricular surface (ZO): Maximum transverse diameter of auricular surface measured on both sides [Table/Fig-1m].
Point Z and A-transverse diameter of auricular surface.

Statistical Analysis
The data were analysed, using SPSS version 16.0 and compared using Student’s t-test with p value <0.05 taken as significant.
Results
Results of linear parameters were shown in [Table/Fig-2]. Sacral length in males was found to be 10.57±0.95 cm, in females it was 8.56±0.49 cm, with statistically significant difference between the two groups, suggesting longer sacral length in males. Second sacral body height was found 2.55±0.23 cm in males and 2.16±0.20 cm in females, values are greater in males than females with statistically significant difference between two groups. Sacral canal anteroposterior diameter in males was 2.31±0.33 cm and 2.07±0.36 cm in females with significant difference between the two groups. Vertical diameter of auricular surface on right side showed values were higher in males (5.43±0.40 cm) than in females (5.07±0.37 cm). Rest all linear parameters showed no significant gender and side difference.
Discussion
Complex anatomy of first sacral vertebra with various important neurovascular structures lying in the vicinity of sacrum makes the dorsal screw placement at appropriate position a tough challenge for spine surgeons. Various factors such as race, sex, environmental factors and life style affect the morphology of bones [13]. Lumbosacral junction is considered to be a sensitive region where degenerative changes are seen. In operative stabilisation, insertion of screws is to be done into first sacral body, second sacral body and sacroiliac joint where complications like nonunion and pseudoarthrosis are very common [14]. Screws can be placed in anteromedial direction (in promontorium) and anterolateral direction (in sacral wing) using entry point just inferolateral to the first sacral facet traverses the pedicle to enter into first sacral body or into sacral wing [15]. Pedicle forms the basis for dorsal screw placement, as it the strongest portion of vertebrae. Transpedicular instrumentation is biomechanically superior than other available posterior instrumentation techniques [16].
Various neurovascular structures like median vessels lying in the middle of ventral surface of sacrum and iliac vessels along with sacral plexus are situated lateral to sacral foramina [7]. Sacral canal also contains nerve roots forming cauda equina below the level of second sacral vertebra. Safety zone for screw placement includes the area above first anterior foramen projection and between first and second anterior foramina projections [1]. Robertson PA and Plank LD evaluated the CT scans of upper sacrum in 100 patients and found that screws can be placed in anteromedial direction from both sides into first sacral body in almost 98.5% cases [17]. Various studies on sacral parameters were conducted using imaging techniques. Measurement of sacrum with spiral CT was done by Meng-jun LI et al., in which the angle and length of pedicle and lateral mass screw trajectories were measured [7]. It is useful for raising the accuracy rate of pedicle screw placement. Radiographic evaluation of sacrum was done by Xu R et al., He concluded that dorsal screw and iliosacral screw placement are best evaluated by inlet and outlet radiographs [1]. Various studies on sacral parameters were conducted in Western Anatolian population [12,15], in Central region of India and also in Eastern part of India. The present study was compared with other regional studies [Table/Fig-3] [18,19].
| S.No. | Parameters (cm) | Male/female | n | Mean±SD | p-value |
|---|
| 1 | Length (AB) | Male | 24 | 10.57±0.95 | <0.001 |
| Female | 24 | 8.56±0.49 | <0.001 |
| 2 | Breadth (CD) | Male | 24 | 9.95±0.64 | 0.36 |
| Female | 24 | 10.13±0.69 | 0.36 |
| 3 | S1 Height (EF) | Male | 24 | 2.98±0.29 | 0.92 |
| Female | 24 | 2.98±0.25 | 0.92 |
| 4 | S2 Height (GH) | Male | 24 | 2.55±0.23 | <0.001 |
| Female | 24 | 2.16±0.20 | <0.001 |
| 5 | PPH-Rt (QR) | Male | 24 | 2.05±0.22 | 0.64 |
| Female | 24 | 2.02±0.23 | 0.64 |
| 6 | PPH-Lt (QR) | Male | 24 | 2.10±0.25 | 0.11 |
| Female | 24 | 1.99±0.22 | 0.11 |
| 7 | FSBAP (IJ) | Male | 24 | 2.91±0.35 | 0.14 |
| Female | 24 | 3.04±0.24 | 0.14 |
| 8 | FSBT (KL) | Male | 24 | 4.77±0.38 | 0.60 |
| Female | 24 | 4.83±0.51 | 0.60 |
| 9 | SCAP (MN) | Male | 24 | 2.31±0.33 | 0.02 |
| Female | 24 | 2.07±0.36 | 0.02 |
| 10 | SCT (OP) | Male | 24 | 2.95±0.34 | 0.28 |
| Female | 24 | 2.86±0.22 | 0.28 |
| 11 | VDAS-Rt (XY) | Male | 24 | 5.43±0.40 | <0.001 |
| Female | 24 | 5.07±0.37 | <0.001 |
| 12 | VDAS-Lt (XY) | Male | 24 | 5.30±0.48 | 0.09 |
| Female | 24 | 5.09±0.37 | 0.09 |
| 13 | TDAS-Rt (ZO) | Male | 24 | 3.53±0.33 | 0.69 |
| Female | 24 | 3.49±0.46 | 0.69 |
| 14 | TDAS-Lt (ZO) | Male | 24 | 3.51±0.38 | 0.97 |
| Female | 24 | 3.50±0.45 | 0.97 |
| 15 | PW-Rt (UV) | Male | 24 | 1.20±0.19 | 0.36 |
| Female | 24 | 1.26±0.25 | 0.36 |
| 16 | PW-Lt (UV) | Male | 24 | 1.20±0.18 | 0.16 |
| Female | 24 | 1.30±0.25 | 0.16 |
| 17 | PD-Rt (ST) | Male | 24 | 2.70±0.23 | 0.68 |
| Female | 24 | 2.66±0.29 | 0.68 |
| 18 | PD-Lt (ST) | Male | 24 | 2.81±0.29 | 0.23 |
| Female | 24 | 2.70±0.35 | 0.23 |
PPH- Posterior pedicle height, FSBAP- First sacral body anteroposterior diameter, FSBT- First sacral body transverse diameter, SCAP- Sacral canal anteroposterior diameter, SCT- Sacral canal transverse diameter, VDAS- Vertical diameter of auricular surface, TDAS- Transverse diameter of auricular surface, PW- Pedicle width, PD- Pedicle depth.
*Rt- Right, **Lt- Left, SD- Standard deviation
Significant p-value (<0.001) were observed in SL, S2 ht and VDAS (Rt)
Variables of sacrum in different studies.
| S.No. | Parameters | Present Study (n=50) | Western Anatolian Population [15] (n=60) | Turkey Population [16] (n=100) | Central Region of India [11] (n=50) | Eastern Population of India [17] (n=250) |
|---|
| 1 | Sacral Length (AB) | M-10.57±0.95 cmF- 8.56±0.49 cm | M-10.43±1.24 cmF- 10.20±1.20 cm | | M-10.29±0.68 cmF-9.09±0.22 cm | M-10.82±0.67 cmF-9.93±0.74 cm |
| 2 | Sacral Breadth (CD) | M-9.95±0.64 cmF-10.13±0.69 cm | M-10.20±1.20 cmF-10.84±0.60 cm | | M-10.04±0.72 cmF-10.57±0.33 cm | M-9.63±0.74 cmF-9.56±0.74 cm |
| 3 | First Sacral Body Height (EF) | M-2.98±0.29 cmF-2.98±0.25 cm | M-3.06±0.31 cmF-2.98±0.24 cm | 3.02±0.23 cm | | |
| 4 | First Sacral AP Diameter (IJ) | M-2.91±0.35 cmF-3.04±0.24 cm | M-3.17±0.28 cmF-3.03±0.28 cm | 3.14±0.28 cm | M-2.94±0.24 cmF-2.97±0.25 cm | M-2.94±0.38 cmF-2.79±0.27 cm |
| 5 | First Sacral Body Transverse Diameter (KL) | M-4.77±0.38 cmF-4.83±0.51 cm | M-5.27±0.61 cmF-5.26±0.79 cm | 4.94±0.58 cm | M-4.57±0.45 cmF-4.70±0.48 cm | M-4.16±0.85 cmF-3.97±0.52 cm |
| 6 | Sacral Canal AP Diameter (MN) | M-2.31±0.33 cmF-2.07±0.36 cm | M-1.46±0.37 cmF-1.55±0.26 cm | | M-1.13±0.37 cmF-1.34±0.33 cm | |
| 7 | Sacral Canal Transverse Diameter (OP) | M-2.95±0.34 cmF-2.86±0.22 cm | M-3.10±0.24 cmF-2.97±0.25 cm | 3.13±0.32 cm | M-2.70±0.37 cmF-2.98±0.31 cm | |
| 8 | Posterior Pedicle Height (QR) | M Rt-2.05±0.22 cmLt-2.10±0.25 cm | M-2.09±0.23 cmF-2.09±0.22 cm | | M Rt-1.97±0.28 cmLt-2.00±0.33 cm | |
| F Rt-1.99±0.22 cmLt-2.03±0.22 cm | F Rt-1.82±0.19 cmLt-1.82±0.23 cm |
| 9 | Pedicle Depth (ST) | M Rt-2.70±0.23 cmLt-2.81±0.29 cm | M-2.26±0.26 cmF-2.41±0.38 cm | | M Rt-2.83±0.26 cmLt-2.85±0.25 cm | |
| F Rt-2.66±0.29 cmLt-2.70±0.35 cm | F Rt-3.06±0.75 cmLt-3.04±0.74 cm |
| 10 | Pedicle Width (UV) | M Rt-1.20±0.19 cmLt-1.20±0.18 cm | M-1.43±0.16 cmF-1.42±0.19 cm | | M Rt-1.24±0.24 cmLt-1.15±0.24 cm | |
| F Rt-1.26±0.25 cmLt-1.30±0.25 cm | F Rt-1.15±0.18 cmLt-1.23±0.16 cm |
| 11 | Vertical Diameter of Auricular Surface (XY) | Rt-5.43±0.40 cmM Lt-5.30±0.48 cm | M-5.77±0.41 cmF-5.47±0.45 cm | | | |
| Rt-5.07±0.37 cmF Lt-5.09±0.37 cm |
| 12 | Transverse Diameter of Auricular Surface (ZO) | Rt-3.53±0.33 cmM Lt-3.51±0.38 cm | M-3.75±0.67 cmF-3.63±0.67 cm | | | |
| Rt 3.49±0.46 cmF Lt-3.50±0.45 cm |
M*- males, F*- females. Second sacral body height was measured in the present study which was not included in others
Rt- Right, Lt- Left
In present study, sacral length gave an idea about the extent of area that can be operated on. Sacral length was found to be higher in males with statistically significant difference between the two values. Similarly, second sacral body height is important parameter as screws can be placed bilaterally in anterolateral and anteromedial directions for better fixation of lumbosacral junction [20]. Second sacral body height was found to be higher in males than females. In present study, sacral canal anteroposterior diameter was found to be higher in males, so narrower sacral canal in females can lead to greater risk as sacral canal contains indispensable neurovascular structures, vertical diameter of auricular surface was found to be higher in males suggesting easy sacroiliac screw placement in males than females.
Limitation
The present study was limited due to low sample size. Also, parameters were measured by manual methods and no imaging techniques were used.
Conclusion
In present study, Sacral length, Second sacral body height, Sacral canal antero posterior diameter and vertical diameter of auricular surface on right side were significantly higher in males, so in surgical procedures like dorsal screw fixation, ALIF, PLIF and iliosacral screw placement these parameters should be kept in mind to avoid neurovascular injuries. Data obtained from present study is similar to data from other regions in India, but it is mismatched with the European data. So in case of prosthesis and implant insertion these values would be of great importance.
PPH- Posterior pedicle height, FSBAP- First sacral body anteroposterior diameter, FSBT- First sacral body transverse diameter, SCAP- Sacral canal anteroposterior diameter, SCT- Sacral canal transverse diameter, VDAS- Vertical diameter of auricular surface, TDAS- Transverse diameter of auricular surface, PW- Pedicle width, PD- Pedicle depth.
*Rt- Right, **Lt- Left, SD- Standard deviation
Significant p-value (<0.001) were observed in SL, S2 ht and VDAS (Rt)
M*- males, F*- females. Second sacral body height was measured in the present study which was not included in others
Rt- Right, Lt- Left
[1]. Xu R, Ebraheim NA, Gove NK, Surgical anatomy of the sacrumAm J Orthop 2008 37(10):E177-81. [Google Scholar]
[2]. Sar C, Kilicoglu O, S1 pediculoiliac screw fixation in instabilities of the sacroiliac complex: biomechanical study and report of two casesJ orthop Trauma 2003 17(4):262-70.10.1097/00005131-200304000-0000412679686 [Google Scholar] [CrossRef] [PubMed]
[3]. Standring S, The Back & Pelvic girdle, Gluteal Region and Thigh. In: Newell RLM, Collins P, Healy JC, Mahadevan V editorsGray’s Anatomy: The anatomical basis of clinical practice 2008 40th edSpainChurchill Livingstone Elsevier:724-1349.10.1016/B978-0-443-06684-9.50088-3 [Google Scholar] [CrossRef]
[4]. Esses SI, Botsford DJ, Huler RJ, Rausching W, Surgical anatomy of sacrum: a guide for rational screw fixationSpine (Phila Pa 1976) 1991 16(6suppl):S283-88.10.1097/00007632-199106001-000211862426 [Google Scholar] [CrossRef] [PubMed]
[5]. Licht NJ, Rowe DE, Ross LM, Pitfalls of pedicle screw fixation in the sacrum: a cadaver modelSpine (Phila Pa 1976) 1992 17(8):892-96.10.1097/00007632-199208000-000061523492 [Google Scholar] [CrossRef] [PubMed]
[6]. Mirkovic S, Abitbol JJ, Steinman J, Edwards CC, Schaffler M, Massie J, Anatomic consideration for sacral screw placementSpine (Phila Pa 1976) 1991 16(6suppl):S289-94.10.1097/00007632-199106001-00022 [Google Scholar] [CrossRef]
[7]. Meng-jun LI, Guo-qiang DAI, Dong WANG, Jin-wu WANG, Hai-tao JIANG, Anatomical and biomechanical analysis of sacral pedicle and lateral massChinese J Traumatol 2011 14(1):29-35. [Google Scholar]
[8]. Wheeless CR, Nunley JA, Urbaniak JR, Wheeless textbook of orthopaedicsDuke University Medical center 2016 Duke University [Google Scholar]
[9]. Kaptanoglu E, Okutan O, Tekdemir I, Beskonakli E, Deda H, Closed posterior superior iliac spine impeding pediculocorporeal S-1 screw insertionJ Neurosurg 2003 99(2suppl):229-34.10.3171/spi.2003.99.2.022912956467 [Google Scholar] [CrossRef] [PubMed]
[10]. Ebraheim NA, Lu J, Yang H, Heck BE, Yeasting RA, Anatomic consideration of second sacral vertebra and dorsal screw placementSurg Radiol Anat 1997 19(6):353-57.10.1007/BF016285009479708 [Google Scholar] [CrossRef] [PubMed]
[11]. Ebraheim NA, Lin D, Xu R, Yeasting RA, Evaluation of upper sacrum by three dimensional computed tomographyAm J Orthop 1999 28(10):578-82. [Google Scholar]
[12]. Basaloglu H, Turgut M, Taser FA, Ceylan T, Basaloglu HK, Ceylan AA, Morphometry of sacrum for clinical useSurg Radiol Anat 2005 27(6):467-71.10.1007/s00276-005-0036-116211321 [Google Scholar] [CrossRef] [PubMed]
[13]. Nurzenski MK, Briffa NK, Price RI, Khoo BC, Devine A, Beck TJ, Geometric indices of bone strength are associated with physical activity and dietary calcium intake in healthy older womenJ Bone Miner Res 2007 22(3):416-24.10.1359/jbmr.06111517147487 [Google Scholar] [CrossRef] [PubMed]
[14]. Kubaszewski L, Nowakowski A, Kaczmarczyk J, Evidence-based support for S1 transpedicular screw entry point modificationJ Orthop Surg Res 2014 9:2210.1186/1749-799X-9-2224708681 [Google Scholar] [CrossRef] [PubMed]
[15]. Arman C, Naderi S, Kiray A, Aksu FT, Yilmaz HS, Tetik S, The human sacrum and safe approaches for screw placementJ clin Neurosci 2009 16:1046-49.10.1016/j.jocn.2008.07.08119442524 [Google Scholar] [CrossRef] [PubMed]
[16]. Castro-Reyes CD, Morales-Avalos R, Vilchez-Cavazos F, Garza-Castro DL, Salinas-Zertuche A, Aguirre POM, Morphometric characteristics of lumbar vertebral pedicles in mexican population. Implications for transpedicular lumbar fusion surgeryJ Morphol Sci 2015 32(1):37-42.10.4322/jms.072014 [Google Scholar] [CrossRef]
[17]. Robertson PA, Plank LD, Pedicle screw placement at the sacrum; anatomical characterization and limitations at S1J Spinal Disord 1999 12(3):227-33.10.1097/00024720-199906000-00011 [Google Scholar] [CrossRef]
[18]. Sinha MB, Rathore M, Trivedi S, Siddiqui AU, Morphometry of first pedicle of sacrum and its clinical relevanceInt J Health Biomed Res 2013 1(4):234-40. [Google Scholar]
[19]. Mazumdar S, Ray A, Mazumdar A, Majumdar S, Sinha A, Vasisht S, Sexual dimorphism and regional differences in size of sacrum: a study in Eastern IndiaAI Ameen J Med Sci 2012 5(3):298-06. [Google Scholar]
[20]. Liu J, Li Y, Wu Y, Zhu Q, An anatomic study on the placement of second sacral screw and its clinical applicationsArch Orthop Trauma Surg 2013 133(7):911-20.10.1007/s00402-013-1753-223636318 [Google Scholar] [CrossRef] [PubMed]