Hypotension is a common complication of neuraxial anaesthesia in obstetric patients [1]. Prophylactic routes have been suggested to reduce the incidence and severity of hypotension which includes fluid loading, left lateral uterine displacement, leg elevation, use of low dose local anaesthetics and the use of vasopressors. However, incidence of hypotension under spinal anaesthesia for c/s is common [1-4].
Spinal technique can be induced with patient in either the sitting or lateral decubitus position. Spread of local anaesthetic solution in Cerebrospinal Fluid (CSF) depends on patient posture [5]. This may have an impact on the incidence and severity of hypotension after intrathecal injection of the local anaesthetic [1]. Studies have shown that the patient’s position in the incidence of hypotension after spinal anaesthesia for c/s maybe effective [6-8]. Whether the use of the lateral or the sitting position is best for routine initiation of neuraxial anaesthesia for c/s is controversial [1].
The current study aimed to compare the maternal haemodynamic effects associated with sitting or lateral decubitus positions during induction of spinal anaesthesia for elective c/s.
Materials and Methods
After the Medical Ethics Committee approval (With ethical no: 92137N8 with IRCT no: 201402017013 N8) and written consent obtained from participants, 76 healthy pregnant women undergoing c/s were enrolled in this prospective, randomised, and double-blind clinical trial from September 2014 to August 2015 in Al-Zahra Hospital. Patients were selected by simple randomisation method. The inclusion criteria were physical status, American Society of Anaesthesiologists (ASA) І- П (it means, participants in this study were healthy or with mildly systemic disease) [9], aged 18-40 years and term pregnancy undergoing elective c/s with spinal anaesthesia. Exclusion criteria was pre-eclampsia, cardiovascular, respiratory, hepatic or renal problems, known allergy to local anaesthetics, contraindication for spinal anaesthesia and psychological disorder. The sample size was selected based on data driven from previous study [10]. We determined that an effective sample size (n=76), would be required for the current study to provide statistical power of 80% to detect a 15% difference of incidence of hypotension between two groups.
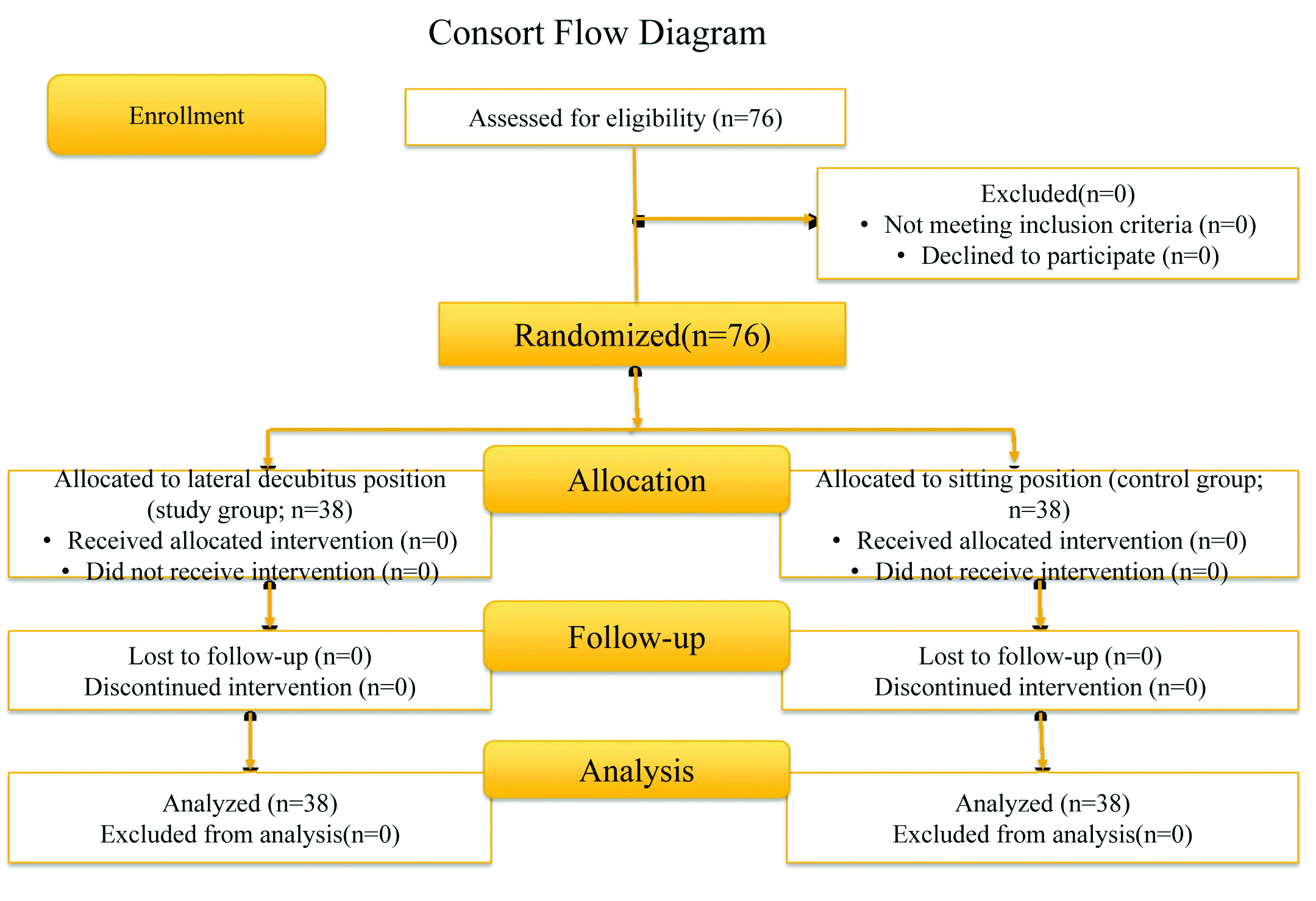
In operation theatre, routine standard monitoring with Non-Invasive Arterial Pressure (NIBP), Electrocardiography (ECG), and pulse-oximetry was established. Base line values were recorded. Each patient was preloaded with 8-10 mL/kg of Ringer solution over 15 minutes before induction of spinal anaesthesia. Parturient was allocated by box randomisation by sealed envelope, to one of the two groups, for positioning during induction of spinal puncture [Table/Fig-1]. Spinal puncture was performed with the parturient either in sitting (control group, n=38) or in left lateral decubitus position (study group, n=38).
Flow chart of patients enrolled to the study.
A 25-gauge Quinke needle (B-BRAUN Melsungen AG 34209 Germany) was used, through which 2 mL 0.5% hyperbaric bupivacaine and 15 μg fentanyl was administered for over 10 second. at the L3-4 or L4-5 level in the subarachnoid space. Following spinal injection, without delay, the parturient was smoothly and gradually laid supine with a wedge under right hip.
After spinal-anaesthetic injection, oxygen 4 to 6 L/minutes was delivered by nasal cannula, until delivery of baby. Level of sensory block by the anaesthesiologist performing the block using pin-prick sensation every two minute after the spinal injection was assessed. An upper level of T4 was considered adequate for surgery. Every two minute after the spinal injection until neonate delivery, assessments were made for haemodynamic parameters {Heart Rate (HR), Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), and Mean Arterial Pressures (MAP)}. Decrease in SBP> 25% of the baseline levels, was treated by incremental doses IV ephedrine 5 mg or phenylephrine 50 μg. Vasopressor requirements and timing of injection, total amount of fluids administered, incidence of peri-operative nausea and vomiting, and neonatal Apgar scores at 1 and 5 minute were recorded. We had no access to bedside echocardiography and cardiologist, so, we cannot assess haemodynamic variables by this modality.
Two anaesthesiologists; first for preparing the study solutions and management of anaesthesia, and the later with medical students who were unaware of study group, were responsible for recording the patient’s data.
Statistical Analysis
Statistical analysis was performed using SPSS version 16.0. Data were analysed using student’s t-test, Chi-square test, and Mann-Whitney U-test. A p-value ≤0.05 was considered to be significant.
Results
There were no significant difference between two groups with respect to maternal demographic data including age, weight, height, gravidity, duration of surgery, and causes of c/s [Table/Fig-2].
Demographic data in two study groups.
| Variables | Lateral group(n=38) | Sitting group(n=38) | p-value |
|---|
| Age (year) | 28.68±5.85 | 30.84±5.52 | 0.70 |
| Weight (kg) | 77.89±9.56 | 78.87±10.15 | 0.67 |
| Height (cm) | 159.47±3.65 | 159.74±3.58 | 0.94 |
| Gravidity (range) | 1-5 | 1-6 | 0.85 |
| Cause of C/S (%) | | | 0.31 |
| 8 (21.1) | 5 (13.2) | |
| CPD | 22 (57.1) | 26 (68.4) | |
| Repeat | 8 (21.1) | 5 (13.2) | |
| Elective | 0 (0) | 2 (5.3) | 0.53 |
| Others | 54.50±13.00 | 56.03±12.38 |
Duration of surgery (minute)
Data was presented as mean (SD) or median (range).
*Cephalopelvic Disproportion
Sensory block variables were shown in [Table/Fig-3]. In the sitting group 16 (42.10%) and lateral group 18 (47.36%) patients had highest sensory block >T4 level (p=0.91). The median sensory block level were not significant in two groups (p=0.89).
Obstetric and anaesthesia variables in two study groups.
| Variables | Lateral group(n=38) | Sitting group(n=38) | p-value |
|---|
| Upper sensory block (dermatome) | T5 (T3-T6) | T5 (T3-T6) | 0.89 |
| Sensory block level>T4 | 18 (47.36) | 16 (42.10) | 0.91 |
| Sustained hypotension | 1 (2.6) | 8 (21.1) | 0.014 |
| Nausea-Vomiting (%) | 0 (0) | 3 (7.9) | 0.12 |
| Unconsciousness (%) | 0 (0.0) | 0 (0.0) | 1.00 |
| Respiratory depression (%) | 1 (2.6) | 4 (10.5) | 0.18 |
| SPO2<90% (%) | 1 (2.6) | 2 (5.3) | 0.50 |
| Total IV fluid(mL) | 2590.79±265.55 | 2602.63±323.19 | 0.25 |
| Duration of sensory block (min) | 65.71±5.02 | 72.74±5.8 | 0.42 |
| Duration of motor block (minute) | 74.76±6.60 | 81.29±5.40 | 0.29 |
Data were presented as mean (SD), median (range) and number (%).
Maternal haemodynamic was presented in [Table/Fig-4]. Base line HR, SBP, DBP and MAP values were matched in both groups. There were significant changes from base value in HR after spinal anaesthesia at the study period in each group. Bradycardia occurred in 8 (21.1%). Patients of sitting position which required treatment with atropine, while none of the patients in the lateral group had bradycardia. Blood pressure was affected by the position used for induction of spinal block. Hypotension (fall in SBP>25% of base value) occurred in 29 (76.3%) patients in group S, and 19 (50.0%) patients in group L (p=0.016). As well as, duration of hypotension was significantly greater in group S (p=0.002). In group S, 29 (76.31%) patients and in group L 14 (36.20%) patients required vasopressor ephedrine or phenylephrine or both (p=0.01).
Perioperative maternal variables and neonatal Apgar scores in two study groups.
| Variables | Lateral group(n=38) | Sitting group(n=38) | p-value |
|---|
| Baseline haemodynamic data | |
| SBP (mmHg) | 126.50±7.21 | 123.97±12.03 | 0.09 |
| DBP (mmHg) | 79.89±8.69 | 77.66±11.53 | 0.22 |
| MAP (mmHg) | 94.18±9.11 | 91.87±11.79 | 0.34 |
| HR (bmp/min) | 95.66±13.81 | 99.18±17.93 | 0.10 |
| SPO2(%) | 97.16±0.89 | 97.13±0.93 | 0.96 |
| Prevalence of hypotension (%) | 19(50.0) | 29(76.3) | 0.016 |
| Time of first hypotension (minute) | 5.05±2.147 | 5.24±2.23 | 0.14 |
| Duration of hypotension (minute) | 8.63±2.73 | 12.21±7.18 | 0.002 |
| Maximum hypotension value (mmHg) | 73.83±10.71 | 80.53±7.72 | 0.11 |
| Vasopressor need (%) | 14(36.20) | 29(76.31) | 0.012 |
| Ephedrine dose (mg) | 10.52±31.10 | 36.84±58.9 | <0.001 |
| Bradycardia (%) | 0(0) | 8(21.1) | 0.014 |
| Atropine dose (mg) | 0.01±0.08 | 0.09±0.28 | 0.001 |
| Metoclopramide dose (mg) | 0.00±0.00 | 0.13±0.81 | 0.04 |
| Midazolam dose (mg) | 0.05±0.22 | 0.10±0.31 | 0.09 |
| Neonatal Apgar scores at: | |
| 1 minute | 9.26±0.44 | 8.92±0.81 | 0.91 |
| 5 minute | 10.00±0.45 | 9.87±0.52 | 0.87 |
Data were presented as mean (SD) and number (%).
Intraoperative side effects and neonatal Apgar score was shown in [Table/Fig-4]. There was significant differences in frequency of sustained hypotension between two groups (21.1% vs. 2.6%; p=0.014). There were no differences in other side effects among two groups.
There were no differences in neonatal Apgar scores at one min of delivery, but mean neonatal Apgar scores in five min was higher in lateral with p-value=0.87 that was not significant.
Discussion
Neuraxial anaesthesia is a safest and preferred method for c/s but it has some complications and effects on maternal haemodynamic [11]. Maternal haemodynamic instability is a common event in spinal anaesthesia that can affect mother and infant status. Traditionally, it was said that other positions has implications on resolving of this problem. Few studies investigated possible correlation between position effect and haemodynamic stability. Prophylactic routes such as pre-anaesthesia hydration, vasopressors or leg rise are performed before spinal anaesthesia but had not dramatic role in prevention of hypotension [12].
Present study showed that the lateral position is associated with greater haemodynamic stability, less vasoconstrictor use, lower side effects, and better neonatal status, when compared with the sitting position [5]. In this study, hypotension was recorded in 63.15% of all patients. This indicates that despite the methods of prevention, the complete prevention of hypotension during c/s is not possible. Generally, the sympathetic blockade usually results in hypotension whether the patient in the sitting or the lateral position [6,7]. Previous studies have shown that the prevalence and severity of hypotension is associated with the height of block, such as Carpenter RL et al., and Morgan P et al., study [13,14].
In this study, we didn’t demonstrate any difference in height of sensory block after spinal anaesthesia between two groups. This finding was contrary to study of Coppejans et al., which reported a greater number of patients in lateral decubitus had a higher sensory block level than patients in sitting position. He also concluded that performing a CSE technique for caesarean delivery in the sitting position was technically easier and induced less severe hypotension, females in the sitting postion required less ephedrine (p=0.012) but in the lateral group, blocks extended more cephalad than with the sitting position (p=0.014) [7].
Haemodynamic instability could be due to the vasovagal episode that might occur with a great frequency or severity in the sitting position and additional gravity dependent peripheral pooling may result in decrease in cardiac output, orthostatic hypotension and uterine blood flow in sitting position [8]. Also, it could be related to slower recovery from sympathectomy induced venous pooling in the lower extremities on assuming supine position vs. the sitting position [15].
Thus, the use of vasoconstrictors was more in sitting position, because the duration of hypotension was longer in the sitting position.
Episodes of bradycardia requiring treatment were more in sitting position. Jackson N and Peterson Brown S, stated that vasovagal reflexes are not rare in regional anaesthesia and their rate is up to 90% [16]. These findings were almost similar to what has been reported previously. In Yun EM et al., study, maternal HR rate and SPO2 at the start of the study were 102±15 bpm and 100%±0.5%, respectively, in the sitting group [17]. In the study of Shahzad K, and Afshan G, also bradycardia which required treatment occurred more in the sitting position [18]. However, this difference was not statistically significant. This finding could be due to activation of parasympathetic nervous system in the face of sympathetic block develop, which occurred more commonly in the sitting position [8].
In one study, the effect of the lithotomy position on the Systolic Blood Pressure (SBP) with the horizontal position after spinal block was evaluated five minute after spinal block. The SBP elevated by the lithotomy position (n=14) from a 16% decrease to an 8% decrease. On the contrary, in the horizontal group (n=14), SBP decreased 16% at 5 minute and continued to decrease to 21% [19]. On the other hand, the head-down position have no effect on the incidence of hypotension during spinal anaesthesia for caesarean delivery [20]. The survey about preservation of BP on assumption of the prone position in patients during low spinal anaesthesia suggests better preservation of autonomic nervous system compensatory mechanisms during low spinal anaesthesia than with general anaesthesia [21]. Frölich MA Caton D, revealed that higher baseline HR, it means higher sympathetic tone may be a useful parameter to predict after spinal anaesthesia hypotension [22]. In other study were showed that maternal haemodynamic were significantly improved in the lateral positions as compared to the sitting position with respect to maternal cardiac index stroke, volume index, heart rate and systolic blood pressure. They showed that position has no effect on blood flow to the healthy foetus. Currently, these results were confirmed [23]. Mavridou I et al., suggested that although, maternal positioning is a routine practice, but has not been shown to be sufficient to prevent or relieve spinal hypotension [24].
There was no significant difference in the incidence of maternal side effects (nausea, vomiting, respiratory depression, and decrease in SPO2) between two groups. But consumption of metoclopramide was greater in sitting position.
All neonates had good Apgar scores at 1 and 5 minute after delivery. This may be explained by the fact that only healthy women were scheduled in this study. Mean Apgar score at 5 min was better in the study group. This may be due to placental flow and gas exchange maintain more effectively in lateral position compared to the sitting position. We did not obtain umbilical cord PH, because it is practice at our hospital to obtain these only when the Apgar score is ≤ 7 at 1 or 5 min.
Limitation
Mother’s body mass index has possible effects on haemodynamic as higher chances of induced hypotension and other comorbid disease that affected studied variables [22], were not considered in our study. We had no access to Doppler ultrasonography or bedside echocardiography
Conclusion
Results of present study revealed that changes in maternal haemodynamic, side effects, and use of vasopressors were lower when spinal anaesthesia induced in lateral position. In addition, neonatal Apgar scores were improved in this position. These results were parallel with previous studies which confirmed effect of supine versus position on speed of onset of block sensory and its implications on maternal haemodynamic. However, it is clear that sever hypotension has important effects on maternal and fetus outcomes and by prevention of hypotension, we can reduce them.
Duration of surgery (minute)
Data was presented as mean (SD) or median (range).
*Cephalopelvic Disproportion
Data were presented as mean (SD), median (range) and number (%).
Data were presented as mean (SD) and number (%).