Bronchogenic Cyst over Sternum–An Unusual Location
Amol Jagdale1, Shopnil Prasla2, Saurav Mittal3
1 Professor, Department of Radiology, Dr. Vasantrao Pawar Medical College and Research Center, Nashik, Maharashtra, India.
2 Junior Resident, Department of Radiology, Dr. Vasantrao Pawar Medical College and Research Center, Nashik, Maharashtra, India.
3 Junior Resident, Department of Radiology, Dr. Vasantrao Pawar Medical College and Research Center, Nashik, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shopnil Prasla, Junior Resident, Department of Radiology, Dr. Vasantrao Pawar Medical College and Research Center, Nashik-422003, Maharashtra, India.
E-mail: shopnilp@yahoo.com.au
Bronchogenic cyst is congenital anomaly arising from the abnormal budding of the tracheobronchial tree during foregut maturation. The cyst is most commonly located in mediastinum and intraparenchymal region. Suprasternal region is considered as rare location for bronchogenic cyst to occur. Most of the cases of the cyst have been reported in male patient within paediatric age group. We report a 13-year-old female child with a swelling present over suprasternal region in midline since birth. Surgical excision was done and diagnosis was confirmed by histopathological examination.
Cutaneous, Pseudostratified, Suprasternal, Swelling
Case Report
A 13-year-old female child presented to our department with complaint of swelling in midline over sternal notch since birth. There was no associated complaint and past medical history or congenital anomaly. On inspection, the swelling appeared as well defined oval mass measuring approximately 2.5 cm x 2.5 cm in size noted at the suprasternal notch. The skin over the swelling appeared normal with no signs of inflammation or punctum over swelling. On palpation the swelling was soft in consistency, non tender, mobile with overlying skin freely moving in all direction. Patient didn’t complain any discharge through swelling and no sinus tract was evident on examinations.
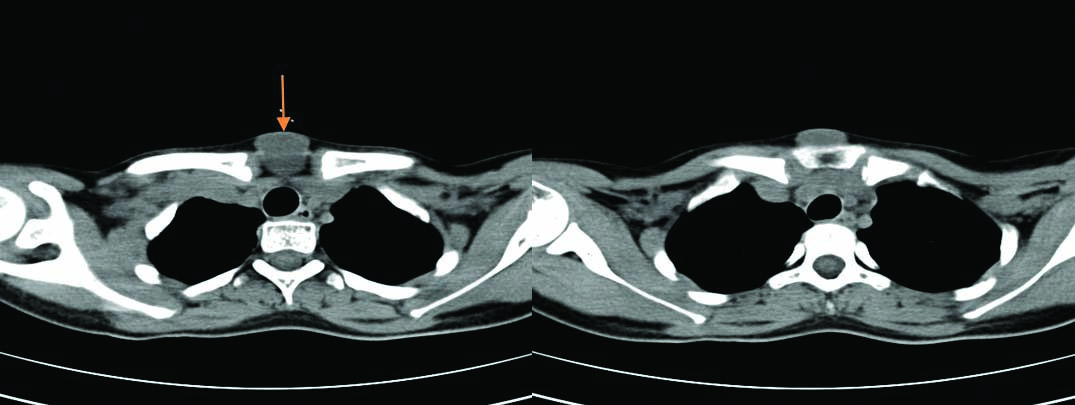
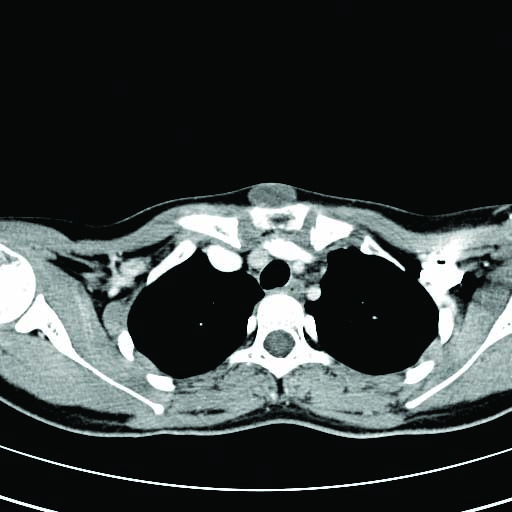
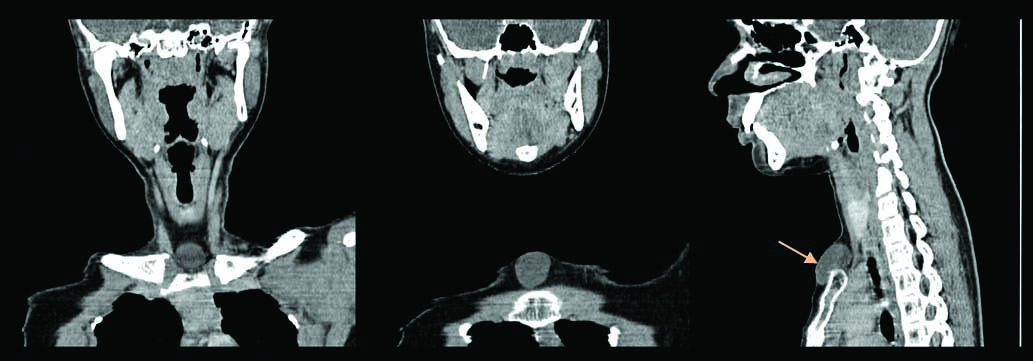
Multislice pre and post contrast serial axial sections of CT scan neck were taken which showed a well-defined midline non-enhancing lesion measuring 2.5 cm x 2.8 cm noted in the surpasternal inter-clavicular region. The lesion extends anterior to the sternum with no associated bony erosion. Sub centimeter sized bilateral Level I lymph nodes were also seen [Table/Fig-1,2]. Coronal and Sagittal section showing swelling over suprasternal notch anteriorly [Table/Fig-3].
Pre contrast axial section showing midline lesion over suprasternal region extending anterior to the sternum.(orange arrow).
Post contrast axial section showing midline non-enhancing lesion over suprasternal region extending anterior to the sternum.
Coronal and Sagittal section (orange arrow) showing swelling over suprasternal notch anteriorly.
The surgical excision was done under general anesthesia and the specimen was sent for histopathological examination. Macroscopically specimen consists of oval soft tissue mass measuring 3 cm x 2.5 cm x 2 cm in size. Externally the mass showed small fatty nodules. On cut section, brown fluid exuded out of the cyst [Table/Fig-4].
Excised cyst with few fatty nodules noted externally.

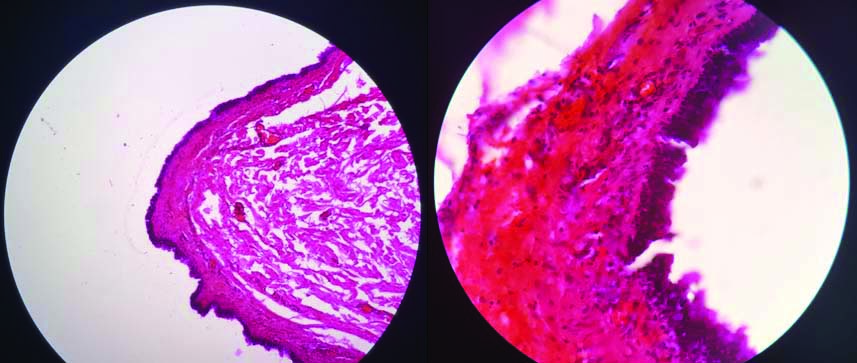
The microscopic examination revealed cyst wall lined by pseudostratified columnar epithelium. Underlying tissue showed fibrocollagenous tissue displaying congestion and focal mononuclear cell infiltration thus confirming diagnosis [Table/Fig-5]. All these features along with the radiological correlation confirmed the diagnosis of cutaneous bronchogenic cyst over sternum.
Histopathological slide stained with haematoxylin and eosin shows cyst lined by pseudostratified columnar epithelium with underlying fibrocollagenous tissue (40X).
Discussion
Endodermal cysts are speculated to originate from the evolving gastrointestinal system and rarely from respiratory system. Endodermal cyst with respiratory epithelium lining is termed as bronchogenic cyst. Bronchogenic cyst is commonly located in mediastinum mainly posterior to the carina and intrapulmonary region, cutaneous suprasternal location is particularly a rare location [1]. Sternal cutaneous bronchogenic cyst is extremely rare condition with very few cases noted in literature having incidence of 1 in 42000 to 1 in 68000 people [2,3]. Bronchogenic cyst was first reported in 1911 by Blackader AD and Evans DJ the first case of cutaneous bronchogenic cyst over sternum was reported by Seybold WB and Clagett OT in 1945 [4,5]. Bronchogenic cyst is a congenital entity occurring due to the embryonic primitive foregut anomaly. In the beginning of the 5th week of gestation, primitive foregut is divided into dorsal and ventral foregut by laryngotracheal groove. By end of the 7th week of gestation foregut separates into dorsal part which extends to form esophagus and ventral part transforms into tracheobronchial tree. Abnormal budding in the ventral foregut leads to abnormal development of tracheobronchial tree mostly on the distal part thus forming blind ended fluid filled pouch termed as bronchogenic cyst [1,6]. The theory postulated for cutaneaous bronchogenic cyst arising from the midline as present in our case is mostly due to anterior relocation of intrathoracic cyst or being pinched off by the merging sternal bars on the evolving anterior portion of lung buds [7]. On evaluating the literature we found that bronchogenic cyst have more predilection for males as compared to female with ratio 4:1 thus making our case rarer because of the female patient [1,6-9].
The most frequent location of cutaneous bronchogenic cyst is suprasternal area accompanied by presternal area, neck and scapula. Other unusual location like chin, posterior neck, shoulder, base of tongue and abdominal cases have also been reported [8]. Cutaneous bronchogenic cyst is usually asymptomatic as seen in our patient, but sometimes continuous epithelial secretion causes cyst to grow larger. Large cyst may compress the adjacent structure producing symptom such as dyspnea, respiratory distress, cough and dysphagia. Rarely secondary infection causes sinus tract formation with external purulent discharge located superficially and abscess formation on deeper locations [10]. Such cyst can be complicated by rupture, haemorrhage and malignant transformation. Possibility of malignant transformation arising from these cysts has been recognized as anaplastic carcinoma, squamous cell carcinoma, bronchoalvelolar carcinoma and rhabdomyosarcoma [3]. Transformation into malignant melanoma or mucoepidermoid carcinoma can be seen, though very rarely [9,11].
The radiological evaluation along with histopathological correlation helps to diagnose the cyst. On plain radiography cyst represent as opaque lesion with homogenous density which is likely because of the retained secretion [12]. Ultrasonography finding reveals anechoic lesion with or without hyper echogenic debris showing variable internal echogenicity. CT is excellent imaging tool for identifying the nature of cystic lesion whether solid or fluid filled lesion. On CT scan evaluation bronchogenic cyst show well circumscribed spherical lesion with smooth or lobulated border. These lesion appear homogeneous with decreased attenuation ranging from 0 to 20 HU equivalent that of fluid filled lesion. In case of increased attenuation, either presence of haemorrhage or proteinaceous secretion should be considered. Cyst does not show any enhancement on the intravenous contrast study [13]. MRI is important in manifesting the size and shape of the cyst and in deciding its position in correlation with other structures [10]. Commonly simple fluid filled cyst on MRI shows very low signal intensity on T1 weighted images. But bronchogenic cyst shows intermediate to higher signal intensity on T1 due to presence of protein and other paramagnetic structure in the cyst and very high signal intensity on T2 weighted images [13].
Cutaneous bronchogenic cyst is mostly lined by ciliated pseudostratified columnar epithelium typical of respiratory origin with fibroconnective tissue overlying it. The tissue wall consists of the seromucinous glands, smooth muscle fibers and cartilage [10]. On rare occasion presence of lymphoid follicle may be seen in cutaneous bronchogenic cyst. However, presence of lymphoid follicles favors branchial origin and eliminates bronchogenic origin [7,14]. In this case, histopathological study did not reveal presence of lymphoid follicles thus supporting our diagnosis towards bronchogenic cyst.
Lesions having pseudostratified columnar epithelium like branchial cyst and thyroglossal cyst should also be considered in the differential diagnosis. Branchial cyst and thyroglossal cyst are located in anterior aspect of sternocleidomastoid muscle and anterior aspect of the neck in midline respectively. Both cyst do not show presence of smooth muscle fibers, cartilage or mucous gland. Other differential diagnosis is mature teratoma, cutaneous ciliated epithelium, dermoid and epidermoid inclusion cyst [9].
Differential diagnosis solely based on imaging includes thyroglossal cyst, and ectopic thyroid gland. These entities can however be differentiated based on imaging properties. Thyroglossal cyst shows well defined fluid attenuation mass having thin wall with rim enhancement on contrast enhanced scans, and are mostly in midline [2]. Ectopic thyroid gland appears hyperdense on plain scans and shows homogenous contrast enhancement [15].
As far as management is concerned, complete surgical excision of the cyst should be done to avoid unnecessary complication of recurrence due to incomplete excision and to avoid the potential malignant transformation [7].
Conclusion
We conclude a case of bronchogenic cyst in female patient with unusual location over suprasternal notch. Histopathological study is essential in confirming the diagnosis and differentiating cyst from the other differential diagnosis. Though our patient was asymptomatic but complete excision was done to avoid unwanted complication and malignant transformation.
[1]. Malik KA, Sternal bronchogenic cyst: a rare conditionPakistan Journal of Medical Sciences 2009 25(6):1007-08. [Google Scholar]
[2]. Mittal MK, Malik A, Sureka B, Thukral BB, Cystic masses of neck: A pictorial reviewThe Indian Journal of Radiology and Imaging 2012 22(4):33410.4103/0971-3026.11148823833426 [Google Scholar] [CrossRef] [PubMed]
[3]. Niño-Hernández LM, Arteta-Acosta C, Redondo-De Oro K, Alcalá-Cerra L, Redondo-Bermúdez C, Marrugo-Grace O, Cervical bronchogenic cyst mimicking thyroglossal cyst. Case report and review of literatureCir Cir 2011 79:330-33. [Google Scholar]
[4]. Blackader AD, Evans DJ, A case of mediastinal cyst producing compression of the trachea ending fatally in an infant of nine monthsArch Paediat 1911 28:194-200. [Google Scholar]
[5]. Seybold WB, Claggett OT, Presternal CystsJ Thoracic Surg 1945 14:217-20. [Google Scholar]
[6]. Park HS, Son HJ, Kang MJ, Cutaneous bronchogenic cyst over the sternumKorean Journal of Pathology 2004 38:333-36. [Google Scholar]
[7]. Manchanda V, Mohta A, Khurana N, Das S, Subcutaneous bronchogenic cystJournal of Cutaneous and Aesthetic Surgery 2010 3(3):18110.4103/0974-2077.7449821430834 [Google Scholar] [CrossRef] [PubMed]
[8]. Farag M, Naguib N, Izzidien A, Bronchogenic cyst: case report and review of literatureWest London Medical Journal 2010 2(3):01-04. [Google Scholar]
[9]. Alar T, Muratli A, A rare presentation of a bronchogenic cyst: presternal, subcutaneous and 42-year-old manTüberk Toraks 2012 60(1):59-61.10.5578/tt.216422554369 [Google Scholar] [CrossRef] [PubMed]
[10]. Moz U, Gamba P, Pignatelli U, D’addazio G, Zorzi F, Fiaccavento S, Bronchogenic cysts of the neck: a rare localization and review of the literatureActa Otorhinolaryngol Ital 2009 29(1):36-40. [Google Scholar]
[11]. Govaerts K, Van Eyken P, Verswijfel G, Van der Speeten K, A bronchogenic cyst: presenting as a retroperitoneal cystic massRare Tumors 2012 4(1):1310.4081/rt.2012.e1322532911 [Google Scholar] [CrossRef] [PubMed]
[12]. Kaur S, Goyal R, Juneja H, Sood N, Intrapulmonary air filled bronchogenic cyst: a rare entityIndian Journal of Radiology and Imaging 2006 16(4):86510.4103/0971-3026.32370 [Google Scholar] [CrossRef]
[13]. McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, Matsumoto S, Bronchogenic cyst: imaging features with clinical and histopathologic correlation 1Radiology 2000 217(2):441-46.10.1148/radiology.217.2.r00nv1944111058643 [Google Scholar] [CrossRef] [PubMed]
[14]. Kim DH, Kim HK, Lee JW, Lee HI, Park KY, Li K, A case of cutaneous bronchogenic cyst presenting with lymphoid folliclesAnnals of Dermatology 2011 23(3):392-95.10.5021/ad.2011.23.3.39221909217 [Google Scholar] [CrossRef] [PubMed]
[15]. Zander DA, Smoker WR, Imaging of ectopic thyroid tissue and thyroglossal duct cystsRadiographics 2014 34(1):37-50.10.1148/rg.34113505524428281 [Google Scholar] [CrossRef] [PubMed]