Martin Kirschner introduced K-wires in 1909, and since then it is widely popular in Orthopaedics. K-wires can be introduced percutaneously, under the guidance of image intensifier, which makes the procedure easy, less time consuming and less invasive than open reduction. K-wire is universally used for the treatment of hand fractures, wrist, foot, ankle surgeries and long bone fractures in children and adults [1-7]. K-wire fixation provides rigid fixation after adequate reduction, which can allow early mobilisation of the adjacent joints [8]. After fracture fixation, the wires may be left buried under the skin or unburied.
The most common complication of K-wire fixation is pin site infection, which is reported to be as high as 28% [9]. Pin site infection is a noted complication ever since K-wire was introduced. Though, there are few studies comparing the infection rate between buried and unburied K-wires, there is still no consensus on whether the K-wires should be left buried under the skin or left unburied [10-16]. Those who advocate that K-wires should be buried under the skin, believe that it reduces the chances of pin site infection and those who support leaving wires unburied, find it cost effective and easy for subsequent removal [10-13]. However, these infections could lead to osteomyelitis, septic arthritis, malunion, nonunion and possible sequelae of joint stiffness and deformities, it is necessary to come to a consensus whether K-wires should be buried or unburied to prevent or atleast reduce the chances of these infections [17]. The purpose of present study was to determine whether burying K-wires reduces the infection rate in fracture fixation compared to unburied K-wires.
Materials and Methods
A multi centric retrospective cohort study in patients from two tertiary care centres of Puducherry, India. The patients underwent K-wire fixation for fractures in upper limbs and lower limbs during the time period between January 2010 to August 2017. We had a total of 474 patients with the required data. Institutional review board clearance was obtained prior to the present study.
The data were retrieved from medical records and radiology archives. For each patient we recorded patient demographic data, site of fracture, whether fracture was open or closed, number of days of hospital stay, whether K-wires were buried or unburied under the skin and whether there was pin site infection or not while the K-wires were insitu. We included only the patients with adequate follow up till the wire removal. We excluded patients who had pathological fractures and those who had infection at the surgical site prior to the surgery. We defined the presence of infection as documented clinical signs of infections such as raised local temperature with erythema, serous or pus discharge at the pin site as well as prolonged hospital stay with intravenous antibiotic treatment or those who warranted operative debridement.
Statistical Analysis
Statistical analysis was done using SPSS version 23.0. Baseline characteristics of the present study population were described using descriptive statistics. Continuous variables were described using mean and standard deviation, and compared using Mann-Whitney U test. Categorical data was described using frequencies and compared using Chi-square test. Fisher’s exact test was used when value of any cell was less than five. Analysis was carried out at 5% level of significance and p-value <0.05 (two-sided) was considered statistically significant.
Results
A total of 474 patients were included in the present study, out of which 409 (86%) were males and 65 (14%) were females. Their median age was 32 years (range: 2-87 years). The mean follow of these patients was 6.79 weeks.
Group 1 and 2 were comparable in terms of age and sex distributions [Table/Fig-1].
Baseline characteristics of the study groups.
| Group 1 (Buried K-wires) | Group 2 (unburied K-wires) | p-value |
|---|
| Number of patients (%) | 141 (30) | 333 (70) | |
| Age (median, range) in years | 34 (8-87) | 32 (2-78) | 0.425 |
| Number of males (%) | 120 (85) | 289 (87) | 0.627 |
| Site of fracture | Upper limb | 100 (71) | 184 (55) | 0.001* |
| Lower limb | 41 (29) | 149 (45) |
| Type of fracture | Closed | 115 (82) | 239 (72) | 0.025* |
| Open | 26 (18) | 94 (28) |
| Centre at which surgery was performed | Centre 1 | 139 (99) | 92 (28) | <0.001* |
| Centre 2 | 2 (1) | 241 (72) |
Values are summarised as numbers (percentages), unless indicated otherwise. *p<0.05†χ2 test was used for categorical variables and Mann-Whitney U test for continuous variables (data was non-normally distributed).
Group 1 had a greater proportion of upper limb surgeries and closed fractures compared to Group 2 and the difference was statistically significant. Also, majority of the surgeries in Group 1 was done in centre 1 and most of that of Group 2 in centre 2.
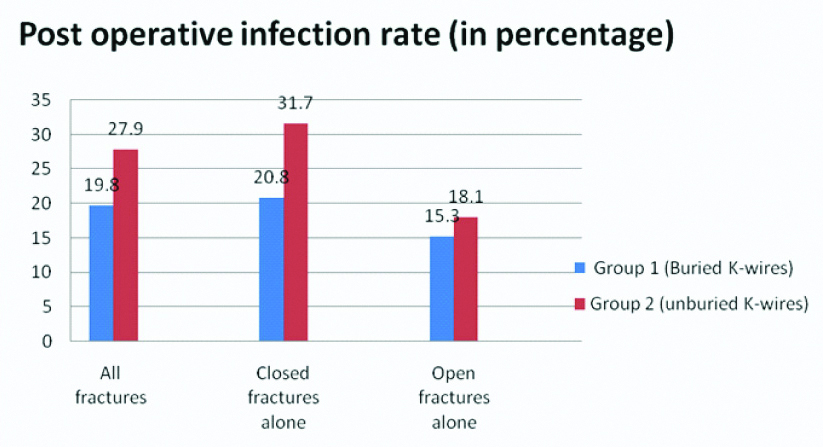
The overall infection rate in the present study was 25.5%. Post operative pin site infection rates were lower in Group 1 (19.8%) compared to group 2 (27.9%). However, the difference was not statistically significant. When closed fractures alone were considered, post operative infection rates were significantly lower in Group 1 compared to Group 2 (p=0.032). Among open fractures, post operative pin site infection rates were not significantly different between the two groups [Table/Fig-2].
Post operative infection rates in Group-1 and 2.
| Group-1 (Buried K-wires) | Group-2 (unburied K-wires) | p-value |
|---|
| All fractures | 28 (19.8) | 93 (27.9) | 0.065 |
| Closed fractures alone | 24 (20.8) | 76 (31.7) | 0.032* |
| Open fractures alone | 4 (15.3) | 17 (18.1) | 1.000 |
Values are summarised as numbers (percentages), unless indicated otherwise. *p<0.05. χ2 test was used to determine statistical significance. Fisher’s exact test used when value of any cell was <5.
Open and closed fractures are not comparable in terms of post operative infection rates because of the contamination in open fractures [Table/Fig-3]. Further, open and closed fractures were not equally distributed in the two groups (buried and un buried K-wires). More closed fractures were fixed with buried K-wires while more open fractures were fixed with unburied. This formed a significant source of bias in the present study. To overcome this, analysis was done separately for open and closed fractures. Among open fractures, there was no advantage noted due to buried K-wires, because the fracture site is already contaminated.
Bar chart for post operative infection rate in buried and unburied K-wires.
Discussion
The basis for using buried K-wires was based on the presumption of reduced pin site infection rates. The concept of burying K-wires under the skin after fracture fixation versus keeping it unburied has been a topic of debate and still studies are underway to come to a consensus regarding this matter. However, till now there have been conflicting conclusions in different studies.
In our retrospective study, of the 474 patients, 25% of the total patients had pin site infections. The pin site infection rate was lower in buried K-wires (20%) compared to unburied K-wires (28%). However, the difference was not statistically significant. There are several prior studies which reported no significant differences in infection between buried and unburied K-wires on statistical analysis, but the raw data in all these studies demonstrated lower infection rate in the buried K-wire technique [14-16].
At the same time, there are many studies which have proved that buried K-wires have statistically significant lower infection rate than unburied K-wires [11-13]. In a similar retrospective study by Ridley TJ et al., in 695 patients over nine years 16.4% unburied K-wires and 9.2% buried K-wires were infected [18]. Rafique A et al., demonstrated a similar rate of infection in his study, 18% in unburied K-wires and 4.4% in buried K-wires [11]. Launay F et al., reported higher rate of infection in unburied K-wires (28%) and only 8% infection in buried K-wires [19].
While the above studies supported buried K-wire technique, there are other studies which reported that there is no difference between buried and unburied K-wire fixations [16,20,21]. Lethaby A et al., performed a Cochrane database analysis and demonstrated that there is no advantage of one technique over the other [22]. Das DS et al., conducted a retrospective cohort study of all lateral condyle fractures treated over a 10 year period at a single institution, and found no significant difference in the rate of infection, using buried and unburied wires [23].
Our retrospective study, demonstrated a statistically significant lower incidence of infection in buried K-wires compared to unburied K-wires in subgroup analysis of closed fractures. The present study is consistent with a prospective randomised study by Hargreaves DG et al., in distal radius fractures. He studied 29 patients with buried K-wires and 27 patients with unburied K-wires, had only one open fracture in each group and reported 34% infection with buried K-wires and 7% with unburied K-wires [13].
The present study is in contrast with few other studies which have compared buried versus unburied K-wire fixations in closed fractures. A study done by Ormsby NM et al., in 124 patients demonstrated no significant difference in incidence of infection with buried and unburied K-wires in closed lateral condyle fractures [20]. Another study by McGonagle L et al., in 67 patients with closed lateral condyle fractures also concluded there is no advantage of burying K-wires over unburied K-wires [24]. A recent meta analysis done by Quin YF et al., also concluded that unburied K-wire fixation of lateral condyle distal humeral fracture in children does not increase the total infection rate or superficial infection rate but use of unburied K-wires is more economical and cost effective [10].
Contrary to expectations, the infection rate was lower in open fractures compared to closed fractures in both the groups. However, as the number of open fractures were few, this may not be reflective of the true infection rate.
Limitation
The type of fracture (open versus closed), site of fracture (upper limb versus lower limb) and the centre at which surgery was done was significantly different in both groups. These are factors which affect post operative infection rates and were potential sources of bias in the present study.
Since, it was a retrospective study, our evaluation of the patients was limited to data available in the medical records. Erythema around the pin sites could be due to skin irritation and we also could not confirm infection as bacterial culture was performed only in few cases.
Conclusion
The present study shows significant lower post operative infection in buried K-wire fixations compared to un buried K-wire fixations in closed fractures . Hence, buried K-wire technique is recommended for fracture fixation in closed fractures.
Values are summarised as numbers (percentages), unless indicated otherwise. *p<0.05†χ2 test was used for categorical variables and Mann-Whitney U test for continuous variables (data was non-normally distributed).
Values are summarised as numbers (percentages), unless indicated otherwise. *p<0.05. χ2 test was used to determine statistical significance. Fisher’s exact test used when value of any cell was <5.