Cardiac arrest is a devastating event, which has extensive negative impact on the health care system. CPR a lifesaving procedure is required to bring back the heart function at the time of cardiac arrest. It can occur both inside the hospital and out of the hospital due to many medical emergencies. The rate of in hospital cardiac arrests is almost 100-fold greater than out-of-hospital arrests among paediatric population [1]. After analysing the global statistical data on cardiac arrest among children in PubMed search there is obvious geographical imbalance suggesting all published research is from North America, Western Europe and few countries of the Asia pacific like China [1,2]. In India the outcome of cardiac arrest is poor due to inadequate pre-medical Emergency Medical System (EMS), shortage of EMS protocols, scarcity of medical resources, equipment and infrastructure, inadequate emergency medical personnel training, paucity of awareness and competence of CPR among bystanders and in the community as compared to western countries, where EMS systems are an essential part of the health care facility which commonly adminsters CPR to every victim of cardiac arrest. Data on the precipitating events, survival and predictors of adverse outcome of cardiac arrest in our patient population will help policy makers and health care facilitator, identify the changes to be made to optimise health care system interventions and improve in hospital cardiac arrest outcome. Although, in-hospital cardiac arrest it is somewhat common, but there is inadequate data highlighted on this issue in developing country like India that to prospective study in a tertiary hospital of southern India. Hence, an attempt has been made to study prevalence and survival of paediatric cardiopulmonary arrest which can be used to create a guidelines for setting up EMS, preparing emergency protocols, imparting technical assistant and training in our population in future.
Materials and Methods
A prospective descriptive study was conducted in the Paediatric Emergency, PICU and general wards of Paediatric Department of JIPMER, a tertiary care teaching institute Puducherry, India from October 2012 to June 2014 (one year and nine months). The reported survival after cardiac arrest in the literature varies from 9-47% [2]. Considering an expected survival rate of 20% in our study population with a 5% margin of error with an alpha error of 5% and 90% power, the estimated sample size comes to 135. All children from day one to 12 years of age developed in-hospital cardiac arrest in paediatric general ward, Emergency and PICU were included in the study. Children developed cardiac arrest within six hours of admission in paediatric emergency care, preterm neonates, children with terminal illness receiving compassionate care, children in whom CPR is not initiated or children with brain death.
Data Collection
Patients with in hospital cardiac arrest in ward, emergency and in PICU satisfying inclusion criteria were enrolled in the study after getting informed consent from parents or legal guardian. Cardiac arrest was defined according to American Heart Association (AHA) 2004 protocol [3]. Only initial cardiac arrest satisfying the inclusion criteria was taken for the study, subsequent arrest was not included in the study. CPR was provided according to Paediatrics Advance Life Support (PALS) 2010 AHA guideline [4].
Baseline characteristics such as age, sex, weight, height were recorded. Aetiology, initial admission clinical parameters such as pulse rate, respiratory rate, Blood Pressure, SpO2, Random Blood Sugar (RBS), Capillary Refilling Time (CRT), rhythm, intubation at admission, Venous Blood Gas analysis (VBG), haemoglobin levels, Total Leucocyte Count (TLC), differential count and platelet counts were recorded. Clinical and biochemical parameters (VBG) recorded in the case record within a period of one hour before arrest were also recorded as pre-arrest variables. Similarly, on admission Liver Function Test (LFT), Renal Function Test (RFT) and serum electrolytes were also collected.
Cardiac arrest characteristics such as location of arrest (PICU, Emergency Department and General ward), first documented rhythm during arrest, whether arrest is witnessed or not, ROSC, CPR duration, adrenaline (dosing and frequency), other medications used during resuscitation (sodium bicarbonate, calcium and atropine) and their dosing and frequency were recorded in the performa.
Post-resuscitation phase haemodynamic parameters were monitored from zero to 24 hours. Temperature, BP, pulse rate, rhythm, CRT, SpO2, Glasgow Coma Scale (GCS), pupillary reaction was recorded at ROSC, 12 hours and 24 hours post-resuscitation. RBS was taken at arrest, two hours and six hours of post-resuscitation. For patients who had ROSC, LFT, RFT, serum electrolytes, haemoglobin levels, TLC, differential count and platelet counts were also collected. Time intervals such as PICU stay, ventilation days and duration of hospital stay were also recorded. Final outcome of the patients as survival or death was also recorded. For the survivors PCPC measure of cognitive function was recorded. Normal (PCPC score 1) and mild disability (PCPC score 2) at hospital discharge was defined as good neurological function [5].
Statistical Analysis
The data obtained from the study was analysed using SPSS 20.0 (IBM Corporation, New York, and U.S.A) software. The various clinical and lab parameters recorded were summarised using mean/median (continuous data) and proportions (binary data). The data of survivors were compared with non-survivors to identify significant association with the primary outcome (survival/death). Continuous variables with normal distribution were compared using student t-test and those not normally distributed using Mann-Whitney U test. Chi-square test or Fisher’s test was used for analysing categorical variables. A multivariate logistic regression analysis has done to predict the independent variables that effecting the final outcome (survival or death) among patients with in hospital cardiac arrest. Three models were created for pre-arrest, arrest and post-arrest variables. All statistics were two-tailed, and a p<0.05 was considered to be significant.
Results
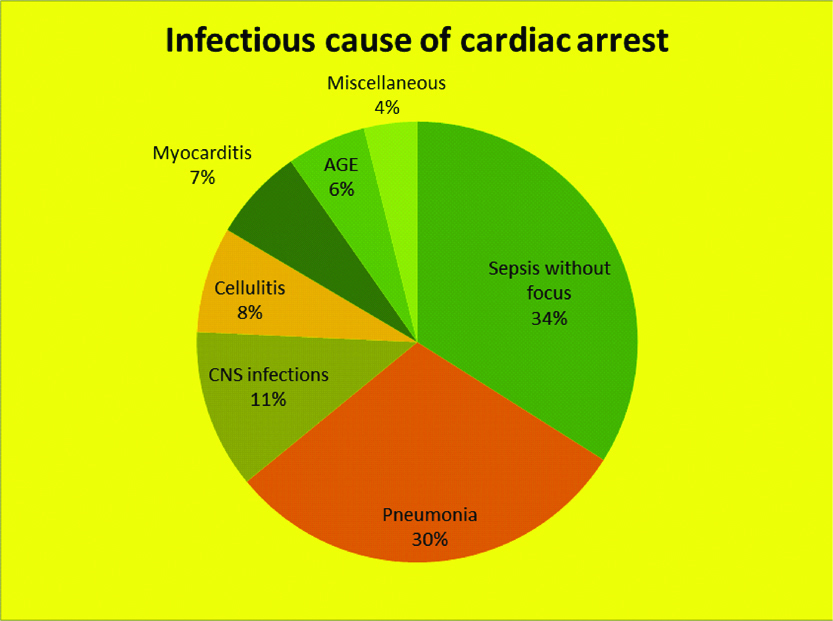
During the study period there were 5049 admissions to the Paediatric Department. Out of this there were only 382 (7.5%). reported cardiac arrests. Totally 137 patients satisfying the inclusion criteria were included in the study [Table/Fig-1]. Most common involved population 77 (56.2%) were infants (less than one year) [Table/Fig-1]. Total patients who had in-hospital cardiac arrest, 80 (58.4%) were males and 57 (41.6%) were females [Table/Fig-1]. Among survivors, majority were in the age group between one month to six months and survival rate was higher among males (14.6%). Infections contributed to 103 cases (75.18%) of the underlying aetiology in children having cardiac arrest [Table/Fig-1]. Most common infection identified was sepsis without focus (33.9%), followed by pneumonia (30%) [Table/Fig-2]. The most common site of occurrence of cardiac arrest was in PICU in 126 (91.97%) patients [Table/Fig-3]. Due to the high preponderance of PICU arrest, 88.3% of the study children were receiving mechanical ventilation at the time of cardiac arrest. Out of 137 children who had cardiac arrest in our study, ROSC was achieved only in 82 children (59.8%) [Table/Fig-3] and out of these 61 (74.3%) children were alive after 12 hours of post-resuscitation, 56 (68.29%) were alive at 24 hours of post-arrest period. Only 27 children (19.7%) out of 137 children who had cardiac arrest, survived to hospital discharge. Median duration of CPR was 20 minutes and median number of adrenaline doses was three [Table/Fig-3]. Children with low BP and prolonged CRT, VBG disturbances like metabolic and respiratory acidosis with hypoxia one hour before the occurrence of cardiac arrest had poor outcome [Table/Fig-4]. At the time of arrest, need of prolonged CPR, use of multiple doses of adrenaline were also predictors of poor outcome [Table/Fig-3]. Most common observed rhythm at the time of cardiac arrest was bradycardia in 100 (72.9%) cases followed by asystole in 26 (19%), shockable rhythms (VT/VF) eight (5.8%) and Pulseless Electrical Activity (PEA) in three (2.1%) cases [Table/Fig-3]. In the post-arrest period, presence of low BP, prolonged CRT, low SpO2 and hypothermia at 12 hours and 24 hours post-cardiac arrest were independently associated with poor outcome [Table/Fig-5]. In addition, lab parameters like low platelet count, deranged Prothrombin Time/International Normalised Ratio (PT/INR) and liver dysfunction in the post-resuscitation phase were associated with poor outcome [Table/Fig-6]. In our study, 21 (77.8%) of the survivors had normal to mild disability at discharge and only one patient (3.7%) had severe disability at discharge [Table/Fig-7]. Results of logistic regression models during pre-arrest, arrest, post-arrest are shown in [Table/Fig-8]. They were used to determine the independent predictors for outcome among the pre-arrest, arrest and post-arrest clinical parameters respectively. During pre-arrest, variables such as prolonged CRT, respiratory acidosis and liver dysfunction were associated with mortality. During arrest, resuscitation parameter like requirement of large number of adrenaline doses were associated with poor survival. During post-arrest vitals like CRT, BP, SpO2, Temperature and pulse rate were found to influence the survival [Table/Fig-8].
Demographic characteristics, aetiology of underlying illness resulting in cardiac arrest of study population and relation to outcome.
| Characteristics | Survivors (n=27) | Non-survivors (n=110) | Total | p-value |
|---|
| Age |
| 1 to 28 days | 3 (18.8%) | 13 (81.2) | 16 (100%) | |
| 1 to < months | 12 (29.3%) | 29 (70.7%) | 41 (100%) | |
| 6 months to <1 year | 3 (15%) | 17 (85%) | 20 (100%) | |
| 1 to <3 years | 1 (4.3%) | 22 (95.7%) | 23 (100%) | 0.231 |
| 3 to <6 years | 4 (28.6%) | 10 (71.4%) | 14 (100%) | |
| 6 to 12 years | 4 (17.4%) | 19 (82.6%) | 23 (100%) | |
| Sex |
| Male | 20 (25%) | 60 (75%) | 80 (100%) | |
| Female | 7 (12.3%) | 50 (87.7%) | 57 (100%) | 0.0316 |
| Aetiology |
| Infections | 19 (18.5%) | 84 (81.5%) | 103 (100%) | 0.197 |
| Heart disease | 3 (27.3%) | 8 (72.7%) | 11 (100%) | 0.453 |
| Fulminant hepatic failure | 1 (14.3%) | 6 (85.7%) | 7 (100%) | 0.583 |
| Envenomation | 2 (33.3%) | 4 (66.7%) | 6 (100%) | 0.337 |
| Status epilepticus | 1 (20%) | 4 (80%) | 5 (100%) | 1.00 |
| Haematological malignancies | 1 (33.3%) | 2 (66.7%) | 3 (100%) | 0.485 |
| Diabetic Ketoacidosis (DKA) | 0 (0.0) | 2 (100%) | 2 (100%) | 0.644 |
Case distribution of children with infectious aetiology.
CNS: Central nervous system
In-hospital arrest event parameters, CPR duration, medications used during resuscitation and their relation to outcome.
| Characteristics | Survivors (n=27) n (%) | Non-survivors (n=110) n (%) | p-value |
|---|
| Location of arrest |
| PICU (n=126) | 23 (85.2) | 103 (93.6) | 0.161 |
| General Ward (n=6) | 3 (11.1) | 3 (2.7) |
| Emergency (n=5) | 1 (3.7) | 4 (3.6) |
| Rhythm at arrest |
| Bradycardia (n=100) | 21 (77.8) | 79 (71.8) | 0.161 |
| Asystole (n=26) | 4 (14.8) | 22 (20.0) |
| VT/VF (n=8) | 1 (3.7) | 7 (6.4) |
| PEA (n=3) | 1 (3.7) | 2 (1.8) |
| ROSC | |
| Yes (n=82) | 27 (100.0) | 55 (50.0) | 0.0001 |
| No (n=55) | 0 (0.0) | 55 (50.0) | |
| CPR duration |
| 0 to 5 minutes (n=39) | 15 (55.6) | 24 (21.8) | 0.0001 |
| 5 to 10 minutes (n=10) | 3 (11.1) | 7 (6.4) |
| 10 to 15 minutes (n=14) | 5 (18.5) | 9 (8.2) |
| 15 to 20 minutes (n=15) | 2 (7.4) | 13 (11.8) |
| 20 to 30 minutes (n=40) | 2 (7.4) | 38 (34.5) |
| 30 to 45 minutes (n=16) | 0 (0.0) | 16 (14.5) |
| More than 45 minutes (n=3) | 0 (0.0) | 3 (2.7) |
| 1. Adrenaline |
| 1 Dose (n=28) | 12 (44.4) | 16 (14.5) | 0.003 |
| 2 Doses (n=30) | 6 (22.2) | 24 (21.8) |
| 3 Doses (n=79) | 9 (33.3) | 70 (63.6) |
| 2. Calcium | |
| 1 Dose (n=36) | 3 (11.1) | 23 (20.9) | 0.210 |
| 2 Doses (n=21) | 2 (7.4) | 19 (17.3) |
| 3 Doses (n=2) | 0 (0.0) | 2 (1.8) |
| No Calcium (n=82) | 22 (16.1) | 66 (60.0) |
| 3. NaHCO3/ATROPINE |
| NaHCO3 (n=19) | 1 (3.7) | 18 (16.4) | 0.120 |
| Atropine (n=13) | 4 (14.8) | 9 (8.2) |
| NaHCO3 and Atropine (n=4) | 2 (7.4) | 2 (1.8) |
| NO NaHCO3/Atropine (n=101) | 20 (74.1) | 81 (73.6) |
CPR: CardioPulmonary Resuscitation, PICU: Paediatric intensive care unit, VT: Ventricular tachycardia, VF: Ventricular fibrillation, PEA: Pulseless electrical activity, ROSC: Return of spontaneous circulation, NaHCO3: Sodium bicarbonate, NO: Nitric oxide
Pre-arrest clinical, haemodynamic characteristics and blood gas parameters relation with outcome*.
| Characteristics | Survivors (n=27) n(%) | Non-survivors (n=110) n(%) | p-value |
|---|
| Pulse rate |
| Normal | 11 (40.7) | 30 (27.3) | 0.561 |
| Tachycardia | 8 (29.6) | 40 (36.4) |
| Bradycardia | 8 (29.6) | 40 (36.4) |
| SpO2 |
| ≤94 | 16 (59.3) | 73 (66.4) | 0.506 |
| 95 to 100 | 11 (40.7) | 37 (33.6) |
| Blood pressure |
| Normal | 16 (59.3) | 23 (20.9) | 0.001 |
| Hypotension | 10 (37.0) | 86 (78.2) |
| Hypertension | 1 (3.7) | 1 (0.9) |
| CRT |
| Normal | 11 (40.7) | 10 (9.1) | 0.001 |
| Prolonged | 16 (59.3) | 100 (90.9) |
| Rhythm |
| Normal | 26 (96.3) | 107 (97.3) | 0.001 |
| Abnormal | 1 (3.7) | 3 (2.7) |
| Bicarbonate |
| 22 to 29 | 7 (25.9) | 7 (6.4) | 0.006 |
| 15 to <22 | 7 (25.9) | 21 (15.3) |
| Less than 15 | 11 (40.7) | 78 (70.9) |
| More than 29 | 2 (7.4) | 4 (3.6) |
| Base excess |
| Less than -5 | 7 (25.9) | 7 (6.4) | 0.001 |
| -5 to -10 | 7 (25.9) | 17 (15.5) |
| -11 to -15 | 8 (29.6) | 18 (16.4) |
| More than -15 | 5 (18.5) | 64 (58.2) |
| Positive base excess | 0 (0.0) | 4 (3.6) |
| PCO2 |
| 35 TO 45 | 11 (40.7) | 22 (20.0) | 0.001 |
| Less than 35 | 10 (37.0) | 18 (16.4) |
| More than 45 | 6 (22.2) | 70 (63.6) |
| pH before arrest** |
| 7.35 to 7.45 | 12 (44.4) | 15 (13.6) | 0.0001 |
| 7.25 to 7.34 | 11 (40.7) | 8 (8.2) |
| 7.11 to 7.24 | 2 (7.4) | 19 (17.3) |
| 7.0 to 7.10 | 0 (0.0) | 22 (20) |
| Less than 7 | 0 (0.0) | 43 (39.1) |
| More than 7.45 | 0 (0.0) | 2 (1.8) |
*Pre-arrest variables are those recorded within one hour prior to cardiac arrest
**In two survivor cases, report of VBG could not obtained. We have analysed the data with 25 cases only. In one case of non-survivors group we have analysed the data with 109 VBG value, as patient report was not obtained.
CRT: Capillary refilling time, VBG: Venous blood gas
Haemodynamic parameters, vital parameters during post-cardiac arrest (0 to 24 hours) compared with outcome.*
| Characteristics | Survivors n(%) | Non-survivors n(%) | p-value |
|---|
| Blood Pressure |
| 12 hours of post-arrest |
| Normal | 27 (100.0) | 18 (52.9) | 0.001 |
| Hypotension | 0 (0.0) | 14 (41.2) |
| Hypertension | 0 (0.0) | 2 (5.9) |
| Blood Pressure |
| 24 hours of post-arrest | 27 (100.) | 23 (79.3) | 0.001 |
| Normal | 0 (0.0) | 5 (17.2) |
| Hypotension | 0 (0.0) | 1 (3.5) |
| Hypertension | | | |
| Pulse Rate |
| 12 hours of post-arrest |
| Normal | 17 (62.9) | 22 (64.7) | 0.001 |
| Tachycardia | 10 (37.1) | 11 (32.3) |
| Bradycardia | 0 (0.0) | 1 (3.0) |
| Pulse Rate |
| 24 hours of post-arrest |
| Normal | 17 (62.9) | 23 (79.3) | 0.001 |
| Tachycardia | 10 (37.1) | 6 (20.7) |
| Bradycardia | 0 (0.0) | 0 (0.0) |
| SpO2 |
| 12 hours of post-arrest |
| Less than 94% | 2 (7.5) | 11 (32.3) | 0.001 |
| 95 to 100% | 25 (92.5) | 23 (67.4) |
| SpO2 |
| 24 hours of post-arrest |
| Less than 94% | 2 (7.5) | 21 (72.4) | 0.001 |
| 95 to 100% | 25 (92.2) | 8 (27.3) |
| CRT |
| 12 hours of post-arrest |
| Normal | 26 (96.3) | 15 (44.2) | 0.001 |
| Prolonged | 1 (3.7) | 19 (55.8) |
| CRT |
| 24 hours of post-arrest |
| Normal | 27 (100.0) | 21 (72.4) | 0.001 |
| Prolonged | 0 (0.0) | 8 (27.3) |
| Temperature |
| 12 hours of post-arrest |
| Normal | 27 (100.0) | 29 (85.3) | 0.001 |
| Hypothermia | 0 (0.0) | 5 (14.7) |
| Temperature |
| 12 hours of post-arrest |
| Normal | 27 (100.0) | 29 (85.3) | 0.001 |
| Hypothermia | 0 (0.0) | 5 (14.7) |
CRT: Capillary refilling time
Organ dysfunction after arrest and relationship to mortality in patients with ROSC*.
| Characteristics | Survivors (n=27) n (%) | Non-survivors (n=55) n (%) | p-value |
|---|
| GCS |
| At 12 hours of post-arrest |
| GCS<5 | 11 (40.7) | 28 (82.4) | 0.0001 |
| GCS≥5 | 16 (59.3) | 6 (17.6) |
| GCS |
| At 24 hours of post-arrest |
| GCS<5 | 6 (22.2) | 20 (68.9) | 0.0001 |
| GCS≥5 | 21 (77.8) | 9 (31.1) |
| Pupil |
| At 12 hours of post-arrest |
| PERL | 26 (96.3) | 28 (82.4) | 0.0001 |
| Not Reacting | 1 (3.7) | 6 (17.6) |
| Pupil |
| At 24 hours of post-arrest |
| PERL | 27 (100.0) | 27 (93.1) | 0.0001 |
| Not Reacting | 0 (0.0) | 2 (6.9) |
| LFT |
| Normal | 27 (100) | 45 (81.8) | 0.0001 |
| Deranged | 0 (0.0) | 10 (18.2) |
| PT/INR |
| Normal | 26 (96.3) | 41 (74.5) | 0.0001 |
| Deranged | 1 (3.7) | 14 (25.5) |
| Albumin |
| Normal | 21 (77.8) | 39 (70.9) | 0.0001 |
| Low | 6 (22.2) | 16 (29.1) |
| Platelet |
| Normal | 21 (77.8) | 21 (38.2) | 0.0001 |
| Thrombocytopenia | 6 (22.2) | 34 (61.8) |
*Totally 82 patients had ROSC after arrest, 55 died during arrest. Post-arrest LFT, RFT, PT/INR, Platelet count and hemoglobin analysis was done for patients who had ROSC.
ROSC: Restoration of spontaneous circulation, GCS: Glasgow coma scale, LFT: Liver function test, RFT: Renal function test, PT/INR: Prothrombin time/International normalised ratio
Paediatric cerebral performance category (PCPC) scale at discharge.
| PCPC score | Survivors (n=27) n(%) |
|---|
| Normal (score=1) | 12 (44.5) |
| Mild disability (score=2) | 9 (33.3) |
| Moderate disability (score=3) | 5 (18.5) |
| Severe disability (score=4) | 1 (3.7) |
| Coma/vegetative state (score=5) | 0 |
| Brain Death (score=6) | 0 |
Model-multivariate regression analysis for pre-arrest, arrest, post-arrest variables independently associated with mortality (R2=0.494).
| Variable | Odds ratio | 95% CI | p-value |
|---|
| Low BP pre-arrest | 12.11 | 10.35-13.87 | 0.001 |
| Prolonged CRT pre-arrest | 16.73 | 14.03-19.43 | 0.0001 |
| Prolonged CPR duration | 20.42 | 19.70-21.14 | 0.0001 |
| Failure of ROSC | 22.56 | 21.36-23.76 | 0.0001 |
| More doses of Adrenaline | 12.94 | 10.34-15.54 | 0.002 |
| Low pH pre-arrest | 40.08 | 39.59-40.57 | 0.0001 |
| High PaCO2 pre-arrest | 12.01 | 10.29-13.73 | 0.001 |
| Low PaO2 pre-arrest | 6.55 | 5.57-7.53 | 0.011 |
| Low HCO3 pre-arrest | 7.37 | 5.80-8.92 | 0.007 |
| High base excess at pre-arrest | 19.24 | 17.92-20.56 | 0.001 |
| Low BP 12 hour post-arrest | 21.23 | 20.39-22.07 | 0.0001 |
| Low BP 24 hour post-arrest | 14.30 | 12.86-15.74 | 0.003 |
| Prolonged CRT 12 hours post-arrest | 22.79 | 22.11-23.47 | 0.0001 |
| Prolonged CRT 24 hours post-arrest | 18.28 | 17.18-19.38 | 0.0001 |
| Low SpO2 12 hours post-arrest | 10.27 | 7.53-13.01 | 0.016 |
| Low SpO2 24 hours post-arrest | 11.88 | 9.94-13.82 | 0.003 |
| Hypothermia 12 hours post-arrest | 7.64 | 3.54-11.74 | 0.022 |
| Hypothermia 24 hours post-arrest | 8.65 | 5.53-11.77 | 0.013 |
| Prolonged PT/INR post-arrest | 5.03 | 1.43-8.63 | 0.025 |
| Liver dysfunction post-arrest | 4.83 | 1.27-8.39 | 0.028 |
| Low platelet post-arrest | 8.80 | 6.72-10.88 | 0.003 |
| Tachycardia 24 hour post-arrest | 9.31 | 6.97-11.65 | 0.01 |
BP: Blood pressure, CRT: Capillary refilling time, CPR: Cardiopulmonary resuscitation, ROSC: Return of spontaneous circulation, HCO3: Bicarbonate, PT/INR: Prothrombin time/International normalised ratio
Discussion
According to our study, the prevalence of cardiac arrest among the total admissions during the study period was 7.5 %. The study by Zeng J et al., the prevalence of cardiopulmonary arrest among hospitalised patients was observed to be 0.18% [1].
In our study, more than half of the patients (56.2%) and series by Meert KL et al., 66.2% were infants [2]. This observation is similar to the meta-analysis done by Young KD and Seidel JS where younger age group with respiratory cause contributed to higher percentage of cardiac arrest [6]. This high proportion of infants in various paediatric series on cardiac arrest may be attributable to the high prevalence of infections, especially respiratory infection in this age group and their tendency to decompensate rapidly.
The most common causes of in-hospital cardiac arrests are respiratory failure (asphyxia) and circulatory shock by Meaney PA et al., [7]. As per Meert KL et al., respiratory diseases were more likely to cause arrest among survivors arrest [2]. According to our study, infections were the underlying aetiology that contributed to 75% of the study children. Most common infection identified was sepsis without focus (33.9%), followed by pneumonia (30%). These observed differences in underlying aetiology may be a reflection of the local epidemiology and the setting in which the studies were carried out.
Overall, 92% of the observed cardiac arrest occurred in PICU. Due to the high preponderance of PICU arrest, 88.3% of the study children were receiving mechanical ventilation at the time of cardiac arrest. A study based in China suggested arrest in PICU contributes 81% [1]. This may be a due to the fact that seriously ill patients were transferred to PICU before the occurrence of significant deterioration of their vital parameters.
As per our study, ROSC was achieved only in 82 children (59.8%) and 27 children (19.7%) survived to hospital discharge. Reis AG et al., who studied 129 children had ROSC of 64%, with a survival rate of 16% [8]. According to De Mos N et al., of 91 children who had cardiac arrest, ROSC attained in 75 (82%) children, 23 (25%) to hospital discharge [9]. Nadkarni VM et al., showed ROSC of 52% with 27% survival along with good neurological outcome in 18% of about 880 patients studied [10].
We also compared the various clinical parameters and other characteristics of survivors and non-survivors to identify important predictors of outcome. Among the variables recorded at the time of hospital admission, presence of prolonged CRT, metabolic acidosis, respiratory acidosis and haematological disturbances like deranged PT/INR, low platelet count and liver dysfunction were independently associated with poor survival. These parameters indicate signs of physiological decompensation irrespective of aetiology and hence, may be general predictors of poor outcome. Factors associated with survival after in hospital cardiac arrest from a European study by Lopez Herce J et al., showed that, duration of CPR more than 10 minutes, occurrence of cardiac arrest in PICU and inotrope infusion before the arrest were associated with poor outcome [11].
In our study, analysis of the resuscitation parameters showed that median duration of CPR was 20 minutes and median number of adrenaline doses was three. We also looked at clinical, laboratory and resuscitation parameters during cardiac arrest and their influence on final outcome. It was observed that children with low BP and prolonged CRT one hour before the occurrence of cardiac arrest had poor outcome [Table/Fig-8]. In addition, need for prolonged CPR (more than 20 minutes), multiple doses of adrenaline (more than three doses), and VBG disturbances like metabolic and respiratory acidosis with hypoxia was also predictors of poor outcome [Table/Fig-8]. Even though use of sodium bicarbonate (13.8%) and calcium gluconate (35.7%) was observed in our study, majority of the children did not receive sodium bicarbonate or calcium gluconate during the arrest. Use of these medications had no influence on the final outcome; however, there was increased frequency of use of calcium during the arrest among non-survivors. Totally 35.7% of our study population received calcium during resuscitation which was lower compared to the study by Srinivasan V et al., where calcium was used in 45% of cardiac arrest victims [12]. Calcium use was associated with higher mortality in their study. In our children, of the 35.7% who received calcium during resuscitation, 32.1% belonged to non-survival group though the difference did not show statistical significance.
Most common observed rhythm during arrest was bradycardia (72.9%) followed by asystole (19%) and shockable rhythms (VT/VF) (5.8%). In their study from U.S.A, Nadkarni VM et al., showed PEA or asystole to be the most common rhythm during arrest [10]. According to NRCPR database arrhythmogenic arrest (VT/VF) contributes 10% of the total rhythm in paediatric cardiac arrest [10]. In our study occurrence of VT/VF was less than that reported by The National Registry CardioPulmonary Resuscitation (NRCPR) database. This difference may be attributable to the difference in the aetiology of underlying illness resulting in cardiac arrest in different settings. In a tertiary care center handling general paediatric patients, with few children having underlying heart disease, the population of patients with shockable rhythms may not be high. In our study, children with underlying heart disease constituted only 8% of the study population. Even though we looked at other parameters such as place of arrest, time of arrest, CPR given by nurse and type of rhythm, these parameters did not influence the final outcome. NRCPR study describes time and day of week as predictors of outcome in adults, but in our study, timing of arrest did not influence the outcome [10].
The post-resuscitation phase after cardiac arrest is a crucial phase where reperfusion injuries can influence the outcome. Out of the 82 children who had return of spontaneous circulation, 61 (74.3%) were alive at 12 hours and 56 (68.29%) were alive at 24 hours. We analysed the serial vital parameters after cardiac arrest to identify the prognostic factors after cardiac arrest in our population. Hypotension in the post-resuscitation phase was associated with poor survival as shown in a study done by Kilgannon JH et al., [13]. De Mos N et al., showed that presence of kidney injury at admission along with epinephrine infusion before arrest was associated with poor outcome [9]. Calcium used at the time of arrest also related to poor survival in their series.
Fever, near normal pH, low lactate levels, two responsive pupils in the first 12 hours following arrest were shown to improve survival by Meert KL et al., [2]. In our study, among the vital parameters analysed, low BP, prolonged CRT, low SpO2 and hypothermia at 12 hours and 24 hours post-cardiac arrest were independently associated with poor outcome [Table/Fig-8]. In addition, low GCS and tachycardia at 24 hours were also predictors of poor outcome. Lab parameters associated with poor survival rates were low platelet count, deranged PT/INR and liver dysfunction [Table/Fig-8]. These identified derangements in vital parameters indicated poor cardiopulmonary function following cardiac arrest. Persistent decompensation of vital parameters in the immediate post-arrest phase indicates poor prognosis in our study. Even though pupillary response and hyperglycaemia following post-arrest phase showed significant association with mortality in univariate analysis, they did not achieve statistical significance in multivariate analysis.
We also looked at neurological status of the survivors by Pediatric cerebral performance score at discharge (PCPC) and found that 77.8% of the survivors had normal to mild disability at discharge. Only one patient (<1%) had severe disability at discharge. The reported frequency of good neurologic outcome from other series ranged from 14% to 76.7% [2,7,14,15]. The relatively good neurological outcome observed in our study may be attributed to the fact that most arrests happened in the PICU where immediate CPR could be initiated. Moreover, the ICU setting ensured good monitoring and supportive management in the post-resuscitation phase in most of these children.
Limitation
We excluded cardiac arrest occurring within six hours of hospital admission due to logistical reasons primarily due to difficulty in collecting data. This could have missed those children having cardiac arrest in the emergency and thus might have resulted in under reporting of cardiac arrests from the emergency. Children from surgical wards were not included in the study. Hence, aetiological profile primarily reflects children with medical problems. Severity of illness scoring was not done at the time of admission to calculate and compare the predicted and observed mortality in children. Follow up of children including mortality at one month and neurological status post discharges were not assessed.
Conclusion
In Paediatric population the prevalence of in-hospital cardiopulmonary arrest is low. Among children with in-hospital cardiac arrest approximately one-fifth cases sustained return of circulation and survived to hospital discharge. Over three fourths had satisfactory neurological outcomes based on PCPC scale measurements in survivors. Many parameters are independently correlated with hospital mortality. Forthcoming research should assess whether each of these correlations constitute as cause and effect. Clinical researcher determining the effectiveness of modern interventions like therapeutic hypothermia in paediatric cardiac arrest is essential to recognise these conclusions in their research methodology.
CPR: CardioPulmonary Resuscitation, PICU: Paediatric intensive care unit, VT: Ventricular tachycardia, VF: Ventricular fibrillation, PEA: Pulseless electrical activity, ROSC: Return of spontaneous circulation, NaHCO3: Sodium bicarbonate, NO: Nitric oxide
*Pre-arrest variables are those recorded within one hour prior to cardiac arrest
**In two survivor cases, report of VBG could not obtained. We have analysed the data with 25 cases only. In one case of non-survivors group we have analysed the data with 109 VBG value, as patient report was not obtained.
CRT: Capillary refilling time, VBG: Venous blood gas
CRT: Capillary refilling time
*Totally 82 patients had ROSC after arrest, 55 died during arrest. Post-arrest LFT, RFT, PT/INR, Platelet count and hemoglobin analysis was done for patients who had ROSC.
ROSC: Restoration of spontaneous circulation, GCS: Glasgow coma scale, LFT: Liver function test, RFT: Renal function test, PT/INR: Prothrombin time/International normalised ratio
BP: Blood pressure, CRT: Capillary refilling time, CPR: Cardiopulmonary resuscitation, ROSC: Return of spontaneous circulation, HCO3: Bicarbonate, PT/INR: Prothrombin time/International normalised ratio