Paranasal Sinus Carcinoma Dissimulating as Alveolar Osteitis
Arulmozhi Nandakumar1, K Vijayalakshmi2, Ramya Ramadoss3, A Kannan4
1 Postgraduate Student, Department of Oral Pathology and Microbiology, SRM Dental College, Ramapuram, Chennai, Tamil Nadu, India.
2 Postgraduate Student, Department of Oral Medicine and Radiology, SRM Dental College, Ramapuram, Chennai, Tamil Nadu, India.
3 Reader, Department of Oral Pathology and Microbiology, SRM Dental College, Ramapuram, Chennai, Tamil Nadu, India.
4 Reader, Department of Oral Medicine and Radiology, SRM Dental College, Ramapuram, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Arulmozhi Nandakumar, Postgraduate Student, Department of Oral Pathology and Microbiology, SRM Dental College, Bharathi Salai, Ramapuram, Chennai-600089, Tamil Nadu, India.
E-mail: docarulmozhi@gmail.com
Diagnostic imaging, Malignant neoplasm, Maxillary sinus cancers, Paranasal sinus neoplasm
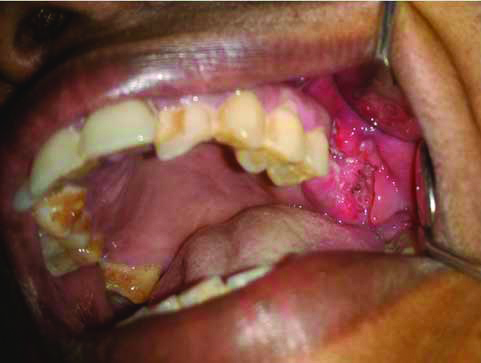
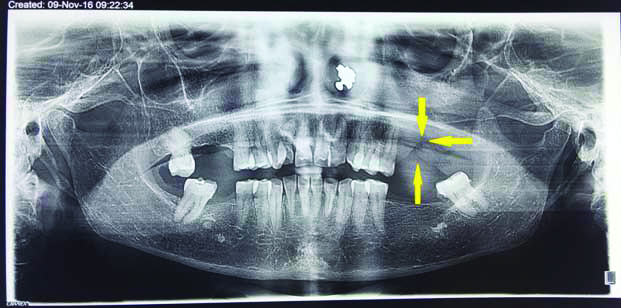
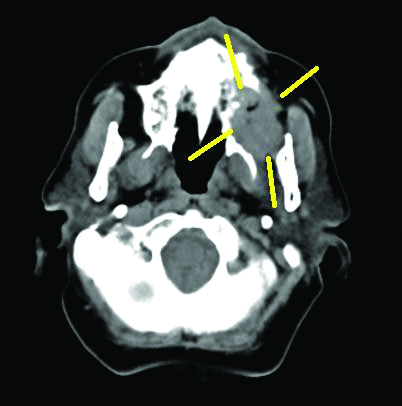
A 58-year-old female patient reported to the Dental Outpatient Department (OPD) for evaluation of persistent pain in the extraction socket of upper left maxillary molar region for past six weeks. The patient gave a history of severe mobility of upper back teeth which was diagnosed as localised chronic periodontitis with Grade III mobility in left upper molar (26,27-FDI system) region for which patient underwent extraction. On intra oral examination, an ulceroproliferative gingival mass measuring 4×3.5 cm dimension was found around the unhealed alveolar socket of 26, 27 and 28 tooth region extending into the buccal vestibule, borders were ill-defined with everted edges and were indurated [Table/Fig-1]. The lesion was tender and exhibited bleeding during examination. A provisional diagnosis of alveolar osteitis was made with differential diagnosis of osteomyelitis and carcinoma of the alveolus and the necessary diagnostic workup was performed. Routine radiographic examination of Orthopantamogram (OPG) revealed radiolucent lesion in relation to 26, 27, 28 tooth region with irregular borders invading maxillary bony trabeculae [Table/Fig-2] but the margins were ill-defined and imaging was non-contributory to diagnosis. In order to visualise the complete extent of the lesion and imaging of the maxillary sinus advanced imaging modalities were employed which lead to a conclusive picture of the lesion. To assess the extent of the maxillary lesion, CT and MRI scan were performed. CT scan of bone window revealed soft tissue mass with irregular borders measuring 3.4×2.5 cm and heterogeneous density in the left posterior maxilla. The lesion had invaded and eroded the left lateral and medial wall of maxillary sinus and left side wall of the nasal cavity [Table/Fig-3].
An ulceroproliferative soft tissue growth in the alveolar socket of 26, 27, 28 tooth region.
An ill-defined radiolucent line with irregular borders adjacent to second premolar region showing bony trabecular erosion evident in the left maxillary posterior region.
CT image reveals soft tissue mass with irregular borders measuring 3.4×2.5 cm.

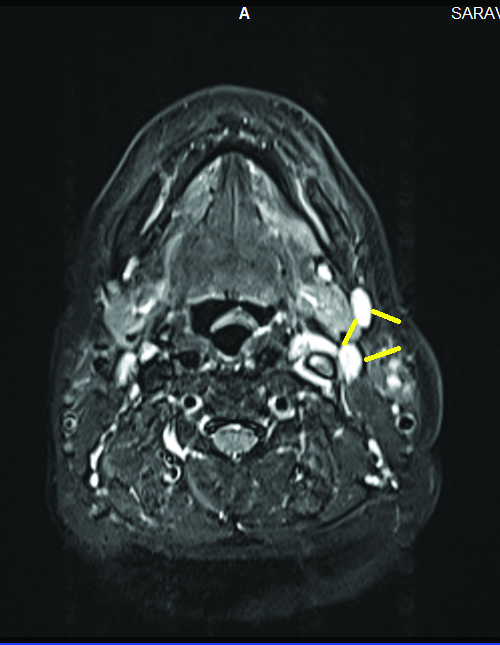
Magnetic Resonance Imaging revealed hypointense signal in T1 weighted image in the left maxillary alveolar process of 26, 27, 28 tooth region and hyper intense signal in T2 weighted image indicating expansion of the tumour till the base of the inferior orbital fissure region [Table/Fig-4,5].
Axial image showing the lesion eroding the left lateral and medial wall of the maxillary sinus and left side of the nasal cavity.
Ipsilateral cervical lymph nodes of 0.6 mm sized level 1B and 0.5 mm sized level 2 evident on the left side of the primary tumour region.
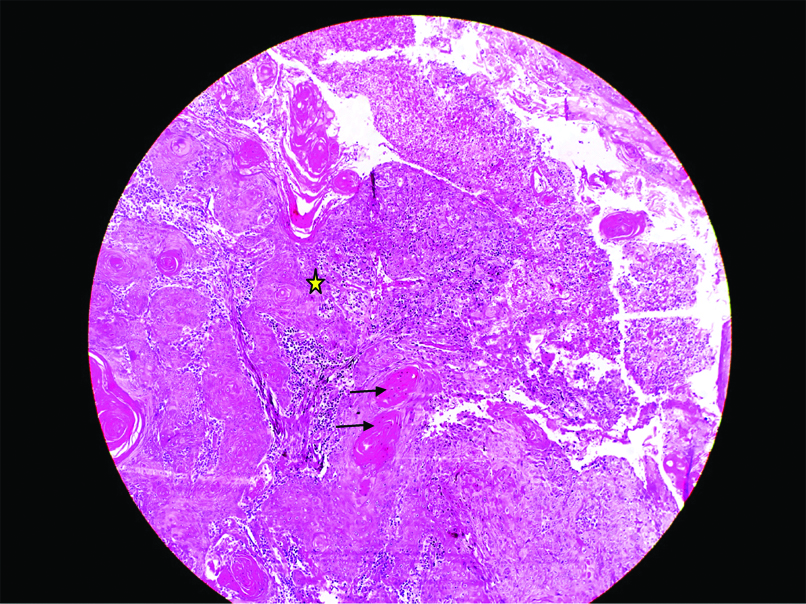
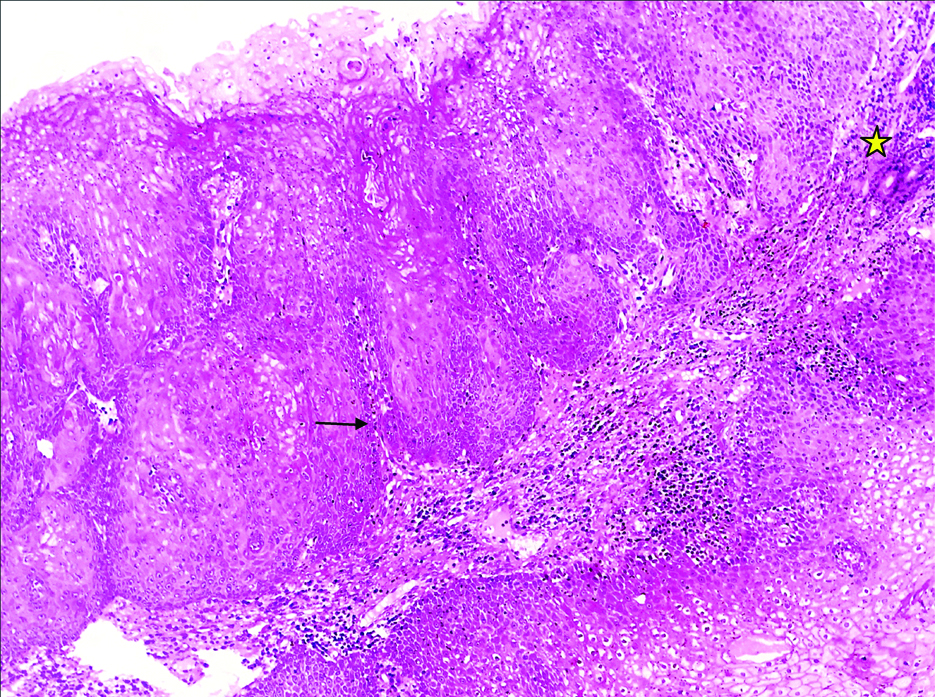
Incisional biopsy under local anaesthesia was done and three soft tissue specimens measuring 1.2×1.5 cm were harvested from the site. The histopathological examination revealed hyperplastic epithelium with varied degree of dysplasia. High degree of keratinisation was found to be exhibited by 50% of the cells. The epithelial cells also showed abundant nuclear pleomorphism with >5 mitotic figures per high power field. Zone of infiltration was well delineated with pushing margins. Stroma exhibited moderate lymphocytic infiltration. Based on Anneroth’s multifactorial grading system the tissue was graded as Grade II Squamous Cell Carcinoma (SCC) [Table/Fig-6,7].
The histopathological examination (4X) revealed hyperplastic epithelium with aberrant keratin pearl formation (->), abundant nuclear pleomorphism with islands of epithelium in the connective tissue (*) and well delineate pushing margins.
The histopathological examination (20X) revealed hyperplastic epithelium with varied degree of dysplasia (->) and zone of infiltration (*).
The earliest symptom presented by the patient was nasal stuffiness and tenderness which can often be misdiagnosed for maxillary sinusitis and lead to late diagnosis of the tumour at a more advance stage. The common clinical presentations include pain (59%), oral symptoms (40%) like mobile tooth or vestibular swelling, maxillary swelling, epistaxis, nasal stuffiness and ocular symptoms like diplopia or proptosis are benign and hence warrant meticulous examination [1,2].
Maxillary sinus neoplasms usually masquerade as periodontal infections, the most common symptoms being pain and mobility in the maxillary molar teeth region. Our patient had presented with Grade III mobility in the maxillary molars and subsequent mild pain during occlusion in the same region which was mistaken for periodontal pain for which she underwent extraction of 26, 27. Though, pulpal and periodontal pathology are the most common etiology for pain in maxillary posteriors, thorough history and radiographic imaging is mandatory to consider non-odontogenic origin prior to extraction of teeth regarded hopeless due to periodontal destruction [2].
The primary objective of radiographic examination is to visualise the malignancy and bone destruction which determines the extent of the carcinoma. In retrospect, it was difficult to diagnose the lesion based on clinical examination prior to treatment. Panoramic radiography an easy accessibility provides the information about the destruction of the boundaries but this imaging modality has its own limitations when it comes to showing evidence of showing early bone destruction and was misleading in this patient’s case [3]. CT and MRI are the choice of examination in such situation. The primary reason for advising CT and MRI study in this case is for better characterising the invasion of structures beyond the site of origin, malignancy and lymph node examination. Aggressive bone destruction is a characteristic feature in patients suffering from SCC. For the present case report, CT bone window findings revealed erosion of medial and lateral wall of the maxillary sinus with nasal cavity extension. MRI is superior in distinguishing tumour from adjacent inflammatory diseases [4]. The incidence of lymph node metastasis is present in 4-20% of all reported cases and if present it has poor diagnosis. In our case report contra lateral neck lymph node was palpable and to check whether there was nodal involvement Apparent Diffusion Coefficient (ADC) values were calculated. ADC value of Level 1B being 1.3 was interpreted as reactive node and Level 2 being 1.6 was suggestive of malignancy in accordance to previous literature [5]. However, micrometastases, if present cannot be diagnosed by the above methods.
[1]. Georgiou AF, Walker DM, Collins AP, Morgan GJ, Shannon JA, Veness MJ, Primary small cell undifferentiated (neuroendocrine) carcinoma of the maxillary sinusOral Sur, Oral Med, Oral Pathol, Oral Radiol, Endodontol 2004 98(5):572-78.10.1016/j.tripleo.2004.04.00315529129 [Google Scholar] [CrossRef] [PubMed]
[2]. Vasudevan V, Kailasam S, Radhika MB, Venkatappa M, Devaiah D, Shrihari TG, Well-differentiated squamous cell carcinoma of maxillary sinusJ Indian Aca Oral Med Radiol 2012 24(3):253-57.10.5005/jp-journals-10011-1307 [Google Scholar] [CrossRef]
[3]. Som PM, Brandwein M, Sinonasal cavities. Tumours and tumour like conditions. In: Som PM, Hugh D, editorsHead and neck imaging 2003 4th ed. StLouisMosby Year Book:262-71. [Google Scholar]
[4]. Tian L, Li YZ, Mo YX, Liu LZ, Xie CM, Liang XX, Nasopharyngeal carcinoma with paranasal sinus invasion: the prognostic significance and the evidence-based study basis of its t-staging category according to the AJCC staging systemBMC Cancer 2014 14:83210.1186/1471-2407-14-83225403714 [Google Scholar] [CrossRef] [PubMed]
[5]. Padhani AR, Liu G, Koh DM, Chenevert TL, Thoeny HC, Takahara T, Diffusion-weighted magnetic resonance imaging as a cancer biomarker: consensus and recommendationsNeoplasia 2009 11(2):102-25.10.1593/neo.8132819186405 [Google Scholar] [CrossRef] [PubMed]