A Persistent Upper Lip Swelling: A Diagnostic Dilemma
Abhishek Soni1, Ashish M Warhekar2, Panjab V Wanjari3
1 Senior Lecturer, Department of Oral Medicine and Radiology, Modern Dental College and Research Center, Indore, Madhya Pradesh, India.
2 Reader, Department of Oral Medicine and Radiology, Modern Dental College and Research Center, Indore, Madhya Pradesh, India.
3 Professor and Head, Department of Oral Medicine and Radiology, Modern Dental College and Research Center, Indore, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Abhishek Soni, 263-Balaji Villa, Shivom Estate, Station Road, Dewas-455001, Madhya Pradesh, India.
E-mail: drabhishek_soni@rediffmail.com
Neoplasms, Mucosa, Tumour
A 62-year-old male patient reported with a complaint of missing teeth and difficulty in eating. Intraoral examination showed completely edentulous maxillary and mandibular arches. Extraoral examination revealed incidental finding of a smooth-surfaced swelling, measuring approximately 3.2×1.4 cm, involving the right side of upper lip [Table/Fig-1]. Detailed history revealed that swelling was present for the past six years and showed spontaneous regression in size approximately within four days and again increased in size over the duration of ten days. The patient denied any pain or altered sensation and could not recount any history of trauma to the area. His past medical history and family history was non-contributory. On palpation, the lesion was fairly well circumscribed, non-tender, freely movable and relatively firm in consistency. No pulsation or blanching on pressure was appreciated. Based on history and clinical examination, a provisional diagnosis of chronic non-specific granulomatous lesion involving the upper lip was made.
Clinical examination of patient: (A) Extraoral examination revealed a non-tender, persistent diffuse swelling of the upper lip; (B) Intraoral view.

Based on clinical presentation various differential diagnoses were considered such as mucoceles, minor salivary gland tumours, Cheilitis Granulomatosa (CG), crohn’s disease, and granulomatous inflammatory diseases. Calibre-persistent labial artery and leiomyoma are included last in the list as the lips being one of the more common sites for both these lesions.
Ultrasonography of the swelling revealed a well-defined cystic lesion with internal echogenic fluid and debris along with the presence of solid component within the cystic space [Table/Fig-2]. Further, Fine Needle Aspiration Cytology (FNAC) was performed which yielded thick, yellow, pus-like fluid, having plenty of cholesterol crystals and few pus cells. Interestingly, the swelling recurred within few minutes after FNAC [Table/Fig-3]. To assess the pathology in detail MRI was advised, which revealed a well-encapsulated, hypointense area with no invasion into surrounding structure [Table/Fig-4].
Ultrasonographic investigation: It revealed a well-defined cystic lesion with internal echogenic fluid and debris. Within the cystic space, presence of solid component is also evident.

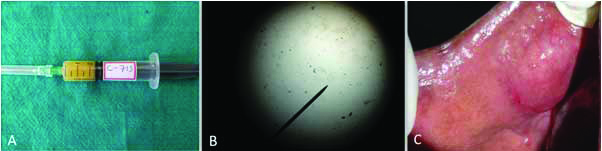
Fine needle aspiration cytology procedure: (A) A thick, yellow, pus-like fluid is aspirated; (B) Plenty of cholesterol crystals and few pus cells are evident within the aspirated fluid; (C) Recurrence of swelling within few min after FNAC.
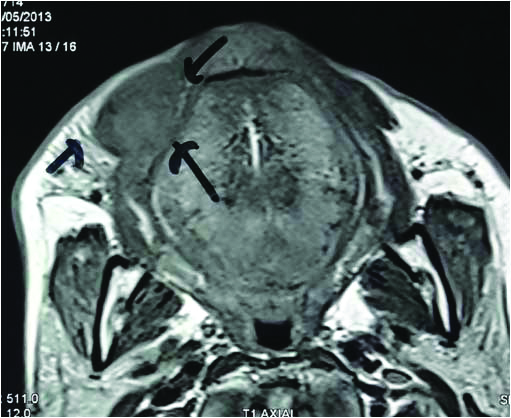
Magnetic Resonance Imaging findings: MRI sections revealed a well-encapsulated, hypointense area with no invasion into surrounding structure.
An excisional biopsy was performed under local anaesthesia, and the excised tissue was submitted for histopathological diagnosis [Table/Fig-5]. Based on histopathological analysis (gross and microscopic), final diagnosis of papillary cystadenoma was made [Table/Fig-6,7]. On follow up evaluation after every three months for one year, no complications or recurrence was noted [Table/Fig-8].
(A) Intraoperative picture depicting the surgical removal of the lesional tissue; (B) Careful resection of the lesional tissue; (C) Excised specimen submitted for histopathological investigation.

On gross histopathological examination, a roughly oval soft tissue specimen, measuring approximately 2.7×1.7×1.3 cm in size. The overlying surface is whitish brown in colour. The outer tissue gives capsular appearance with focal globular areas projecting inside. Centre of the specimen is filled with dark brown jelly like material.

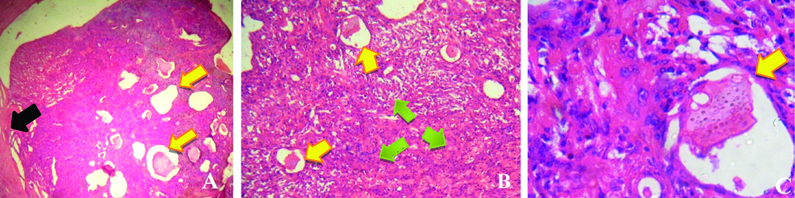
Histopathological features: (A) Scanner view, showing multicysticlesional tissue (yellow arrow) surrounded by thick fibrous capsule (black arrow); (B) In low power view, many cystic spaces (yellow arrow) of variable sizes are evident filled with eosinophillic material surrounded by dense cellularity (green arrow); (C) In high power view, section showing cystic space (yellow arrow) filled with eosinophillic material lined by flattened cells and surrounded by oval cells. Few papillary projections were also evident.
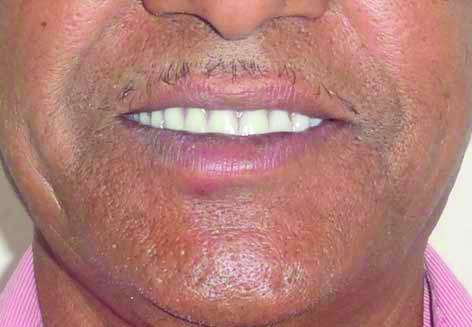
(A) Post-operative picture of the patient after denture insertion, showing no recurrence of the swelling after follow up for one year.
Papillary cystadenoma of the salivary glands is a rare benign tumor in which the epithelial proliferation is characterised by the formation of multiple cystic cavities containing intraluminal papillary projections [1]. It represents 0.7–8.1% of all benign salivary gland tumours, and almost 10.7% of cases found involving the lips [1,2]. It is a well-circumscribed or encapsulated tumour. Due to its well-circumscribed nature and indolent behaviour, the recurrence rate of papillary cystadenoma is low and the prognosis is good [3,4].
Papillary cystadenoma most commonly manifests in eighth decade of life with a mean age of occurrence of 57 years [1,2]. According to the literature, the cystadenomas are more frequent in males than in females, but occasionally female predominance is mentioned with a female: male ratio of 3:1 [5,6]. The palate was found to be the commonest site followed by upper lip, lower lip, and buccal mucosa. Clinically it manifests as an asymptomatic, slow growing mass, usually <1 cm in greatest dimension when arising in the minor salivary glands [1,2]. Similarly, in our case, patient was a 62-year-old male having lesion involving the upper lip with no associated pain or any altered sensation.
Histopathologically, papillary cystadenoma showed multiple cystic spaces of variable size, exhibiting intraluminal papillary projections. The tumour was typically well circumscribed and surrounded by a rim of fibrous tissue. The lining of the cystic structures was composed of a double layer of flattened to columnar epithelium. The cells were cuboidal, mucous and/ or oncocytic, without atypia. Focal variation in epithelial differentiation was common, but in an individual cystadenoma, a single cell type was characteristically predominant [1,2,6-8]. The definitive diagnosis can only be established by histopathological evaluation of this rare minor salivary gland neoplasm. However, in view of the complexity and histomorphological diversity of salivary gland tumours, the accurate histopathological diagnosis of cystadenoma required the elimination of similar lesions with analogous histopathological presentations such as intraductal papilloma, papillary cystadenocarcinoma, low-grade mucoepidermoid carcinoma and Warthin’s tumour [6,7,9].
Immunohistochemically, expression of pan-cytokeratin in tumour parenchyma is suggestive of origin of tumour tissue from epithelial or epidermal components. Cytokeratins including CK-8 are intermediate filaments expressed in cells of epithelial origin. Mucinous cystadenoma is a proliferation of epithelial and ductal cells of salivary gland. Therefore, intense cytokeratin intermediate filament expression was consistently observed in mucinous cystadenoma; while they show absence of immunoreactivity for Smooth Muscle Antigen (SMA), CD-113 and calponin, hence ruling out the tumours of myoepithelial, lymphoid, vascular and endothelial origin [1].
The recommended treatment for papillary cystadenoma is simple surgical excision, although follow up of the patient is necessary since recurrences due to incomplete excision have been reported [1,2]. In the present case, complete surgical excision of the lesion was done under local anaesthesia with an uneventful post-operative recovery, and no recurrence was found on follow up evaluation for one year.
[1]. Girotra C, Padhye MN, Mahajan P, Nair A, A rare case report of mucinous cystadenoma with immunohistochemical analysis and review of literatureJ Maxillofac Oral Surg 2015 14(Suppl 1):426-34.10.1007/s12663-014-0656-225861198 [Google Scholar] [CrossRef] [PubMed]
[2]. Ananthaneni A, Kashyap B, Prasad VR, Srinivas V, Cystadenoma: a perplexing entity with subtle literatureJ NTR Univ Health Sci 2012 1(3):179-81.10.4103/2277-8632.102448 [Google Scholar] [CrossRef]
[3]. Halbritter SA, Altermatt HJ, Caversaccio M, Bornstein MM, Apocrine papillary cystadenoma of a minor salivary gland on the lower lip: case presentationQuintessence Int 2009 40(2):167-69. [Google Scholar]
[4]. Lim CS, Ngu I, Collins AP, McKellar GM, Papillary cystadenoma of a minor salivary gland: report of a case involving cytological analysis and review of the literatureOral Surg Oral Med Oral Pathol Oral Radiol Endod 2008 105(1):e28-33.10.1016/j.tripleo.2007.07.01918155598 [Google Scholar] [CrossRef] [PubMed]
[5]. Whittaker JS, Turner EP, Papillary tumours of the minor salivary glandsJ Clin Path 1976 29(9):795-805.10.1136/jcp.29.9.795977781 [Google Scholar] [CrossRef] [PubMed]
[6]. Santos JND, Barros AC, Sarmento VA, Gurgel CAS, De Souza VF, Cystadenoma: a rare tumour originated in minor salivary glandJ Bras Patol Med Lab 2008 44(3):205-08.10.1590/S1676-24442008000300008 [Google Scholar] [CrossRef]
[7]. Tjioe KC, de Lima HG, Thompson LDR, Lara VS, Damante JH, de Oliveira-Santos C, Papillary cystadenoma of minor salivary glands: report of 11 cases and review of the english literatureHead Neck Pathol 2015 9(3):354-59.10.1007/s12105-014-0602-025547059 [Google Scholar] [CrossRef] [PubMed]
[8]. Tsurumi K, Kamiya H, Yokoi M, Kameyama Y, Papillary oncocyticcystadenoma of palatal minor salivary gland: a case reportJ Oral Maxillofac Surg 2003 61(5):631-33.10.1053/joms.2003.5012012730845 [Google Scholar] [CrossRef] [PubMed]
[9]. Auclair PL, Ellis GL, Gnepp DR, Surgical pathology of the salivary glands 1991 1st edPhiladelphiaSaunders:135-164. [Google Scholar]