Application of Le Fort I Osteotomy for Post-traumatic Malocclusion Secondary to Condylar Fractures in an Elderly Patient: A Case Report
Shinsuke Yamamoto1, Toshihiko Takenobu2, Izumi Kouchi3, Yuzo Hirai4, Naoki Taniike5
1 Assistant Head Physician, Department of Oral and Maxillofacial Surgery, Kobe City Medical Center General Hospital, Kobe, Hyogo, Japan.
2 Director, Department of Oral and Maxillofacial Surgery, Kobe City Medical Center General Hospital, Kobe, Hyogo, Japan.
3 Resident, Department of Oral and Maxillofacial Surgery, Kobe City Medical Center General Hospital, Kobe, Hyogo, Japan.
4 Clinical Fellow, Department of Oral and Maxillofacial Surgery, Kobe City Medical Center General Hospital, Kobe, Hyogo, Japan.
5 Head Physician, Department of Oral and Maxillofacial Surgery, Kobe City Medical Center General Hospital, Kobe, Hyogo, Japan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shinsuke Yamamoto, 2-1-1, Minatojima Minamimachi, Chuo-Ku, Kobe, Hyogo 650-0047, Japan.
E-mail: s.yamamoto@kcho.jp
The condylar region is a common site of mandibular fractures, and inadequate treatment of condylar fractures causes an anterior open bite. This malocclusion reduces the quality of life and requires surgical intervention in some cases. However, in elderly patients with a relevant history, the treatment method should be minimally invasive and safe. Here we report a rare case on the application of Le Fort I osteotomy for post-traumatic malocclusion secondary to condylar fractures in an elderly patient. A 76-year-old man with a medical history of a cerebral infarction and diabetes mellitus was referred to our department with the chief complaint of malocclusion. The diagnosis was post-traumatic malocclusion mainly secondary to condylar fractures. Le Fort I osteotomy was performed to re-establish the occlusion. The postoperative course was uneventful and normal occlusion and good mandibular mobility was achieved. The course of this patient provides two important suggestions. First, Le Fort I osteotomy is effective in improving post-traumatic malocclusion secondary to condylar fractures. Second, this method is minimally invasive and safe for treatment of elderly patients. This case report highlights the usefulness of Le Fort I osteotomy for post-traumatic malocclusion secondary to condylar fractures in elderly patients.
Mandibular fractures, Minimally invasive surgery, Open bite
Case Report
A 76-year-old man was referred to our department in August 2015 with the chief complaint of malocclusion. His past medical history included incomplete paralysis of the left upper limbs caused by cerebral infarction two years ago, diabetes mellitus for six years and an injury to the chin from a fall while walking in June 2015. He was admitted to another hospital and underwent conservative treatment for one month with a facial bandage for a diagnosis of bilateral subcondylar fractures and an incomplete Le Fort I type fracture. However, after discharge, he was concerned about malocclusion.
On examination, he had good facial symmetry and mobility of the mandible [Table/Fig-1a,b].
a) Frontal and b) open mouth photographs demonstrate good facial symmetry and mobility of the mandible; c) The occlusion showed an anterior open bite and slight deviation of the mandible to the left side.

There was no masticatory complex pain or temporomandibular joint sounds during function. The occlusion showed an anterior open bite and slight deviation in the mandible to the left side [Table/Fig-1c].
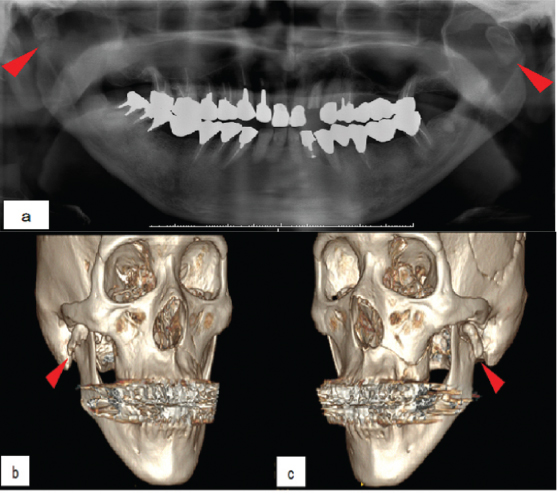
Panoramic radiography and computed tomography revealed bilateral subcondylar fractures with lateral displacement and bilateral ramus shortening with a Le Fort I type fracture without clear displacement [Table/Fig-2a,b,c]. We diagnosed a post-traumatic malocclusion secondary to bilateral condylar fractures and Le Fort I osteotomy under general anaesthesia was performed seven months after the fall. Considering that the patient had good mandibular function even though his condyle remained out of the fossae, we decided to use the mandible as a platform to re-establish the occlusion. Treatment planning performed using model surgery determined that a 3 mm posterior impaction and 1 mm rotation of the maxilla to the left side were needed. During surgery, a horizontal vestibular incision was made between the maxillary first molars and osteotomy in Le Fort I plane was performed. The mobilised maxilla was wired into the occlusion with the mandible using a surgical splint between the upper and lower dentition intraoperatively and fixed with titanium miniplates along the anterior and anterolateral maxillary buttresses [Table/Fig-3]. Postoperatively, the facial configuration was maintained, and normal occlusion was restored without the use of Maxillomandibular Fixation (MMF) or elastics [Table/Fig-4a,b].
a) Panoramic radiograph and b,c) 3D-CT at the initial visit. Panoramic radiograph and 3D-CT exhibit bilateral subcondylar fractures with lateral displacement (red arrow heads) and bilateral ramus shortening.
Intraoperative view: The mobilised maxilla is wired into the occlusion with the mandible with a splint between the upper and lower dentition.

a) Extraoral and b) intraoral photographs at 10 months postoperatively. A normal and stable occlusion was restored.

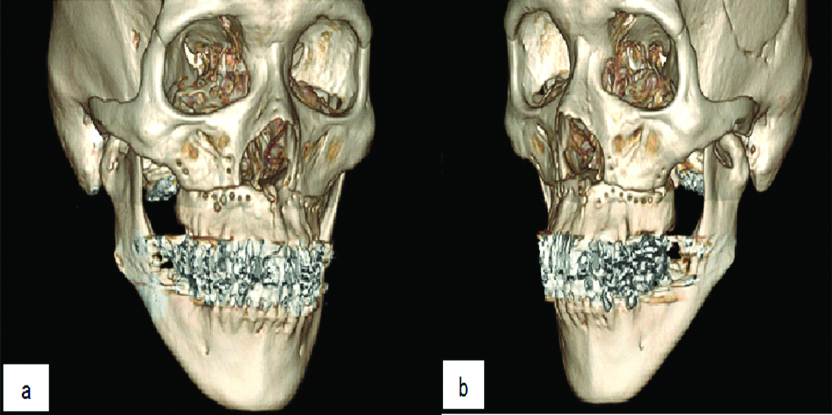
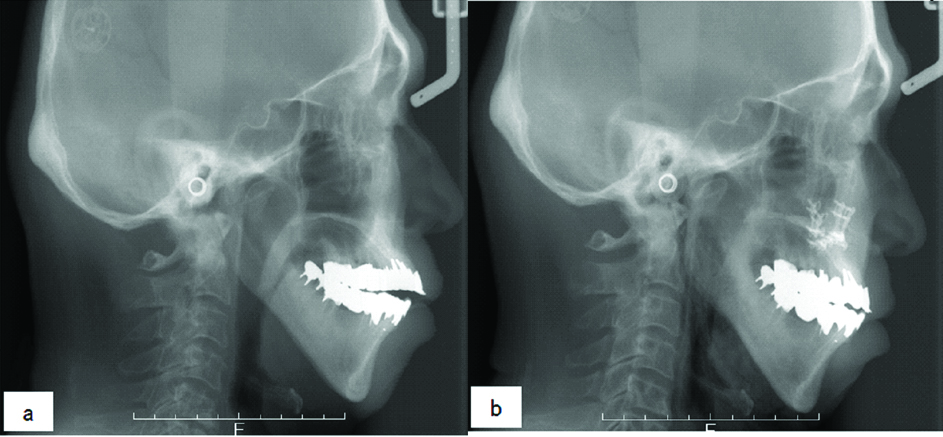
The postoperative course was uneventful, and he maintained normal and stable occlusion and good mandibular mobility even after one year and four months [Table/Fig-5a,b,6a,b].
a,b) A 3D-CT at 10 months postoperatively. A 3D-CT exhibits the malunion of bilateral subcondylar fractures and good bone healing after Le Fort I osteotomy.
Lateral cephalometric radiographs at the a) initial visit and b) postoperatively. The anterior open bite was improved by posterior impaction of the maxilla.
Discussion
The condylar region is a common site of mandibular fractures [1]. Treatment of condylar fractures has generated a great deal of discussion and controversy in maxillofacial trauma and many different treatment methods have been established. Recent studies suggest that open reduction and internal fixation is now considered as the treatment of choice for subcondylar and condylar neck fractures [2,3]. Furthermore, the transoral endoscopically assisted approach is reportedly useful for the treatment of subcondylar or condylar neck fractures. Thus, this procedure has gained popularity because of the greater effectiveness and lower risk of morbidity (e.g., facial nerve injury and aesthetic impairment) [3,4]. However, surgeons tend to choose conservative treatment for condylar fractures in some cases and facilities. The incidence of malocclusion secondary to condylar fractures is not clear [5], but Forouzanfar T et al., reported that 12% of bilateral condylar fractures treated conservatively had developed malocclusion [6]. A common malocclusion of bilateral condylar fractures is an anterior open bite caused by the loss of mandibular height bilaterally with clockwise rotation of the mandibular plane bilaterally [7]. This helps facilitate a new articulation by bringing the condylar stump closer to the cranial base and once a new articulation is established, the posterior vertical dimension stabilises [8].
Depending on the severity of the anterior open bite, treatment options of malocclusion secondary to bilateral condylar fractures include functional rehabilitation, occlusal equilibration, orthodontics, orthognathic surgery and temporomandibular reconstruction [5]. In particular, orthognathic surgery is the most predictable and stable method for the treatment of post-traumatic malocclusion [9]. For the treatment of an anterior open bite, the choice of performing mandibular or maxillary surgery depends on the position of the lower dental midline. Specifically, if there is a symmetrical minor anterior open bite from bilateral fractures, Le Fort I osteotomy can readily correct the malocclusion. On the other hand, if there is an asymmetric anterior open bite or severe deviation of the mandible to one side, then mandibular ramus surgery should be performed [5,8]. He D et al., reported the usefulness of a Le Fort I osteotomy for delayed panfacial fractures to re-establish proper occlusion [10]. Although, the present case had an anterior open bite with slight deviation of the mandible to the left side, we choose Le Fort I osteotomy to correct the malocclusion. Le Fort I osteotomy was not required to correct the mandibular ramus where the condylar malunions were located [5,7] because the risk of pain reactivation and altered function were more important than the problem of slight maxillary midline deviation to the left side in the present case. Moreover, a higher prevalence of temporomandibular joint problems occurs after mandibular ramus surgery than after Le Fort I osteotomy to close an anterior open bite [9]. When performing surgery, it is important to consider the timing. If the condyle continues to remodel postoperatively, the occlusion can change; therefore, we ensured that the new articulation functioned well and was stable prior to surgery [5,8]. In the present case, Le Fort I osteotomy was performed seven months after the fall as a latency period to stabilise the new articulation. In fact, the patient had good mandibular function even though the condyle remained out of the fossae at the time of the surgery. The stability of the occlusion was restored without postoperative use of MMF or elastics. Le Fort I osteotomy, which does not change the condylar position, is considered to be effective in improving post-traumatic malocclusion secondary to condylar fractures.
Majority fractures in elderly patients are caused by falling due to traffic accidents [11]. The elderly patients are more likely to have a relevant history of cardiovascular, respiratory or neurologic diseases, diabetes and osteoporosis that may subsequently alter the course of treatment [11-13]. Furthermore, they are at an increased risk of avascular necrosis, osseous ankylosis and fibrous ankylosis following surgery [11]. Henceforth, surgical intervention is indicated less frequently for facial trauma in elderly patients, and the risk of developing malocclusion secondary to condylar fractures is likely higher in elderly patients than in younger patients. The present case had incomplete paralysis of the left upper limbs caused by an old cerebral infarction; therefore, we had to choose a minimally invasive and safe method to correct the malocclusion. Normal and stable occlusion was achieved by Le Fort I osteotomy without the use of MMF or elastics postoperatively. As a result of a 3 mm impaction of the posterior maxilla, it was possible to avoid performing mandibular ramus surgery, while taking into account aesthetic outcomes by not changing point A. Shortly after surgery, the patient was able to eat a normal diet. Hence, this method should be considered minimally invasive and safe for the treatment of elderly patients.
Conclusion
Le Fort I osteotomy, can effectively improve post-traumatic malocclusion secondary to condylar fractures without any change in the position of the mandibular condyle. This method is minimally invasive and safe for elderly patients as does not require the use of maxillomandibular fixation and elastics.
[1]. Ellis E 3rd, Moos KF, el-Attar A, Ten years of mandibular fractures: an analysis of 2,137 casesOral Surg Oral Med Oral Pathol 1985 59(2):120-29.10.1016/0030-4220(85)90002-7 [Google Scholar] [CrossRef]
[2]. Neff A, Chossegros C, Blanc JL, Champsaur P, Cheynet F, Devauchelle B, Position paper from the IBRA Symposium on Surgery of the Head-the 2nd International Symposium for Condylar Fracture Osteosynthesis, Marseille, France 2012J Craniomaxillofac Surg 2014 42(7):1234-49.10.1016/j.jcms.2014.03.00524831849 [Google Scholar] [CrossRef] [PubMed]
[3]. Al-Moraissi EA, Ellis E 3rd, Surgical treatment of adult mandibular condylar fractures provides better outcomes than closed treatment: a systematic review and meta-analysisJ Oral Maxillofac Surg 2015 73(3):482-93.10.1016/j.joms.2014.09.02725577459 [Google Scholar] [CrossRef] [PubMed]
[4]. Schoen R, Fakler O, Metzger MC, Weyer N, Schmelzeisen R, Preliminary functional results of endoscope-assisted transoral treatment of displaced bilateral condylar mandible fracturesInt J Oral Maxillofac Surg 2008 37(2):111-16.10.1016/j.ijom.2007.06.01717822877 [Google Scholar] [CrossRef] [PubMed]
[5]. Ellis E 3rd, Walker RV, Treatment of malocclusion and tmj dysfunction secondary to condylar fracturesCraniomaxillofac Trauma Reconstr 2009 2(1):01-18.10.1055/s-0028-110290022110792 [Google Scholar] [CrossRef] [PubMed]
[6]. Forouzanfar T, Lobbezoo F, Overgaauw M, de Groot A, Kommers S, van Selms M, Long-term results and complications after treatment of bilateral fractures of the mandibular condyleBr J Oral Maxillofac Surg 2013 51(7):634-38.10.1016/j.bjoms.2012.12.00523375048 [Google Scholar] [CrossRef] [PubMed]
[7]. Maron G, Kuhmichel A, Schreiber G, Secondary Treatment of Malocclusion/Malunion Secondary to Condylar FracturesAtlas Oral Maxillofac Surg Clin North Am 2017 25(1):47-54.10.1016/j.cxom.2016.10.00328153182 [Google Scholar] [CrossRef] [PubMed]
[8]. Ellis E 3rd, Complications of mandibular condyle fracturesInt J Oral Maxillofac Surg 1998 27(4):255-57.10.1016/S0901-5027(05)80506-5 [Google Scholar] [CrossRef]
[9]. Becking AG, Zijderveld SA, Tuinzing DB, Management of posttraumatic malocclusion caused by condylar process fracturesJ Oral Maxillofac Surg 1998 56(12):1370-74.10.1016/S0278-2391(98)90394-9 [Google Scholar] [CrossRef]
[10]. He D, Zhang Y, Ellis E 3rd, Panfacial fractures: analysis of 33 cases treated lateJ Oral Maxillofac Surg 2007 65(12):2459-65.10.1016/j.joms.2007.06.62518022469 [Google Scholar] [CrossRef] [PubMed]
[11]. Nogami S, Yamauchi K, Yamashita T, Kataoka Y, Hirayama B, Tanaka K, Elderly patients with maxillofacial trauma: study of mandibular condyle fracturesDent Traumatol 2015 31(1):73-76.10.1111/edt.1212925233910 [Google Scholar] [CrossRef] [PubMed]
[12]. Goldschmidt MJ, Castiglione CL, Assael LA, Litt MD, Craniomaxillofacial trauma in the elderlyJ Oral Maxillofac Surg 1995 53(10):1145-49.10.1016/0278-2391(95)90620-7 [Google Scholar] [CrossRef]
[13]. Gerbino G, Roccia F, De Gioanni PP, Berrone S, Maxillofacial trauma in the elderlyJ Oral Maxillofac Surg 1999 57(7):777-82.10.1016/S0278-2391(99)90812-1 [Google Scholar] [CrossRef]