Introduction
Laryngeal Mask Airway (LMA) and combitube are used as an alternative to endotracheal tube for airway maintenance and in elective surgeries whenever required.
Aim
To compare the ease of insertion and haemodynamic changes of LMA and combitube in patients undergoing general anaesthesia.
Materials and Methods
The present prospective, comparative, randomised and observational study was conducted in Government Medical College and Rajindera Hospital, Patiala, Punjab, India (from December 2015 to November 2016) on 100 patients aged between 20 to 55 years of both sexes, belonging to the American Society of Anaesthesiologists (ASA) Grades I and II, scheduled for elective surgeries under general anaesthesia. The patients were randomly divided into two groups: Group L, LMA (n=50) and Group C, Combitube (n=50). The ease of insertion as per four grades, haemodynamic changes, changes in oxygen saturation (SpO2), End-tidal Carbon dioxide (EtCO2), and postoperative complications were recorded.
Results
The ease of insertion, SpO2 and EtCO2 in the Group L were statistically insignificant when compared to those in Group C (p>0.05). The increased haemodynamic changes (i.e., heart rate, systolic blood pressure, diastolic blood pressure, mean arterial pressure) observed in Group C when compared to those in Group L showed statistical significance immediately after insertion, one minute after insertion and three minutes after insertion (p<0.05), but not at five 10, and 15 minutes after insertion. Incidence of trauma was statistically significant in Group C (p<0.05), but postoperative sore throat was not statistically significant in both the groups (p>0.05).
Conclusion
This study suggests that both combitube and LMA are equally effective in airway maintenance in elective surgeries.
Introduction
Laryngeal mask airway was designed by Brain AI, in the year 1981 [1]. It was introduced into clinical practice in the year 1987, and it was found that the technique of insertion of LMA obviated the need for laryngoscopy, which was a major cause of the pressor responses. The LMA has gained widespread acceptance as a general purpose airway with worldwide usage estimated at over 10 million patients by 1993. The popularity of the device for routine use stems from its perceived benefits for the patients and anaesthetist over traditional forms of airway management. Prospective surveys have shown the overall success rate for the technique to be high and low complication rate [2-4].
Laryngeal mask airway offers a much less invasive way of maintaining the airway because it does not pass through the glottis but is placed over the glottis. It does not require instrumentation like the use of the laryngoscope. It acts as an intermediate between the Endotracheal Tube (ETT) and the oropharyngeal airway [5].
Relative contraindications to use of the LMA include situations associated with an increased risk of aspiration (full stomach, previous gastric surgery, Gastroesophageal Reflux (GER), diabetic gastroparesis, over 14 weeks pregnant, dementia, trauma, opiate medications and increased intestinal pressure) unless other techniques for securing the airway have failed. Absolute contraindications are complete airway obstruction and patient with difficult mouth opening [6].
The use of combitube is mainly for the unexpected difficult airway, failed tracheal intubation and perhaps the inability to visualise the vocal cords in a patient at risk of aspiration of gastric contents, e.g., upper airway bleeding or continued vomiting. It should be cautiously used in patients with cardiovascular or cerebrovascular disease. If insertion of the combitube is considered, effective measures should be implemented to minimize the stress responses [7].
The Frass M et al., invented the Oesophageal Tracheal Combitube (OTC) in an attempt to ease the method of securing an intact airway and to exclude the use of laryngoscopy and associated complication [8]. It scores satisfactorily in ease of insertion, successful first insertion, seal for Intermittent Positive Pressure Ventilation (IPPV) and minimal risk of aspiration [9,10].
Ventilation and oxygenation via the combitube showed comparable results to endotracheal intubation in patients with cardiopulmonary arrest or patients undergoing elective surgery. Blood gas analysis showed a significantly higher mean arterial oxygen tension (PaO2) in patients ventilated with the combitube. The higher level of PaO2 during ventilation with the combitube compared with the ETT may be explained by the difference in pressure waveform; with the combitube, inspiratory pressure increases more slowly and the expiratory flow time is prolonged with the formation of a small auto-positive end-expiratory pressure [11,12].
Minimal training is needed before use. The skills required to insert a combitube do not need to be reinforced as often as they do for tracheal intubation. The combitube can be used successfully by non-anaesthesia personnel both as a first-line treatment and after failed tracheal intubation. It is often used by paramedics [13,14].
Combitube and easy tube may be continued for general anaesthesia in patients undergoing elective non-laparoscopic surgeries of moderate duration if placed for airway maintenance. This is based on satisfactory intraoperative ventilatory maintenance and lack of any major intraoperative or postoperative complication necessitating active intervention [15].
Combitube has certain disadvantages such as its insertion is sometimes unsuccessful, is available in only two custom made sizes {Combitube 37 F SA (small adult), to be used in patients 4-6 feet in height (120-180 cm), and Combitube 41 F, for patients taller than 6 feet (180 cm)}, and is associated with increased airway trauma and overinflation of cuff [16].
The ASA task force on difficult airway management lists combitube, along with LMA and transtracheal jet ventilation, as one of three non-surgical “cannot ventilate-cannot intubate” rescue methods. Therefore, a combitube should be part of a portable kit for the management of difficult airways [17].
The present study was conducted to compare both devices, viz., combitube and LMA, with respect to the ease of insertion conditions, haemodynamic changes, and complications (if any) such as trauma, sore throat, and aspiration in patients undergoing elective surgeries under general anaesthesia in Government Medical College and Rajindera Hospital, Patiala, Punjab, India.
Materials and Methods
This prospective, comparative, randomised and observational study was conducted in Government Medical College and Rajindera Hospital, Patiala, Punjab, India (from December 2015 to November 2016) on 100 patients aged between 20 to 55 years of both sexes, belonging to ASA Grades I and II, and Mallampati grades one and two, scheduled for elective surgeries under general anaesthesia after getting approval from the Ethical Committee and obtaining written informed consent from the patients. Based on present pilot study, we calculated the sample size of atleast eight in each group with a power of 0.8 and type of error of 0.05. Due to availability of logistic support, 50 patients were taken in each group as there is no upper limit of sample size.
Exclusion Criteria
Exclusion criteria were patients with ASA Grade III and above, head and neck surgeries, anticipated difficult intubation; full stomach; regurgitation; prone position; suspected or detected nervous system, respiratory, renal, neuromuscular or psychiatric disorders; history of severe hepatic or renal disease; history of cardiovascular abnormalities; baseline heart rate <60 beats per minute; moribund obesity and patient refusal.
The patients were randomly divided into two groups: Group L, LMA (n=50) and Group C, Combitube (n=50). Randomisation was done by simple sealed envelope method. Each patient received injection of midazolam (2 mg) and phenergan (25 mg) in half an hour before the surgery as premedication.
Procedure
Intravenous access was established with an 18 gauge cannula after arrival in the anaesthetic room. After stabilisation period of five minutes, the baseline values of Heart Rate (HR), Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Mean Arterial Pressure (MAP) and SpO2 were recorded.
After confirming nil oral status, the patients were preoxygenated with 100% oxygen via a face mask for five minutes. The patients were induced with IV injections of glycopyrrolate (0.004 mg/kg), pentazocine (0.5 mg/kg), and propofol (2 mg/kg), and after confirming loss of the eye lash reflex, injection of succinylcholine (1.5 mg/kg, IV) was given. After one minute, in Group L, lubricated LMA of an appropriate size was inserted and in Group C, a lubricated combitube was inserted and secured blindly using the standard technique. They were fixed in midline and a bite block was placed. Air was injected following the manufacturer recommendation for both supraglottic devices. Proper placement of both devices was confirmed by bilateral equal chest movements or air entry, absence of gastric insufflations or absence of audible leak on gentle IPPV and square wave capnography. Ease of insertion was compared by four grades; Grade 1: excellent (no resistance to insertion), Grade 2: good (slight resistance to insertion), Grade 3: poor (moderate resistance to insertion), and Grade 4: impossible. If LMA or combitube insertion was unsuccessful after two attempts, the patients were excluded from the study [18].
Anaesthesia was maintained with manually IPPV using Bain’s circuit with N2O and O2 (50:50), isoflurane and using an injection of vecuronium bromide as the muscle relaxant. Ventilation was adjusted in such a way that the EtCO2 level maintained below 45 mmHg and SpO2 above 95%.
The HR, SBP, DBP, MAP, SpO2 and EtCO2 values were recorded just before induction, immediately after insertion, and at one, three, five, 10 and 15 minutes. Any kind of painful stimulus including surgical incision was not allowed while the readings were being recorded.
After the surgical procedure, residual paralysis was adequately reversed with injection of neostigmine (0.05 mg/kg) and glycopyrrolate (0.008 mg/kg). LMA was removed after ascertaining that the patient was awake and responsive. Cuff was partially deflated for removal of LMA. Combitube was removed after deflating both the cuffs.
After removal of airways, the patients were observed for complications such as trauma (traces of blood on combitube or LMA), aspiration and sore throat on the first postoperative day. All data were analysed statistically.
Statistical Analysis
Analysis was conducted using IBM SPSS Statistics (version 22.0). Numerical data were expressed as mean and standard deviation, and statistical analysis was carried out using the independent t-test to compare the two groups. For skewed data/scores, Mann–Whitney U test was used. Gender and ease of insertion (grades) were compared using Chi-square test. The p-value of <0.05 was considered as statistically significant.
Results
The demographic data of patients age, body weight and gender were similar in the two groups and were statistically comparable as p-value>0.05 [Table/Fig-1,2].
Distribution of patients according to age and weight in Group C and Group L.
| Groups | Mean±SD | Mean difference | p-value |
|---|
| Age (years) | C | 50 | 39.58±9.95 | 1.66 | 0.435 |
| L | 50 | 37.92±11.19 |
| Weight | C | 50 | 64.66±7.86 | 1.56 | 0.356 |
| L | 50 | 63.10±8.91 |
Distribution of patients according to gender in Group C and Group L (p>0.05).
| Gender | Group C | Group L |
|---|
| No. of patients | % | No. of patients | % |
|---|
| Male | 16 | 32 | 18 | 36 |
| Female | 34 | 68 | 32 | 64 |
| Total | 50 | 100 | 50 | 100 |
| Chi-square value | 0.178 |
| p-value | 0.673 |
Ease of Insertion
In the present study, as per the ease of insertion conditions, the patients were graded as 1, 2, 3, and 4. In Group L, 64% patients had Grade 1, 32% Grade 2, and 4% Grade 3 whereas in Group C 58% patients had Grade 1, 32% Grade 2, and 10% Grade 3. There was no Grade 4 insertion in either group. Airway device insertion success rate was 100% in all the patients and number of attempts was first or second in each group. The ease of insertion in Group L was statistically comparable to that in Group C. In all 100 patients, airway maintenance using LMA and combitube was possible throughout the surgery duration. There was no significant difference between the two groups (p>0.05) [Table/Fig-3].
Ease of insertion (Grades) in Group C and Group L (p >0.05).
| Ease of Insertion | Group C | Group L |
|---|
| No. of patients | % | No. of patients | % |
|---|
| Grade 1 | 29 | 58 | 32 | 64 |
| Grade 2 | 16 | 32 | 16 | 32 |
| Grade 3 | 5 | 10 | 2 | 4 |
| Total | 50 | 100 | 50 | 100 |
| Chi-square value | 1.433 |
| p-value | 0.488 |
Heart Rate, Systolic Blood Pressure, Diastolic Blood Pressure and Mean Arterial Pressure
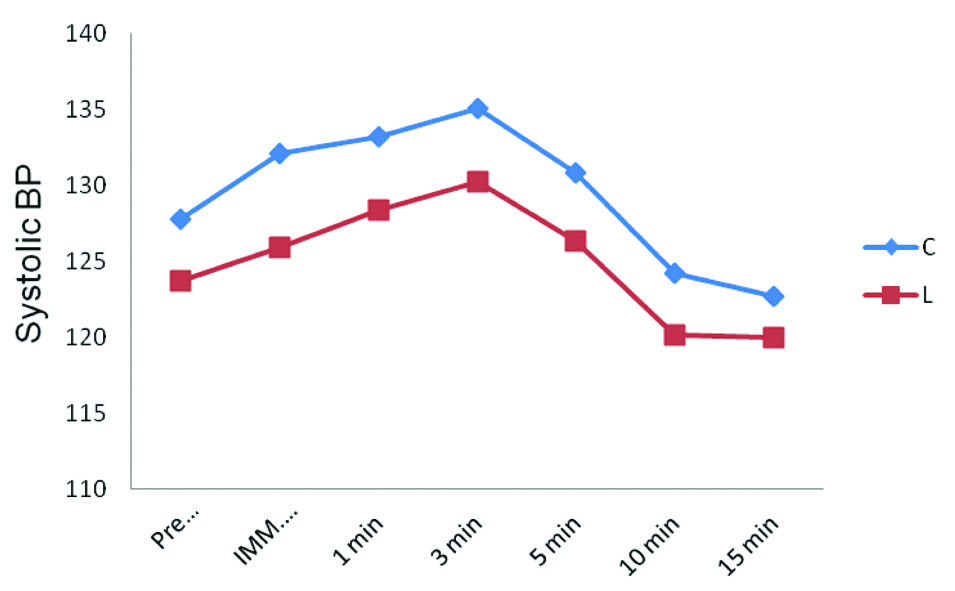
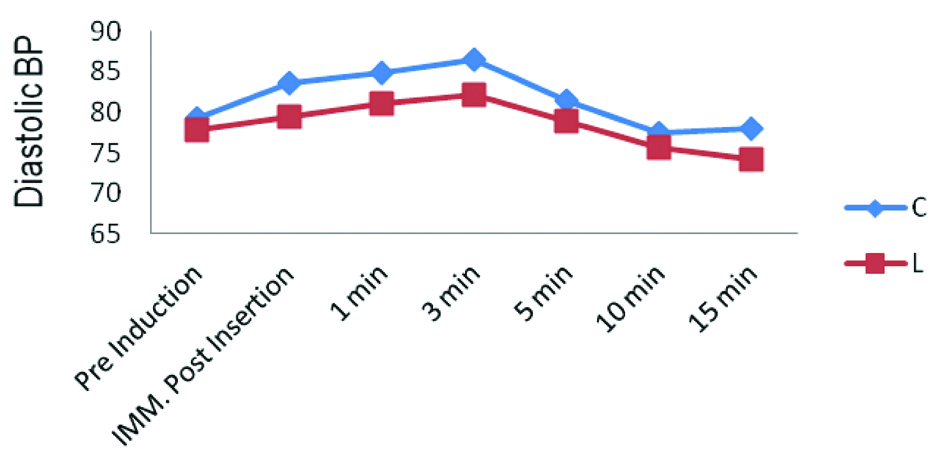
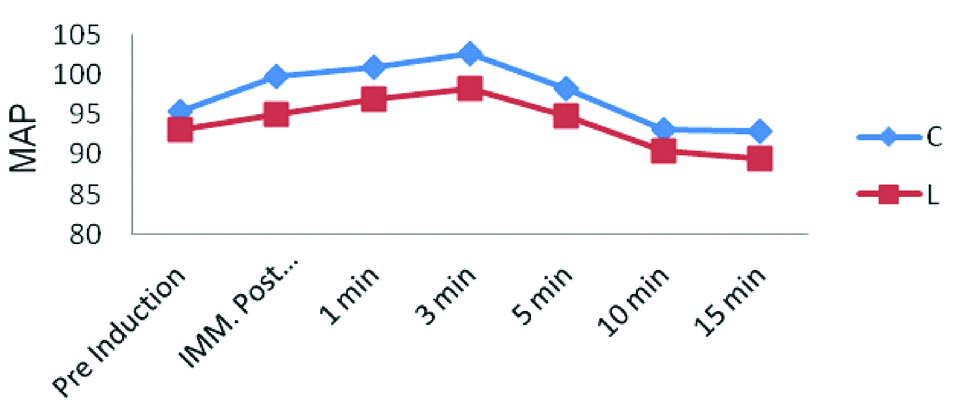
The values of HR, SBP, DBP, and MAP in Group C were significantly increased immediately after insertion, one minute, three minutes compared to those in Group L and then declined gradually, reaching to the near baseline value at the end of 15 minutes. There were statistically significant differences in HR, SBP, DBP, and MAP at immediately after insertion, one minute, and three minutes but not at five, 10, and 15 minutes [Table/Fig-4,5,6 and 7].
Heart rate at different time intervals in both groups represents the increased mean heart rate measurement Group C compared to the Group L was statistically significant at immediate post insertion, one and three minutes as p-value<0.05.

Systolic blood pressure at different time intervals in both groups represents the increased SBP measurement Group C compared to the Group L was statistically significant at immediate post insertion, one and three minutes as p-value<0.05.
Diastolic blood pressure at different time intervals in both groups represents the increased DBP measurement Group C compared to the Group L was statistically significant at immediate post insertion, one and three minutes as p-value<0.05.
Mean arterial pressure at different time intervals in both groups represents the increased MAP measurement Group C compared to the Group L was statistically significant at immediate post insertion, one and three minutes as p-value<0.05.
Saturation of Peripheral Oxygen
Levels of SpO2 were comparable in both the groups without any significant change in baseline (p-value>0.05). They remained 100% throughout the surgery in both the groups.
End-tidal Carbon Dioxide
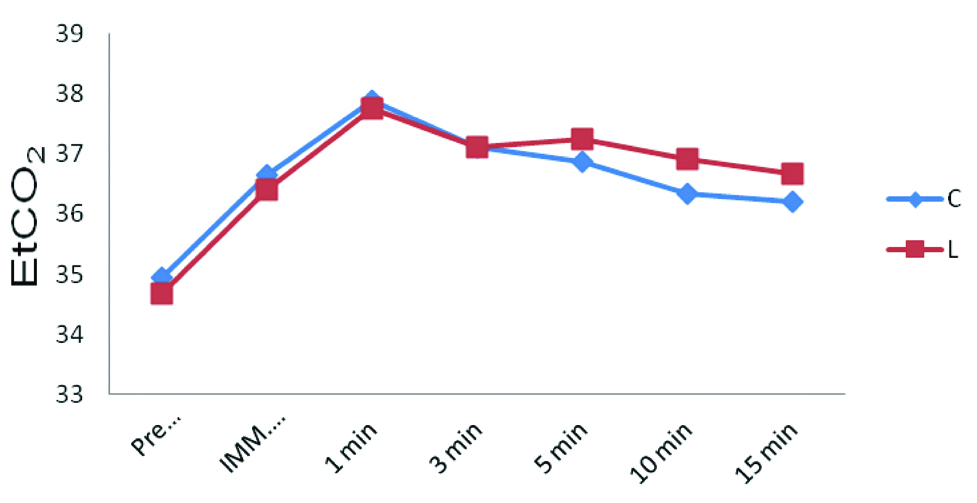
There was no significant difference between the two groups (p>0.05). Levels of EtCO2 were comparable in both the groups. Mean EtCO2 was maintained between 34 and 40 mmHg during the study [Table/Fig-8].
End-tidal carbon dioxide at different time intervals in both groups represents statistically comparable results (p>0.05).
Postoperative Complication
Incidence of trauma was only present in Combitube group which was statistically significant (p<0.05). Incidence of sore throat in LMA group (10%) is less as compared to Combitube group (16%) which was not statistically significant (p>0.05). There was no incidence of postoperative aspiration in both the groups (p>0.05) [Table/Fig-9].
Postoperative complications.
| Complications | Groups | Yes | No | p-value | Sig. |
|---|
| N | Age (%) | N | Age (%) |
|---|
| Trauma | C | 06 | 12 | 44 | 88 | 0.012 | S |
| L | 00 | 0 | 50 | 100 |
| Sore throat | C | 08 | 16 | 42 | 84 | 0.372 | NS |
| L | 05 | 10 | 45 | 90 |
| Aspiration | C | 00 | 0 | 50 | 100 | 1.000 | NS |
| L | 00 | 0 | 50 | 100 |
NS: Normal Saline
Discussion
Ease of insertion was assessed and was comparable in both groups. The results obtained in the present study were similar to those reported by Oczenski W et al., who showed that Combitube group had excellent to good scores in 84% and poor score in 16% patients and that LMA group had excellent to good scores in 92% of patients, but in the remaining 8% patients, LMA insertion was not possible and they had to be intubated [7]. In the present study, airway device insertion was successful in all the patients of both the groups and placement of the combitube was always oesophageal. The probable reason for this might be use of the succinylcholine (1.5 mg/kg, IV) and airway insertion was attempted after two minutes in the present study whereas Oczenski W et al., had used rocuronium (0.6 mg/kg, IV) and airway insertion was attempted after two minutes [7].
The results obtained in the present study were also similar to those reported by Sangani S et al., who reported both groups had excellent to good scores in 100% patient and no Grades 3 and 4 were observed [18]. The ease of insertion in LMA group was comparable to that in Combitube group (p>0.05).
Haemodynamic parameters like HR, SBP, DBP, MAP were recorded and were less in LMA group as compared to Combitube group. The results obtained in the present study were similar to those reported by Oczenski W et al., [7].
The results obtained in the present study were different from study reported by Sangani S et al., in which there was significant increase in HR, SBP, DBP, and MAP-values at one and two minutes after insertion of airway device in both groups [18]. They remained near the baseline till postoperative period. The reason for the significant increase in HR, SBP, DBP, and MAP values in both the groups in this study might be because of the difference in induction agents used, i.e., injection of thiopentone 5-7 mg/kg in that study whereas in the present study, we used injection of propofol (2 mg/kg) as induction agents.
Levels of SpO2 remained 100% throughout the surgery. There was no incidence of hypoxia throughout the surgery. The results obtained in the present study were similar to those shown in other studies [7,19].
EtCO2 was maintained between 34 and 40 mmHg during the study. There was no incidence of hypercarbia throughout the surgery. The results in the present study were similar to those reported in other studies [7,19].
At removal of the airway, traces of blood on combitube were observed in six patients and there was no oedema of the tongue or airway obstruction after removal of the airway. At 12 hour after the airway insertion, five patients complained of sore throat in LMA group and eight patients complained of sore throat in Combitube group. These complaints were mild in all patients and subsided within 24 hour after surgery. There was no incidence of postoperative aspiration in both the groups.
The results obtained in the present study were similar to study conducted by Sangani S et al., in which incidence of trauma was significantly present in 16.66% of patients in Combitube group and no incidence in LMA group. Incidence of sore throat in LMA group (10%) is less as compared to Combitube group (20%) [18].
The results obtained in the present study were similar study conducted by Hagberg CA et al., in which the combitube was comparable to the LMA regarding the incidence of GER and tracheal acid aspiration [19].
Limitation
The present study has several limitations. We focussed on airway complications due to the impact of the device on direct surrounding tissues. Complications such as regurgitation and vomiting were excluded from further evaluation. These findings need to be taken into account before one may conclude if use of the combitube is superior to LMA. In addition, as contraindications exist for the use of supraglottic airway devices, only a subgroup of surgical patients can be used for a random choice between LMA and combitube. This limits applicability of the study findings.
Conclusion
The ease of insertion of LMA and combitube was comparable; however, the haemodynamic changes in LMA were less as compared to combitube. Incidence of trauma was observed only in Combitube group and that of postoperative sore throat was slightly higher in Combitube group as compare to LMA. There was no incidence of postoperative aspiration in both the groups. These complaints were mild in all patients and subsided within 24 hour after surgery. We conclude that both combitube and LMA are equally effective in airway maintenance in elective surgeries.
[1]. Brain AI, The development of the laryngeal mask–a brief history of the invention, early clinical studies and experimental work from which the laryngeal mask evolvedEur J Anaesthesiol 1991 4:05-17. [Google Scholar]
[2]. Fujii Y, Tanaka H, Toyooka H, Circulatory responses to laryngeal mask airway insertion or tracheal intubation in normotensive and hypertensive patientsCan J Anaesthesiol 1995 42(1):32-36.10.1007/BF030105687534216 [Google Scholar] [CrossRef] [PubMed]
[3]. Brain AI, The laryngeal mask-a new concept in airway managementBr J Anaesth 1983 55(8):801-05.10.1093/bja/55.8.8016349667 [Google Scholar] [CrossRef] [PubMed]
[4]. Brimacombe J, The advantages of the LMA over the tracheal tube or facemask: a meta-analysisCan J Anaesth 1995 42(11):1017-23.10.1007/BF030110758590490 [Google Scholar] [CrossRef] [PubMed]
[5]. Morgan GE, Mikhail MS, Murray MJ, Clinical Anaesthesiology 2008 4th edNew YorkLange Medical Books/McGraw-Hill:97-110. [Google Scholar]
[6]. Dorsch JA, Dorsh SE, Supraglottic airway devicesIn: Understanding anaesthesia equipment 2008 5th edLippincott William and Wilkins:462-93. [Google Scholar]
[7]. Oczenski W, Krenn H, Dahaba AA, Hemodynamic and catecholamine stress responses to insertion of Combitube, laryngeal mask airway or tracheal intubationAnaesth Analg 1999 88:1389-94.10.1213/00000539-199906000-00035 [Google Scholar] [CrossRef]
[8]. Frass M, Frenzer R, Zdrahal F, Hoflehner G, Porges P, Lackner F, The esophageal tracheal combitube preliminary results with a new airway for CPRAnn Emerg Med 1987 16:768-72.10.1016/S0196-0644(87)80571-1 [Google Scholar] [CrossRef]
[9]. Urtubia RM, Aguila CM, Cumsille MA, Combitube: a study for proper useAnaesth Analg 2000 90(4):958-62.10.1213/00000539-200004000-00034 [Google Scholar] [CrossRef]
[10]. Roy K, Hemavathi B, Ravishankar M, Combitube for routine airway maintenance in elective surgeryJ Anaesth Clin Pharmacol 2005 21(3):283-86. [Google Scholar]
[11]. Frass M, Frenzer R, Rauscha F, Schuster E, Glogar D, Ventilation with the esophageal tracheal Combitube in cardiopulmonary resuscitation. Promptness and effectivenessChest 1988 93:781-84.10.1378/chest.93.4.7813349834 [Google Scholar] [CrossRef] [PubMed]
[12]. Frass M, Rodler S, Frenzer R, Ilias W, Leithner C, Lackner F, Esophageal tracheal Combitube, endotracheal airway, and mask: comparison of ventilatory pressure curvesJ Trauma 1989 29:1476-79.10.1097/00005373-198911000-000042585558 [Google Scholar] [CrossRef] [PubMed]
[13]. Dorsch JA, Dorsh SE, Devices for managing the difficult airwayIn: Understanding anaesthesia equipment 2008 5th edLippincott William and Wilkins:661-64. [Google Scholar]
[14]. Yardy N, Hancox D, Strang T, A Comparison of two airway aids for emergency use by unskilled personnelAnaesthesia 1999 54:181-83.10.1046/j.1365-2044.1999.00651.x10215715 [Google Scholar] [CrossRef] [PubMed]
[15]. Sethi AK, Desai M, Tyagi A, Kumar S, Comparison of combitube, easy tube and tracheal tube for general anaesthesiaJ Anaesthesiol Clin Pharmacol 2014 30(4):526-32.10.4103/0970-9185.14284925425779 [Google Scholar] [CrossRef] [PubMed]
[16]. Krafft P, Nikolic A, Frass M, Esophageal rupture associated with the use of the CombitubeAnaesth Analg 1998 87:145710.1097/00000539-199812000-000599842855 [Google Scholar] [CrossRef] [PubMed]
[17]. Practice guidelines for management of the difficult airwayA report by the American Society of Anaesthesiologists Task Force on management of the difficult airwayAnaesthesiology 1993 78:597-602.10.1097/00000542-199303000-00028 [Google Scholar] [CrossRef]
[18]. Sangani S, Vasava JC, Swadia VN, Comparison of clinical performance of Combitube with classic laryngeal mask airway in elective surgeries–a pilot studyInt J Res Med 2013 2(3):25-30. [Google Scholar]
[19]. Hagberg CA, Vartazarian TN, Chelly JE, Ovassapian A, The incidence of GER and tracheal aspiration detected with pH electrodes is similar with the laryngeal mask airway and esophageal tracheal combitube–a pilot studyCan J Anaesth 2004 51:243-49.10.1007/BF0301910415010407 [Google Scholar] [CrossRef] [PubMed]