Survival Impact of Postoperative Adjuvant Radiotherapy for Treatment of Advanced Stage Maxillary Sinus Cancer Patients
Upendra Nandwana1, Manoj Verma2, Tej Prakash Soni3, Naresh Jakhotia4, Nidhi Patni5, Anil Kumar Gupta6, Lalit Mohan Sharma7, Rajesh Pasricha8
1 Senior Resident, Department of Radiation Oncology, BMCHRC, Jaipur, Rajasthan, India.
2 Senior Resident, Department of Preventive and Social Medicine, AIIMS, Jodhpur, Rajasthan, India.
3 Consultant, Department of Radiation Oncology, BMCHRC, Jaipur, Rajasthan, India.
4 Consultant, Department of Radiation Oncology, BMCHRC, Jaipur, Rajasthan, India.
5 Consultant, Department of Radiation Oncology, BMCHRC, Jaipur, Rajasthan, India.
6 Consultant, Department of Surgical Oncology, BMCHRC, Jaipur, Rajasthan, India.
7 Consultant, Department of Medical Oncology, BMCHRC, Jaipur, Rajasthan, India.
8 Consultant, Department of Radiation Oncology, AIIMS, Rishikesh, Utharakhand, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Upendra Nandwana, 4 E-17, Rangbari Yojna, Kota-324005, Rajasthan, India.
E-mail: upendranandwana@gmail.com
Introduction
Maxillary sinus cancer is a rare disease and usually present in advanced stage. Limited clinical data exists from India about the use of adjuvant radiotherapy in advanced cases and survival thereafter.
Aim
To study survival and identify prognostic factors of importance in patients irradiated postoperatively for advanced stage maxillary sinus carcinoma.
Materials and Methods
Medical records of 25 patients of advanced stage maxillary sinus carcinoma treated with curative intent from January 2011 to November 2016 were analysed retrospectively. All the patients underwent primary surgery followed by postoperative adjuvant radiotherapy. Survival analysis was done using Kaplan-Meier method.
Results
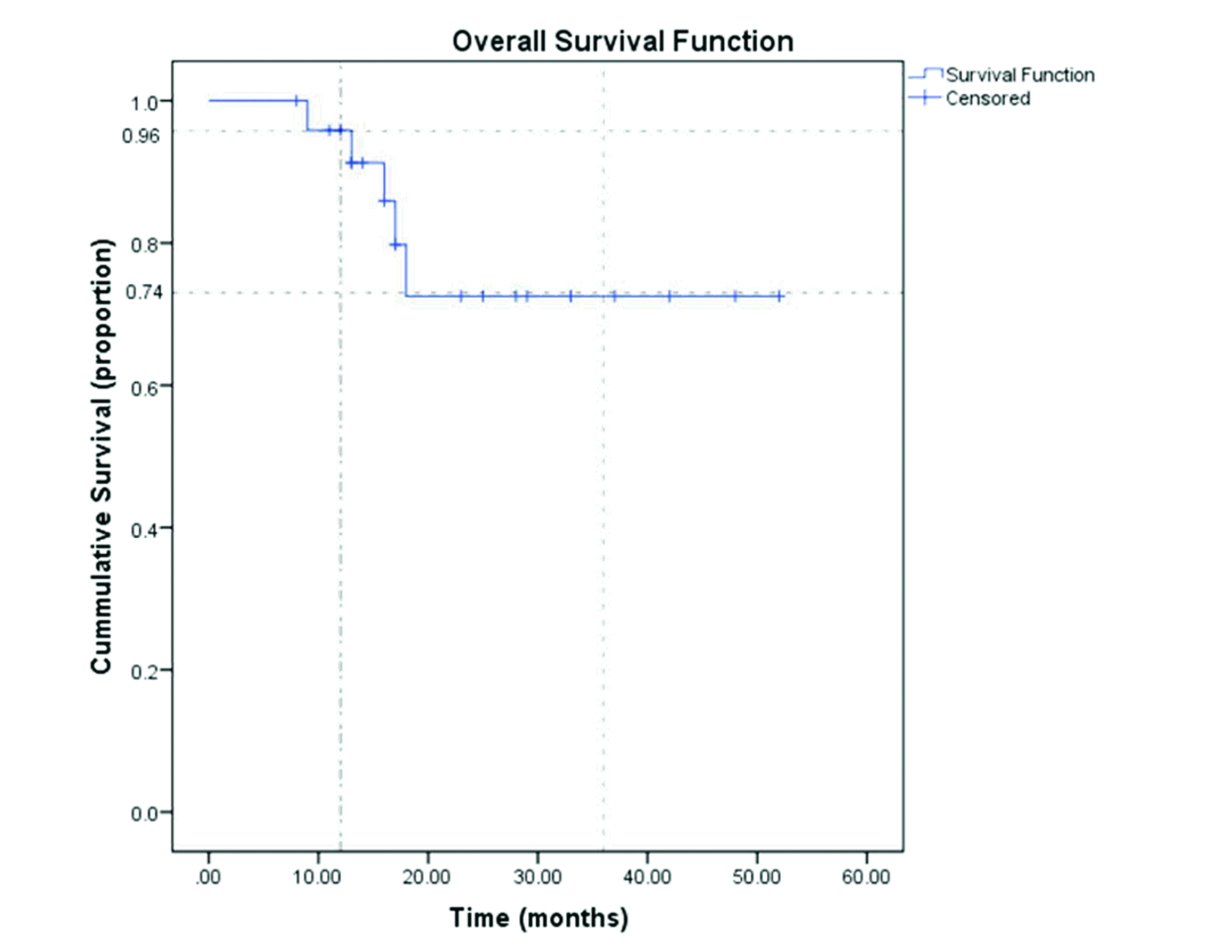
All patients presented with advanced disease Stage III or IV; nodal involvement was observed in 5 (20%) patients. The three-year overall survival after surgery and postoperative radiotherapy with or without concurrent chemotherapy was 74%. Median survival was 17 months. Most common pattern of recurrence was at the primary site, observed in 5 (20%) patients. Lymph node involvement, pT4 lesion, surgical margins positive, depth of invasion >10 mm, high grade, lymphovascular/perineural invasion were prognostic factors of importance.
Conclusion
Primary surgical treatment of maxillary sinus carcinoma in advanced stage followed by postoperative adjuvant radiotherapy is a good treatment option.
Carcinoma, Maxilla, Survival analysis
Introduction
Malignancy of the maxillary sinus is rare, occurs in approximately 1 in 100,000 people and amounts to 3% of all head and neck cancers. Carcinomas of the maxillary sinus comprise nearly 80% of all cases of paranasal sinus tumours [1-4]. It is almost twice as common in males as female, with most common incidence after 40 years of age [5]. The treatment of maxillary sinus carcinoma is challenging as they often present in advanced stage. Multimodal approach including surgery, radiotherapy and chemotherapy has been used for treatment of maxillary carcinoma [6-9]. Optimal therapy remains to be defined in advanced stages III and IV of maxillary carcinoma with many concepts being defined in literature, some recommend neoadjuvant chemotherapy to be given first followed by surgery or radiotherapy [10] while some recommend direct upfront chemoradiotherapy [11]. Few studies have reported use of surgery alone without adjuvant radiotherapy due to fear of increased risk of toxicity [12]. Uncertainty exists regarding fundamental management of this rare malignancy. Protocol followed in this institute was primary surgery followed by radiotherapy with or without chemotherapy and present study intend to present the survival advantage achieved by this protocol. The purpose of this study was to determine survival in advanced stage maxillary sinus carcinoma treated by surgery and postoperative adjuvant radiotherapy and to identify factors associated with poor survival.
Materials and Methods
A retrospective survival analysis was conducted at Bhagwaan Mahaveer Cancer Hospital and Research Institute, Jaipur, Rajasthan, India, from January 2016 to Novemeber 2016. Ethical clearance was taken from Institutes Ethical Committee prior to data collection. Incisional biopsy confirmed advanced stage maxillary carcinoma treated with curative intent at this centre between January 2011 and November 2016 were included in the study. Patients who were treated for palliative intent or those who had undergone prior treatment at other centre was not included in study. Twenty five eligible cases that were treated with curative intent and did not receive any treatment at other centre were included in the study. On physical examination, most common findings were facial swelling, intranasal mass and trismus. No patient had distant metastases at the time of diagnosis. Imaging usually comprised of computed tomography. All patients were restaged retrospectively according to the American Joint Committee on Cancer Staging System for maxillary sinus tumours [8]. Data were collected regarding their sociodemographic profile, clinical profile, histology, imaging, recurrence and survival. All patients underwent primary surgery followed by postoperative adjuvant radiotherapy with/without concomitant chemotherapy. Total maxillectomy was done in all the cases. Out of 25 patients, 18 (72%) patients underwent a neck dissection out of which Modified Neck Dissection (MND) was done in 14 patients and Supraomohyoid Neck Dissection (SOHND) was done in 4 patients. Eighteen patients received concurrent chemotherapy due to adverse risk factors like margins positivity, extracapsular extension, lymphovascular/perineural invasion etc. Remaining seven patients did not receive concurrent chemotherapy due to absence of these factors. Concurrent chemotherapeutic agents used was either injection Cisplatin 50 mg IV every week or injection Carboplatin 150 mg IV weekly. Postoperative adjuvant radiotherapy to all patients was started within 4-6 weeks of primary surgery. The dose of postoperative adjuvant radiotherapy was from 60 Gy-66 Gy in 30-33 sittings @2G/fraction, five days a week given by 6 Mv photons by LA 3DCRT or IMRT or IGRT technique. The regional nodes were only treated in patients with neck node involvement.
Statistical Analysis
Continuous data were expressed as mean±SD and categorical data as proportion (%). Overall survival and disease free survival were calculated using the Kaplan-Meier method. These end points were calculated from the date of diagnosis until the event of death (for overall survival) and local, regional or distant failure (for disease free survival). The mean and median follow up times were 22 and 17 months respectively. Statistical analysis was done using SPSS trial version 20.0.
Results
Histopathology confirmed squamous cell carcinoma in 20 patients, adenocarcinoma in 2 patients and adenocystic carcinoma in 3 patients. Most of the cases were males 16 and only 9 were females. Mean age of study subjects was 50.96±19 years with a range of 18-75 years. Most common presenting symptom was facial swelling, followed by oral symptoms and nasal obstruction. All patients presented with advanced Stage III and IV. Nodal disease at presentation was seen in 5 (20%) patients. Four patients had N1 disease and one patient had N2 disease. Two patients had T2 lesion, ten patients had T3 lesion and thirteen patients had T4 lesion. Negative resection margins were achieved in 20 patients (80%) and 5 patients (20%) had positive margins. The 1 and 3-year overall survival of patients with advanced maxillary sinus carcinoma were 96% and 74% respectively [Table/Fig-1]. Median survival was 17 months. In 20 (80%) patients there was no clinical evidence of disease and they were alive at the time of study. Overall 5/25 (20%) developed recurrent disease and died due to it. The majority of recurrences were within one year of diagnosis. The most common site of recurrence was at the primary site and occurred in patients with positive surgical margins. Patients who exhibited pT4 lesion, nodal disease N1-2, pathological Grade 3 [13], lymphovascular/perineural invasion, depth of invasion >1cm exhibited a lower rate of survival [Table/Fig-2].
Kaplan-Meier curve for overall survival of advanced maxillary sinus carcinoma patients managed with primary surgery and postoperative adjuvant radiotherapy.
Three year survival in relation to prognostic factors.
| Number of Patients | Number of patient who survived disease free for 3 years (3 years survival %) |
|---|
| Age (years) | <50 | 11 | 2 (18.18) |
| ≥50 | 14 | 2 (14.28) |
| Gender | Male | 16 | 2 (12.5) |
| Female | 9 | 2 (22.22) |
| T stage | T3 | 10 | 2 (20) |
| T4 | 13 | 1 (7.69) |
| Node | N0 | 20 | 4 (20) |
| N1-2 | 5 | 0 (0) |
| Grade [13] (n=20) | 1 | 10 | 3 (30.0) |
| 2 | 6 | 1 (16.66) |
| 3 | 4 | 0 (0) |
| PNI+ | 2 | 0 (0) |
| LVI+ | 2 | 0 (0) |
| DOI (n=20) | >1cm | 8 | 1 (12.5) |
| <1cm | 12 | 3 (25) |
For grading and DOI, only squamous cell carcinoma cases were included.
PNI-perineural invasion, LVI-lymphovascular invasion
Discussion
Maxillary sinus carcinoma is a rare disease, it occurs less frequently than that of buccal mucosa, retromolar trigone and floor of mouth or lip [14]. Patients usually present in advanced stage as symptoms are non specific and vague and appear much later. In present study majority of the patients were of T3 and T4 stages, males were more commonly affected. Similar distribution have been reported in published literature [3,4,15]. In present study, most common clinical presentation was facial swelling, followed by oral symptoms and nasal obstruction as was similarly reported by Waldron JN et al., [15] in a series of 110 patients, where oral symptoms (38%), facial swelling (40%) and nasal obstruction (35%) and epistaxis (25%) were most common presentation. Cervical lymphadenopathy was seen in 5 (20%) patients at the time of presentation. This is consistent with most other studies where lymph node involvement has been reported in 7% to 22% cases [16-18]. Surgery and radiotherapy given as combined modality had been the mainstay for treatment of squamous cell carcinoma of the maxillary sinus because this approach had demonstrated superior outcomes. St-Pierre S and Baker SR [9] in a study on 66 patients reported better survival in patients receiving combined surgery and radiotherapy. Paulino AC et al., [18] in a study of 42 patients reported higher overall survival rate (52%) in patient treated with surgery and postoperative radiotherapy as compared to patients treated with radiotherapy alone (0%). Blanco AI et al., [7] in a study of 106 patients noted a 35% disease free survival rate in patients receiving combined modality treatment compared to only 29% in patients receiving radiation alone. A local control rate of 60% was observed by Chen AM et al., [19] in T3 and T4 cases of sinonasal carcinoma. The excellent results of survival at 1-year and 3-year in present study as compared to above mentioned studies also supports the above notion that in advanced stages maxillary carcinoma primary surgery should be followed by postoperative adjuvant radiation therapy to increase the chance of cure and improve survival.
The main reason of treatment failure in maxillary sinus carcinoma is local recurrence [6-9]; hence, treatment modalities should target for better local control. In present study, local reoccurrence was also seen in 20% of the patients and was the most common pattern of recurrence. Frozen section should be included in the diagnosis of maxillary sinus carcinoma as it helps in knowing the positive margins of the cancer and helps in deciding the treatment modality [20]. These positive cases are the ones in which the outcome was poorer. In present study, treatment protocol of primary surgery followed by postoperative adjuvant radiation in advanced stage maxillary carcinoma achieved a 3-year survival rate of 74%. In present study, poor survival was seen in patients who presented with pT4 (7.69%), N1-2 (0%), Grade 3 (0%), LVI/PNI (0%), DOI>1cm (12.5%). Poor prognostic factors reported by Fan KH et al., [21] were poor differentiation, perineural invasion, lymphatic invasion, bone invasion, location (hard palate and retromolar trigone), invasion depths ≥10 mm, and margin distances ≤4 mm. In yet another study by Lin CY et al., [22], primary tumour site and neck stage were found to be prognostic factors of importance in advanced stage oral cancer patients who received radical radiotherapy. A retrospective study done by Qureshi SS et al., [23] found a 3 and 5-year overall survival rate of 38% and 35% respectively, with primary site failure in 35% cases. In present series of patients excellent survival rate was achieved due to better radiation delivery techniques with increased effect and less side effects.
Limitation
As this study was retrospective in nature it carried all inherent limitations associated with it like non randomisation and retrospective staging. Also the sample size (n=25) was small in this study so it seems that prospective randomised study with large sample size need to be conducted in future.
Conclusion
Present study highlights the importance of postoperative adjuvant radiotherapy in management of advanced stages maxillary sinus carcinoma with good survival rate and decreased recurrence. Recurrence occurred mostly in margins positive patients; hence meticulous surgery with clear margins should be aimed for. Pathological T4 lesion, lymph node involvement, DOI >10 mm, high grade, LVI, PNI are prognostic factors of importance and should be kept in mind while deciding individual treatment plan.
For grading and DOI, only squamous cell carcinoma cases were included.
PNI-perineural invasion, LVI-lymphovascular invasion
[1]. Bristol IJ, Ahamad A, Garden AS, Morrison WH, Hanna EY, Papadimitrakopoulou VA, Postoperative radiotherapy for maxillary sinus cancer: longterm outcomes and toxicities of treatmentInt J Radiat Oncol Biol Phys 2007 68(3):719-30.10.1016/j.ijrobp.2007.01.03217543999 [Google Scholar] [CrossRef] [PubMed]
[2]. Roush GC, Epidemiology of cancer of the nose and paranasal sinuses: current conceptsHead Neck Surg 1979 2(1):03-11.10.1002/hed.2890020103 [Google Scholar] [CrossRef]
[3]. Silverberg E, Grant RN, Cancer statistics,1970CA Cancer J Clin 1970 20(1):11-23.10.3322/canjclin.20.1.105005751 [Google Scholar] [CrossRef] [PubMed]
[4]. Manrique RD, Deive LG, Uehara MA, Manrique RK, Rodriguez JL, Santidrian C, Maxillary sinus cancer review in 23 patients treated with postoperative radiotherapyActa Otorrinolaringol Esp 2008 59(1):06-10.10.1016/S0001-6519(08)73250-3 [Google Scholar] [CrossRef]
[5]. Waldron JN, O’Sullivan B, Gullane P, Witterick IJ, Liu FF, Payne D, Carcinoma of the maxillary antrum: a retrospective analysis of 110 casesRadiother Oncol 2000 57(2):167-73.10.1016/S0167-8140(00)00256-5 [Google Scholar] [CrossRef]
[6]. Le QT, Fu KK, Kaplan M, Terris DJ, Fee WE, Goffinet DR, Treatment of maxillary sinus carcinoma: comparison of the 1997 and 1977 American Joint Committee on cancer staging systemsCancer 1999 86:1700-11.10.1002/(SICI)1097-0142(19991101)86:9<1700::AID-CNCR11>3.0.CO;2-4 [Google Scholar] [CrossRef]
[7]. Blanco AI, Chao KS, Ozyigit G, Adli M, Thorstad WL, Simpson JR, Carcinoma of paranasal sinuses: long-term outcomes with radiotherapyInt J Radiat Oncol Biol Phys 2004 59:51-58.10.1016/j.ijrobp.2003.09.10115093898 [Google Scholar] [CrossRef] [PubMed]
[8]. American Joint Committee on Cancer. In: Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, et al, editors. American Joint Committee on Cancer Staging Manual. Nasal cavity and Paranasal sinuses. 6th ed. Springer-Verlag: New York; 2002. pp. 59-6710.1007/978-1-4757-3656-4_6 [Google Scholar] [CrossRef]
[9]. St-Pierre S, Baker SR, Squamous cell carcinoma of the maxillary sinus: analysis of 66 casesHead Neck Surg 1983 65:508-13.10.1002/hed.2890050610 [Google Scholar] [CrossRef]
[10]. Inuyama Y, Fujii M, Tanaka J, Takaoka T, Hosoda H, Kohno N, Neoadjuvant chemotherapy in maxillary sinus carcinoma with cisplatinum and peplomycin intraarterial infusionAuris Nasus Larynx 1985 12:S249-54.10.1016/S0385-8146(85)80068-7 [Google Scholar] [CrossRef]
[11]. Kreppel M, Danscheid S, Scheer M, Lüers JC, Eich HT, Zöller JE, Neoadjuvant chemoradiation in squamous cell carcinoma of the maxillary sinus: a 26-year experienceChemotherapy Research and Practice 2012 2012:01-08.10.1155/2012/41358923056940 [Google Scholar] [CrossRef] [PubMed]
[12]. Ramalingam B, Ebenezer V, Retrospective analysis of survival of patients with squamous cell carcinoma of the maxilla after primary resection and elective bilateral neck dissection: an institutional experienceAnnals of Maxillofacial Surgery 2011 1(1):42-47.10.4103/2231-0746.8315523483114 [Google Scholar] [CrossRef] [PubMed]
[13]. Akhter M, Hossain S, Rahman QB, Molla MR, A study on histological grading of oral squamous cell carcinoma and its co-relationship with regional metastasisJ Oral Maxillofac Pathol 2011 15:168-76.10.4103/0973-029X.8448522529575 [Google Scholar] [CrossRef] [PubMed]
[14]. Dulguerov P, Jacobsen MS, Allal AS, Lehmann W, Calcaterra T, Nasal and paranasal sinus carcinoma: are we making progress? A series of 220 patients and a systematic reviewCancer 2001 92:3012-29.10.1002/1097-0142(20011215)92:12<3012::AID-CNCR10131>3.0.CO;2-E [Google Scholar] [CrossRef]
[15]. Sharma S, Sharma SC, Singhal S, Mehra YN, Gupta BD, Ghoshal S, Carcinoma of the maxillary antrum: a 10-year experienceInd J Otolaryngol 1991 43:191-194. [Google Scholar]
[16]. Amendola BE, Eisert D, Hazra TA, King ER, Carcinoma of the maxillary antrum: surgery of radiation therapy? Int J Radiat Oncol Biol Phys 1981 7(6):743-46.10.1016/0360-3016(81)90467-3 [Google Scholar] [CrossRef]
[17]. Jiang GL, Ang KK, Peters LJ, Wendt CD, Oswald MJ, Goepfert H, Maxillary sinus carcinomas: natural history and results of postoperative radiotherapyRadiother Oncol 1991 21(3):193-200.10.1016/0167-8140(91)90037-H [Google Scholar] [CrossRef]
[18]. Paulino AC, Fisher SG, Marks JE, Is prophylactic neck irradiation indicated in patients with squamous cell carcinoma of the maxillary sinus?Int J Radiat Oncol Biol Phys 1997 39(2):283-89.10.1016/S0360-3016(97)00293-9 [Google Scholar] [CrossRef]
[19]. Chen AM, Daly ME, El-Sayed I, Garcia J, Lee NY, Bucci MK, Patterns of failure after combined-modality approaches incorporating radiotherapy for sinonasal undifferentiated carcinoma of the head and neckInt J Radiat Oncol Biol Phys 2008 70(2):338-43.10.1016/j.ijrobp.2007.06.05718207030 [Google Scholar] [CrossRef] [PubMed]
[20]. Nigam J, Misra V, Dhingra V, Jain S, Varma K, Singh A, Comparative study of intra-operative cytology, frozen sections, and histology of tumor and tumor-like lesions of nose and paranasal sinusesJournal of Cytology 2013 30(1):13-17.10.4103/0970-9371.10750623661934 [Google Scholar] [CrossRef] [PubMed]
[21]. Fan KH, Wang HM, Kang CJ, Lee LY, Huang SF, Lin CY, Treatment results of postoperative radiotherapy on squamous cell carcinoma of the oral cavity: Coexistence of multiple minor risk factors results in higher recurrence ratesInt J Radiat Oncol Biol Phys 2010 77:1024-29.10.1016/j.ijrobp.2009.06.06420610038 [Google Scholar] [CrossRef] [PubMed]
[22]. Lin CY, Wang HM, Kang CJ, Lee LY, Huang SF, Fan KH, Primary tumor site as a predictor of treatment outcome for definitive radiotherapy of advanced-stage oral cavity cancersInt J Radiat Oncol Biol Phys 2010 78:1011-19.10.1016/j.ijrobp.2009.09.07420434273 [Google Scholar] [CrossRef] [PubMed]
[23]. Qureshi SS, Chaukar DA, Talole SD, D’Cruz AK, Squamous cell carcinoma of the maxillary sinus: a Tata Memorial Hospital experienceIndian J Cancer 2006 43:26-29.10.4103/0019-509X.2577216763359 [Google Scholar] [CrossRef] [PubMed]