A Swimmer in a Sea of Tumour
Aminder Singh1, Pavneet Kaur Selhi2, Neena Sood3, Manjot Kaur4
1 Assistant Professor, Department of Pathology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
2 Professor, Department of Pathology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
3 Professor and Head, Department of Pathology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
4 Resident, Department of Pathology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aminder Singh, Assistant Professor, Department of Pathology, Dayanand Medical College and Hospital, Tagore Nagar, Ludhiana-141001, Punjab, India.
E-mail: dramisingh@gmail.com
Carcinoma, Microfilaria, Parotid
Dear Editor,
Microfilaria is an endemic and major public health disease in Asia particularly in Eastern India and Africa. Microfilaria is rarely and accidently aspirated with Fine Needle Aspiration Cytology (FNAC) techniques [1]. Its been reported at number of sites both in fluid and tissue aspirates in literature but only a handful cases have been seen from parotid and being detected in mixed parotid gland tumour [2,3]. However, it is the first ever case, where microfilaria is being aspirated from malignant parotid gland carcinoma with lymph node metastasis. The presence of microfilaria along with neoplasms is considered to be an incidental finding. However, the possibility of parasites acting as triggering factors in carcinogenesis needs to be explored further.
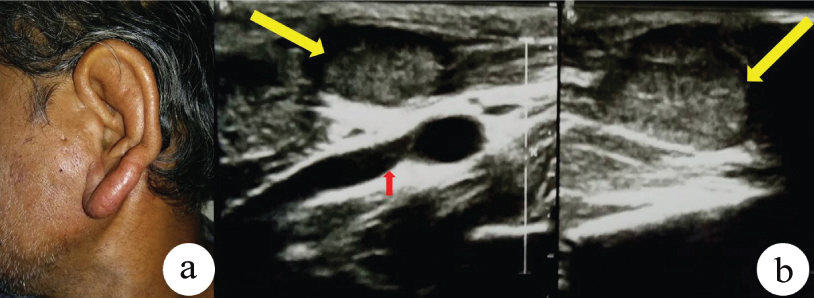
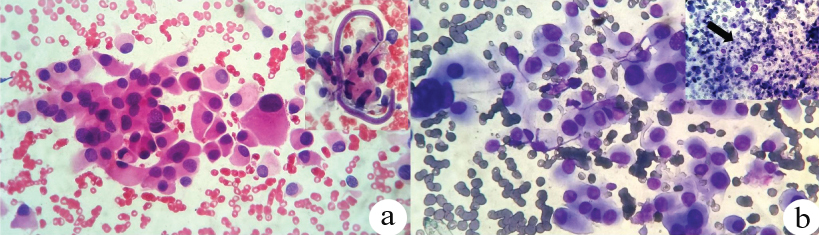
A previously healthy 63-year-old man presented with history of left parotid swelling for three months along with yellowish discharge left ear and oedematous earlobe for two days. No history of fever, loss of appetite, weight loss or any other significant comorbidities was present. Examination revealed firm, non mobile parotid swelling measured 4×3 cm along with subcutaneous oedema, left facial nerve palsy and lymphadenopathy [Table/Fig-1a]. Multiple nodular regions in left superficial lobe of parotid and multiple enlarged lymph nodes were evident on USG [Table/Fig-1b]. FNAC showed a cellular malignant tumour with plasmacytoid morphology with metastatic deposits in the adjoining lymph node [Table/Fig-2a]. Possibility of oncocytic type of salivary duct carcinoma was made. A solitary sheathed kinked microfilaria with overlapping irregular body nuclei reaching up to the tail, morphologically resembling Brugia malayi seen adherent to tumour cells [Table/Fig-2b] with inset. Further staging and histopathological confirmation of tumour could not be done as patient lost to follow up because of financial constrains.
a) Left parotid gland swelling with subcutaneous oedema of earlobe; b) Ultrasound images showed left enlarged parotid with coarse heterogeneous echotexture and lobulated lesion (yellow arrows). A large feeding vessel also appreciated (small red arrow).
a) The smear from left parotid mass showing cellular tumour with presence of Brugia malayi (inset) adherent to tumour cells (H&E, 400X); b) This cytopathological FNAC smear from left cervical lymph node demonstrates tumour cells with similar morphology as seen in parotid (Giemsa, 400X). Foci of necrosis also appreciated (Inset: black arrow; Giemsa, 200X).
Few authors believe that microfilaria can act as the triggering factor for the causation of neoplasm tough exact mechanism is not known. Probable hypothesis is that parasitic infestation leads to tumourigenesis by releasing certain cytokines or by causing chronic irritation at the site of infestation. Other probable explanations with neoplastic association are that microfilaria circulates in vasculature and lymphatic system and when neoplasms cause lymphovascular obstruction, the organisms appear in tissue fluid. In malignant tumours, increased blood flow and angiogenesis causes the increase deposition of microfilaria to these sites [4]. Accidental detection of microfilaria does not mean that it will be the only pathology in the lesion. But along with the management of neoplastic aetiology; its treatment is also required to prevent the further comorbidities associated with the disease. So, these patients should receive Hetrazan therapy prior to surgery.
[1]. Mondal S, Incidental detection of filaria in fine-needle aspirates: A cytologic study of 14 clinically unsuspected cases at different sitesDiagn Cytopathol 2012 40:292-96.10.1002/dc.2155722431316 [Google Scholar] [CrossRef] [PubMed]
[2]. Pantola C, Kala S, Agarwal A, Khan L, Microfilaria in cytological smears at rare sites coexisting with unusual pathology: A series of seven casesTrop Parasitol 2012 2:61-63.10.4103/2229-5070.9724423508347 [Google Scholar] [CrossRef] [PubMed]
[3]. Rama Devi K, Rajayalakshmi A, Nirmala V, Shravan O, Microfilaria in fine needle aspiration cytology smear of mixed parotid tumour - A case reportIndian J Mednod Allied Sciences 2015 3:40-42.10.5958/2347-6206.2015.00008.4 [Google Scholar] [CrossRef]
[4]. Gupta S, Sodhani P, Jain S, Kumar N, Microfilariae in association with neoplastic lesions: Report of five casesCytopathology 2001 12:120-26.10.1046/j.1365-2303.2001.00301.x11284956 [Google Scholar] [CrossRef] [PubMed]