A Rare Cause of Headache during Pregnancy
Fabiane Amaral Das Neves1, Filipa Raquel Pereira Nunes2, Maria Inês Marques Polónio3
1 Senior Resident, Department of Obstetrics B, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal.
2 Senior Resident, Department of Obstetrics B, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal.
3 Senior Doctor, Department of Obstetrics B, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Fabiane Amaral das Neves, Rua Francisco Lucas Pires, n65, 1B, 3030-489, Coimbra, Portugal.
E-mail: fabiane.am.neves@gmail.com
Aneurysmal Subarachnoid Hemorrhage (SAH) during pregnancy is an important cause of maternal and fetal morbidity and mortality. Controversies still exist related to its diagnostic and treatment approach. This article aims to call attention to the importance of early diagnosis and treatment of intracranial aneurysm during pregnancy, through, a case report of a 38-year-old female, 38 weeks 5 days pregnant, with essential Arterial Hypertension (AHT), treated with Nifedipine, was admitted to the emergency room after suffering a mild headache. She presented high blood pressure and moderate proteinuria. She was also submitted to cranial-cephalic MRI, showing SAH and angio-MRI, confirming cerebral aneurysm of the right middle artery. Immediately afterwards, the patient underwent emergency cesarean section and aneurysm clipping.
Intracranial aneurysm, Pre-eclampsia, Subarachnoid hemorrhage
Case Report
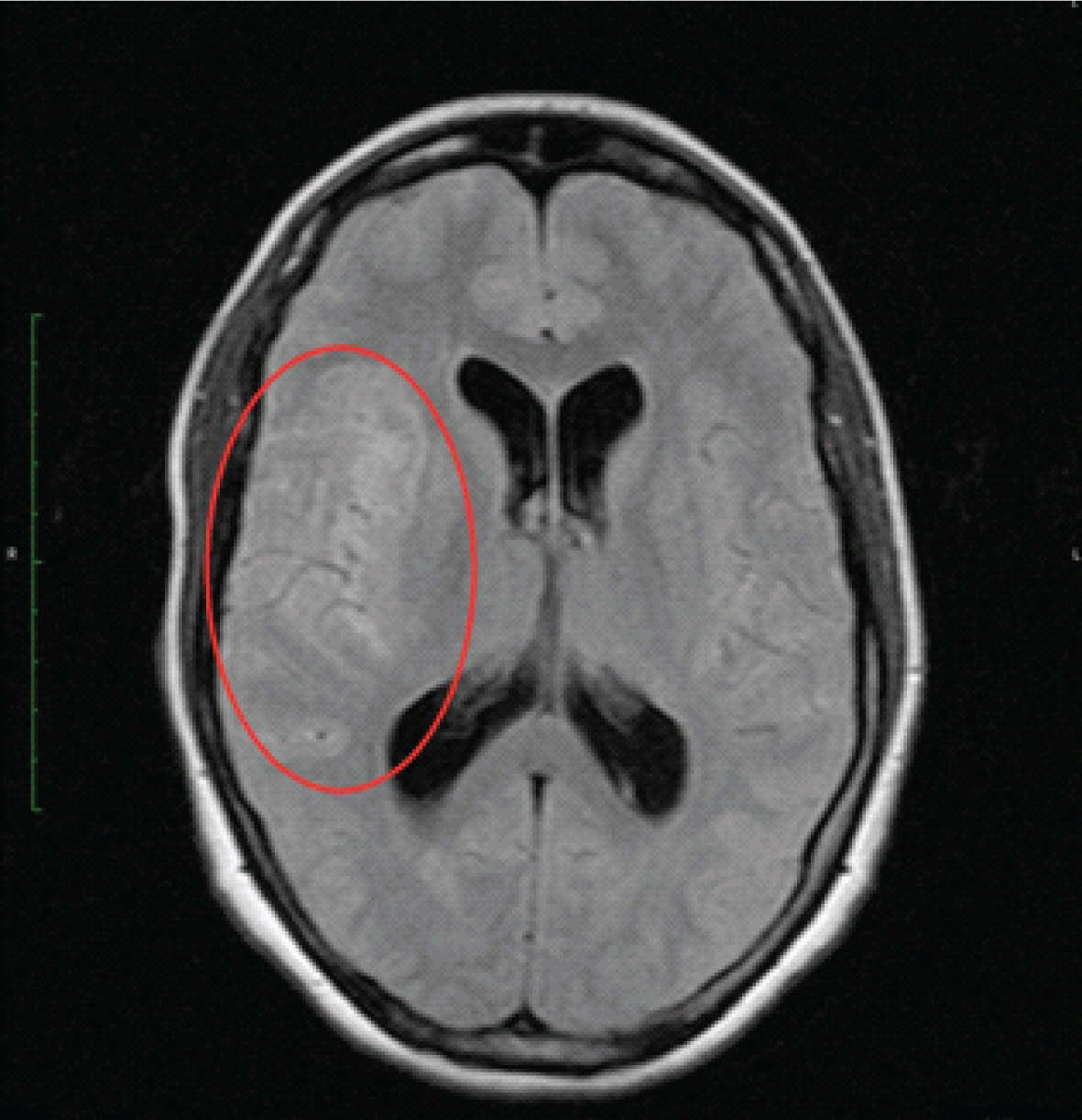
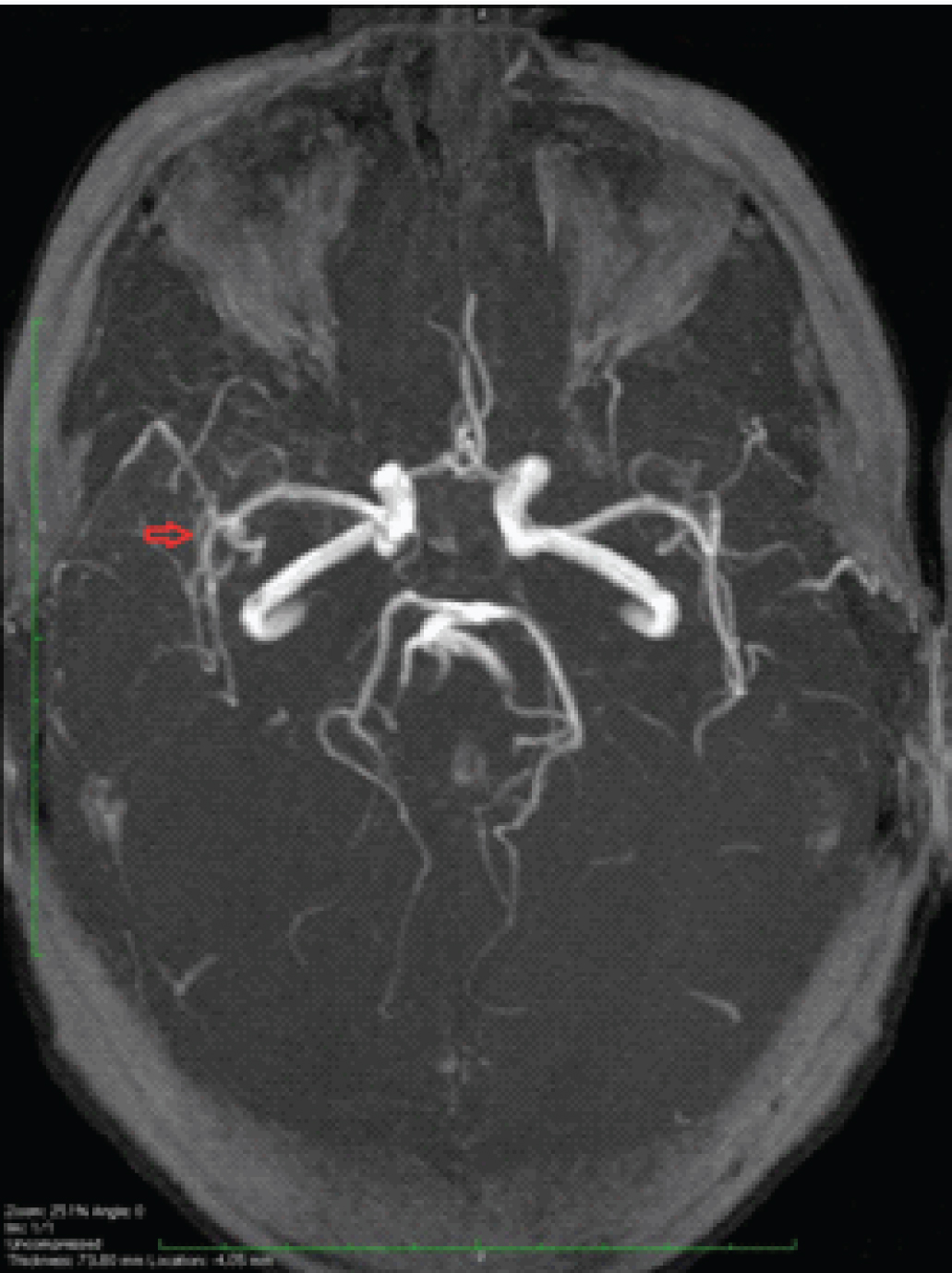
A female patient, 38-year-old, 38 weeks and 5 days pregnant, veterinarian, GIIIPI (vaginal birth at full term six years ago, prostaglandin-induced labour due to pre-eclampsia, without other complications), with chronic arterial hypertension, receiving Nifedipine (screened for secondary causes of AHT since the age of 19), was admitted to the emergency room due to faint spell followed by moderate occipital headache and vomiting. There was no personal or family history of headache, blood clotting or thromboembolic events. She denied smoking or drinking. Axillary temperature was recorded at 36.5°C, and blood pressure was 143/95 mmHg. The urine test strip showed protein (2+ dipstick), so an analytical analysis was conducted, but without changes (total protein test measured normal levels at the given gestational age). Physical examination showed odema up to the ankles. The patient was hospitalised as pre-eclampsia was suspected. During the following eight hours, as the headaches, vomiting and related changes in conscious state did not improve, the patient was referred to Neurology. Submitted to the neurological Glasgow Coma Scale (GCS), she scored 15. There were no signs of focal deficit and fundoscopy showed no change. The electroencephalogram conducted did not reveal any significant changes either. The brain MRI [Table/Fig-1] highlighted SAH mostly on the right Sylvian fissure and also by the basal cistern and the posterior fossa, and small intra ventricular haemorrhagic areas. Diffuse sulcal effacement and discrete hydrocephalic expansion of the supratentorial ventricular system were also present. There were signal changes in the opercular parenchyma and the right insular cortex, namely in the diffusion images, translating extension to the cortical parenchyma of haemorrhagic areas and related ischemic areas, the latter possibly caused by vasospasm due to the rupturing of an aneurysm. The angio-MRI study [Table/Fig-2] was completed, hereby confirming aneurysm of the right M1 segment of the middle cerebral artery. After diagnosing SAH due to rupturing of an aneurysm, the pregnant patient was submitted to emergency cesarean section under general anaesthesia because it was easier to control of blood pressure so as to balance the risk of re-bleed and the risk of cerebral and placental hypoperfusion. She gave birth to a healthy newborn weighing 3.190 g with APGAR score of 9 at one minute after birth and 10 at five minutes after birth. Aneurysm clipping and intraparenchymal Intracranial Pressure (ICP), sensor implant procedure were performed immediately afterwards. The patient remained in the ICU under sedation for 16 days, at first with mechanical ventilation and then spontaneous breathing. She completed 15 days of antibiotic therapy (Amikacin and Levofloxacin) due to nosocomial lung infection, and stayed for another ten days in the neurosurgical ward until she was discharged without focal deficit. About one years after surgery the patient was still free of focal deficit.
T2 sequence (Dark Blood) heterogeneous area is identified with sulcal effacement in topography corresponding to the Sylvian fissure.
TOF sequence: small aneurysmatic expansion of the right M1 segment of the middle cerebral artery.
Discussion
Subarachnoid Hemorrhage caused by cerebral aneurysm seldom occurs during pregnancy and is described in literature through case reports [1]. The average reported rate of SAH during pregnancy and puerperium ranges between 8 and 31 per 100,000 deliveries. Some suggest that the risk of SAH during pregnancy, birth or puerperium is higher than at other times [2]. Mortality rates are close to 50%, as is the neurological morbidity of survivors [3].
A pregnant woman with blood pressure elevation, proteinuria and headache is often diagnosed with pre-eclampsia/eclampsia, while less common diagnoses like cerebral aneurysm complications are hardly ever addressed, which can result in negative outcomes and high maternal and/or foetal morbidity and mortality [4].
Risk factors of stroke during pregnancy may or may not be linked to pregnancy related causes [5]. The factors which are not directly linked to pregnancy are the same as those of the general population, hypertension, smoking, coagulopathies, cardiovascular diseases, etc., Pregnancy related factors were reported by Bateman and include advanced maternal age, black race, hypertension, pre-eclampsia/eclampsia, pre-existing coagulopathy and smoking [6].
The symptoms of ruptured aneurysm are always acute: loss of consciousness (44%), correlated with rapid increase of ICP, light to severe headache, manifestations of meningeal irritation, convulsions, paralysis of cranial nerves and even coma. Hypertension, nausea and vomiting may be transitory [1,3]. Vitreous (pre-retinal) Hemorrhage with SAH combined is called Terson Syndrome and implies an even worse prognosis. This case should raise our awareness of headache in pregnancy; although it is a frequent symptom and even if it is not severe/incapacitating, it can be associated with a serious condition, especially if there are risk factors of vascular complications, such as hypertension. In this case the clinical sign was frustration at first and not the typical acute and intense headache of SAH.
An emergency physical examination must assess patient’s state of awareness, meningeal signs, paralysis of the cranial nerves or focal deficit.
The diagnosis of SAH involves a high level of suspicion and several neuroimaging studies. Computed Tomography (CT) scanning without contrast is the most relevant diagnostic test (greater sensitivity in the first 6-12 hours after Hemorrhage and only 58% on the 5th day) [7]. Lumbar puncture should be performed when initial CT findings are negative. Limited data suggests that cranio encephalic magnetic resonance can be as sensitive as a CT in detecting SAH and, in some cases, it is more sensitive in sub-acute conditions (>4 days of Hemorrhage). In several reported cases of aneurysmal SAH, cesarean section is the most consensual approach before surgical treatment or intravascular embolisation [4,8,9]. An emergency cesarean section followed by aneurysmal treatment (Clipping) was our strategy in this case. In addition, in these patients, the risk of experiencing a Hemorrhage increases over time [8]. Deciding on the type of anaesthesia during surgery can also be difficult and must be discussed on an individual basis, according to the anaesthetist’s experience. The rate of complications is higher with general anaesthesia than local regional anaesthesia in pregnant women [10]. We opted for general anaesthesia because it was easier to control blood pressure so as to balance the risk of re-bleed and the risk of cerebral and placental hypoperfusion.
The level of suspicion of a neurological entity is important for the rapid referral of the case by a multidisciplinary team, thus containing obstetric and neurological complications for the pregnant woman.
Conclusion
SAH as a result of rupture of an intracranial aneurysm is a serious complication in pregnancy and it can lead to morbidity and mortality during pregnancy. General principles of management are the same as for non pregnant individuals with special focus on control of blood pressure so as to balance the risk of re-bleed and the risk of cerebral and placental hypoperfusion. Considering the threat that brain aneurysm poses to both mother and child, all obstetricians must be suspicious of it when a pregnant woman calls in with signs of acute headache, specially in parallel with neurological signs. Addressing such cases with a multidisciplinary team is paramount.
[1]. Roman H, Descargues G, Lopes M, Emery E, Clavier E, Diguet A, Subarachnoid Hemorrhage due to cerebral aneurysmal rupture during pregnancyActa Obstet Gynecol Scand 2004 83:330-34.10.1111/j.0001-6349.2004.00281.x15005778 [Google Scholar] [CrossRef] [PubMed]
[2]. Groenestege A, Rinkel G, Van der Bom J, Algra A, Klijn C, The risk of aneurysmal subarachnoid Hemorrhage during pregnancy, delivery, and the puerperium in the utrecht populatio. case-crossover study and standardized incidence ratio estimationStroke 2009 40(4):1148-51.10.1161/STROKEAHA.108.53970019211489 [Google Scholar] [CrossRef] [PubMed]
[3]. Fairhall JM, Stoodley MA, Intracranial Hemorrhage in pregnancyObstetric Medicine 2009 2(4):142-48.10.1258/om.2009.09003027579059 [Google Scholar] [CrossRef] [PubMed]
[4]. Kocak A, Ates O, Cayli SR, Sarac K, Pregnant woman with subarachnoid Hemorrhage and multiple intracranial aneurysms: A case reportTurkish Neurosurgery 2006 16(2):100-04. [Google Scholar]
[5]. Khan M, Wasay M, Haemorrhagic strokes in pregnancy and puerperiumInternational Journal of Stroke 2013 8:265-72.10.1111/j.1747-4949.2012.00853.x22863273 [Google Scholar] [CrossRef] [PubMed]
[6]. Bateman BT, Olbrecht VA, Berman MF, Minehart Rd, Schwamm LH, Leffert LR, Peripartum subarachnoid Hemorrhage. Nationwide data and institutional experienceAnaesthesiology 2012 116(2):324-33.10.1097/ALN.0b013e3182410b2222166951 [Google Scholar] [CrossRef] [PubMed]
[7]. Perry J, Stiell G, Sivilotti L, Bullard J, Symington C, Worster A, Sensitivity of computed tomography performed within six hours of onset of headache for diagnosis of subarachnoid Hemorrhage: prospective cohort studyBMJ 2011 343:d427710.1136/bmj.d427721768192 [Google Scholar] [CrossRef] [PubMed]
[8]. Chen J, Wang Y, Li P, Chen W, Zhou J, Hu X, Treatment of a giant arteriovenous malformation associated with intracranial aneurysm rupture during pregnancy: A case reportExperimental and Therapeutic Medicine 2016 12:1337-40.10.3892/etm.2016.350527588055 [Google Scholar] [CrossRef] [PubMed]
[9]. Kim K, Chang C, Choi B, Jung Y, Endovascular treatment of a ruptured posterior inferior cerebellar artery aneurysm during pregnancyJ Korean Neurosurg Soc 2014 55(5):273-76.10.3340/jkns.2014.55.5.27325132934 [Google Scholar] [CrossRef] [PubMed]
[10]. Carvalho L, Vilas Boas W, Anaesthetic conduct in cesarean section in a parturient with unruptured intracranial aneurysmRevista Brazilian J Aneshph 2009 59(6):746-50.10.1016/S0034-7094(09)70100-X [Google Scholar] [CrossRef]