Importance of Mycologic Evaluation in Chronic Non Healing Ulcers
Vivek Hada1, Anuradha Sharma2, Vijaya Lakshmi Nag3, Kushwant Singh Rathore4
1 Senior Resident, Department of Microbiology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
2 Associate Professor, Department of Microbiology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
3 Professor and Head, Department of Microbiology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
4 Senior Resident, Department of Orthopaedics, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anuradha Sharma, Associate Professor, Department of Microbiology, All India Institute of Medical Sciences, Jodhpur-342005, Rajasthan, India.
E-mail: asharma3170@gmail.com
Chronic non healing ulcers are caused by various aetiologies ranging from infections, autoimmune disorders to neoplasms. Fungal infections are important yet neglected cause of non healing ulcers. In most of these instances there is a history of direct inoculation due to minor trauma. Presence of immuno-compromised state is an important risk factor. In this case report, we are discussing a case of 48-year-old immunocompetent female patient, who had undergone local debridement at a rural hospital about eight months back on her left foot, later she developed a chronic non healing ulcer at the site. Chronic non healing ulcers should always be investigated for bacterial as well as fungal aetiologies despite patient’s normal immune status to prevent misuse of antibiotics along with prolonged disability of the patient.
Candida, Diabetes, Fusarium, Lower limb, Trauma
Case Report
A 48-year-old female from the rural western Rajasthan visited OPD with the complaint of chronic non healing ulcer on dorsum of third toe of the left foot for last seven to eight months. The ulcer developed following incision and drainage of a localised swelling, which was performed by an unregistered medical professional in the village. The ulcer gradually increased in size with the development of new lesions around the ulcer. Subsequently, there was restriction in movement of foot with difficulty in walking and pain during movement of the foot. Local debridement of wound was performed several times by the same practitioner. There was no history of diabetes, smoking, corticosteroids intake or any cardiovascular disease.
On examination, size of the ulcer was approximately 7×3 cm and it involved dorsum of left foot starting from third toe. The surface of ulcer was wet with friable mass of granulation tissue. The proximal margin of ulcer had signs of cellulitis with a zone of erythema surrounding the lesion. There was presence of 2-3 bullae proximal to the ulcer and largest of them was 2.5 cm in diameter. Bullae were filled with the serous discharge [Table/Fig-1]. There was no foul odour from the lesion and base of the ulcer was vascular with a bleeding tendency. There were no signs of neurovascular compromise.
The chronic ulcer with friable base and adjoining bullae before starting the antifungal treatment.

On investigation, patient’s fasting and postprandial blood glucose level were within normal limits and she was non-reactive for HIV serology. X-Ray of the foot did not reveal any bony involvement due to lesion. The tissue from ulcer base was sent for histopathology examination which showed presence of chronic granulation tissue comprising predominantly of plasma cells, lymphocytes along with proliferating capillary channels. No cells of malignant nature were seen. After ruling out non-infectious causes like neoplasm, vascular compromise and diabetes, patient was evaluated for infective aetiology.
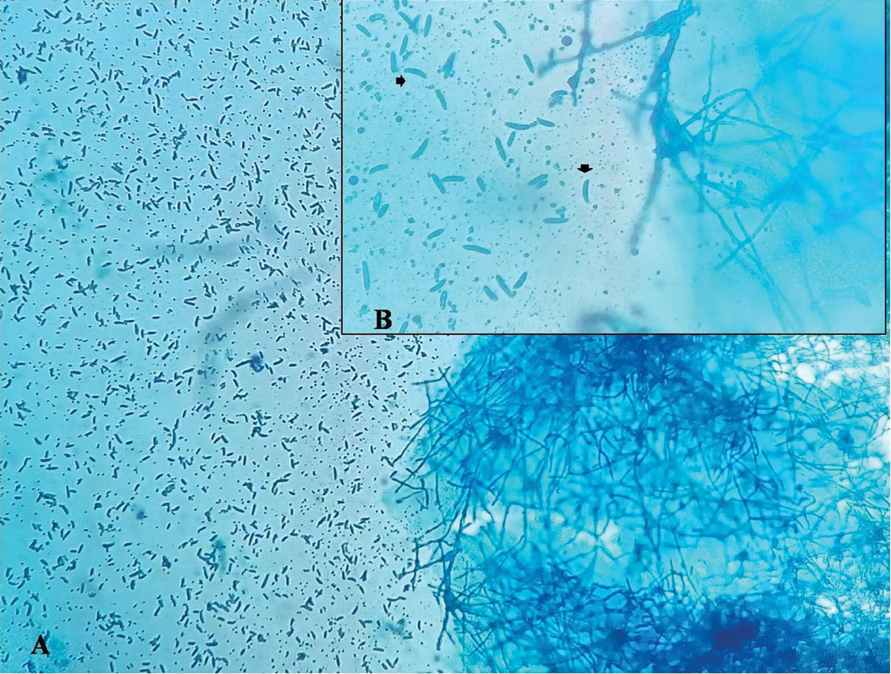
Initially specimen was collected from the ulcer base by means of sterile swab and it was sent for aerobic bacterial culture and gram staining. On Gram stain, many inflammatory cells were seen along with lightly stained gram positive filamentous structures raising suspicion of fungal aetiology. The punch biopsy was collected after cleaning and debridement of the wound to confirm the fungal elements. A 20% KOH mount from tissue revealed hyaline, septate fungal hyphae [Table/Fig-2]. Biopsy sample was inoculated on Sabouraud’s Dextrose agar and incubated at 25°C. After five days of incubation, white filamentous growth was obtained having cottony surface. There was no obvious pigment on the reverse side of the growth. Along with it; a few creamy white coloured colonies were also isolated. Lactophenol Cotton Blue mount of the filamentous growth showed hyaline septate hyphae 3-8 μm in diameter along with abundance of canoe-shaped, multi-celled macroconidia and one or two-celled hyaline microconidia [Table/Fig-3]. The isolate was identified as Fusarium spp. on basis of microscopic findings. There were few white creamy colonies on culture which on gram staining showed budding yeast cells. These were identified as Candida albicans on the basis of positive Germ tube test and light green coloured colony on CHROM agar. Patient was initially advised oral voriconazole but she was not able to afford the drug due to cost constraints. Thus, she was advised topical application of Miconazole ointment along with oral Fluconazole (150 mg) once daily for 1 month. On subsequent visit after ten days, there was gross decrease in size of the ulcer with shrinking of erythematous area [Table/Fig-4]. The margins of ulcer showed gradual epithelisation [Table/Fig-5]. The patient continued to respond to the antifungal treatment.
The KOH mount of the specimen showing septate hyaline hyphae (40X magnification).
Lacto Phenol Cotton Blue mount (A-10X and B-40X magnification) showing hyaline septate hyphae along with multicelled canoe shaped macroconidia.
Decrease in size of ulcer and healing of bullae after one month of antifungal treatment.

Further reduction in size of ulcer with initiation of healing process after 45 days of treatment.

Discussion
Chronic lower limb ulcers area relatively common condition. They are considered as chronic if a wound fails to heal even after 3 months of adequate treatment or not fully healed after 12 months. They are mostly caused by vascular abnormalities, mostly venous insufficiency, followed by arterial diseases and mixed aetiology. Almost 5% of leg ulcers results from less common pathophysiological causes, and this latter group comprise considerable challenges in diagnosis, assessment, and management [1]. Almost 0.6-3% of elderly over the age of 60 years suffers from this condition and it increases up to 5% in people over 80 years. Prevalence of chronic leg ulcer in the community ranges from 1.9% to 13.1% [2]. Among various aetiologies fungi constitute an uncommon cause of chronic ulcer [3]. This could be one of the reasons that in our case the specimen was not sent for fungal culture initially. But visualisation of filamentous fungal hyphae like structure prompted for fungal culture.
Fungi are emerging as important causative agents of chronic lower limb ulcers especially in immunocompromised patients with malignancy, diabetes, chemotherapy, etc. Diagnosis of fungi as a causative aetiology is very important as most of the time there will be no obvious sign for suspecting them which was also seen in this case. Among various fungi, Fusarium species has now been reported as an important aetiological agent of chronic ulcer disease especially in diabetics [4,5].
Fusarium species is hyaline filamentous fungi associated with disseminated infections in immunocompromised patients, with a high mortality rate of 50-80% [6,7]. In immunocompetent individuals, it has been associated with localised infection of skin and/ or subcutaneous tissue and also rarely causes mycotoxicosis [7,8]. In their review Nucci M and Anaissie E concluded that history of trauma, break in skin or inoculation injury is invariably present in immunocompetent individuals who have ulcers associated with Fusarium spp. and it is present in upto 70% of cases. Sometimes duration between injury and presentation to clinic could be up to 1 year [8]. Similar history was seen in our case where patient had undergone treatment for small abscess followed by there was development of chronic non healing ulcer.
One of the important sources for infection with Fusarium spp. could be water supply in health care unit. Anaissie EJ et al., during their study were able to isolate Fusarium spp. from 162 (57%) water samples in the hospital. Thus, any person with skin breakdown should avoid exposure to environmental sources of Fusarium spp. including tap water [9]. This could be an important source of infection especially in case of improper wound management techniques.
Schulte DM et al., during their prospective study found that use of broad spectrum antimicrobial is independent risk factor associated with risk of colonisation of Candida spp. in patients even at the time of hospitalisation [10]. Repeated isolation of Candida albicans along with Fusarium spp. in our case could be due to super added infection following multiple courses of broad spectrum antibiotics. Culture of biopsy specimen is important for isolation and identification of fungi in these cases because of differences in their susceptibility to antifungal agents. Fusarium solanii is the most common species to be isolated from clinical specimens and shows decreased susceptibility to many antifungal drugs including amphotericin B in vitro susceptibility tests [11]. Newer triazole agents like itraconazole, voriconazole and posaconazole have good antifungal activity against Fusarium spp. but local debridement and topical antifungal agents (e.g., Natamycin & Amphotericin B) are also adequate [8]. In present case also patient responded to local antifungal treatment along with oral fluconazole, with significant decrease in size of ulcer within one month.
Conclusion
This case highlights the importance of keeping in mind the possible role of fungal pathogens in chronic ulcers of limb. Also, early and thorough investigations in these cases not only help in achieving correct diagnosis but also prevent misuse of antibiotics.
[1]. Rayner R, Carville K, Keaton J, Prentice J, Santamaria N, Leg ulcers: atypical presentations and associated comorbiditiesWound Pract Res 2009 17(4):168-85. [Google Scholar]
[2]. Agale SV, Vinayak S, Chronic leg ulcers: epidemiology, aetiopathogenesis, and managementUlcers 2013 :1-9.10.1155/2013/413604 [Google Scholar] [CrossRef]
[3]. Kahle B, Hermanns H-J, Gallenkemper G, Evidence-based treatment of chronic leg ulcersDtsch Arztebl Int 2011 108:231-37.10.3238/arztebl.2011.023121547162 [Google Scholar] [CrossRef] [PubMed]
[4]. Dutta P, Premkumar A, Chakrabarti A, Shah VN, Behera A, De D, Fusarium falciforme Infection of Foot in a Patient with Type 2 Diabetes Mellitus: A Case Report and Review of the LiteratureMycopathologia 2013 176:225-32.10.1007/s11046-013-9646-z23813152 [Google Scholar] [CrossRef] [PubMed]
[5]. Nucci M, Anaissie E, Fusarium infections in immunocompromised patientsClin Microbiol Rev 2007 20:695-704.10.1128/CMR.00014-0717934079 [Google Scholar] [CrossRef] [PubMed]
[6]. Pai R, Boloor R, Shreevidya K, Shenoy D, Fusarium solani: an emerging fungus in chronic diabetic ulcerJ Lab Physicians 2010 2:37-39.10.4103/0974-2727.6671021814405 [Google Scholar] [CrossRef] [PubMed]
[7]. Nelson PE, Dignani MC, Anaissie EJ, Taxonomy, biology, and clinical aspects of Fusarium speciesClin Microbiol Rev 1994 7:479-504.10.1128/CMR.7.4.4797834602 [Google Scholar] [CrossRef] [PubMed]
[8]. Nucci M, Anaissie E, Cutaneous infection by fusarium species in healthy and immunocompromised hosts: implications for diagnosis and managementClin Infect Dis 2002 35:909-20.10.1086/34232812355377 [Google Scholar] [CrossRef] [PubMed]
[9]. Anaissie EJ, Kuchar RT, Rex JH, Francesconi A, Kasai M, Müller FM, Fusariosis associated with pathogenic fusarium species colonization of a hospital water system: a new paradigm for the epidemiology of opportunistic mold infectionsClin Infect Dis 2001 33:1871-78.10.1086/32450111692299 [Google Scholar] [CrossRef] [PubMed]
[10]. Schulte DM, Sethi A, Gangnon R, Duster M, Maki DG, Safdar N, Risk factors for Candida colonization and Co-colonization with multi-drug resistant organisms at admissionAntimicrob Resist Infect Control 2015 4:4610.1186/s13756-015-0089-926568822 [Google Scholar] [CrossRef] [PubMed]
[11]. Tortorano AM, Richardson M, Roilides E, van Diepeningen A, Caira M, Munoz P, European Society of Clinical Microbiology and Infectious Diseases Fungal Infection Study Group; European Confederation of Medical Mycology. ESCMID and ECMM joint guidelines on diagnosis and management of hyalohyphomycosis: Fusarium spp., Scedosporium spp. and othersClin Microbiol Infect 2014 20(Suppl 3):27-46.10.1111/1469-0691.1246524548001 [Google Scholar] [CrossRef] [PubMed]