Onychomycosis by Trichosporon Inkin: A Rare Clinical Entity
Charu Jain1, Ravinder Kaur2, Deepti Rawat3, Suraiya K Ansari4
1 Senior Resident, Department of Microbiology, Lady Hardinge Medical College and Associated Hospitals, Delhi, India.
2 Director Professor and Head, Department of Microbiology, Lady Hardinge Medical College and Associated Hospitals, Delhi, India.
3 Assistant Professor, Department of Microbiology, Lady Hardinge Medical College and Associated Hospitals, Delhi, India.
4 Senior Resident, Department of Microbiology, Lady Hardinge Medical College and Associated Hospitals, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ravinder Kaur, 275, Ground Floor, Gagan Vihar Main, Delhi-110051, India.
E-mail: doccharujain@gmail.com
Trichosporon species are basidiomycetous yeasts that are widely distributed in the nature and regularly found on normal skin. The cylinder-shaped arthroconidia forming yeast has undergone a major taxonomic reclassification with Trichosporon inkin associated with white piedra of hair shafts. Here in we report a rare case of onychomycosis in an otherwise healthy adult.
Appressoria, Blastoconidia, Sarcinae
Case Report
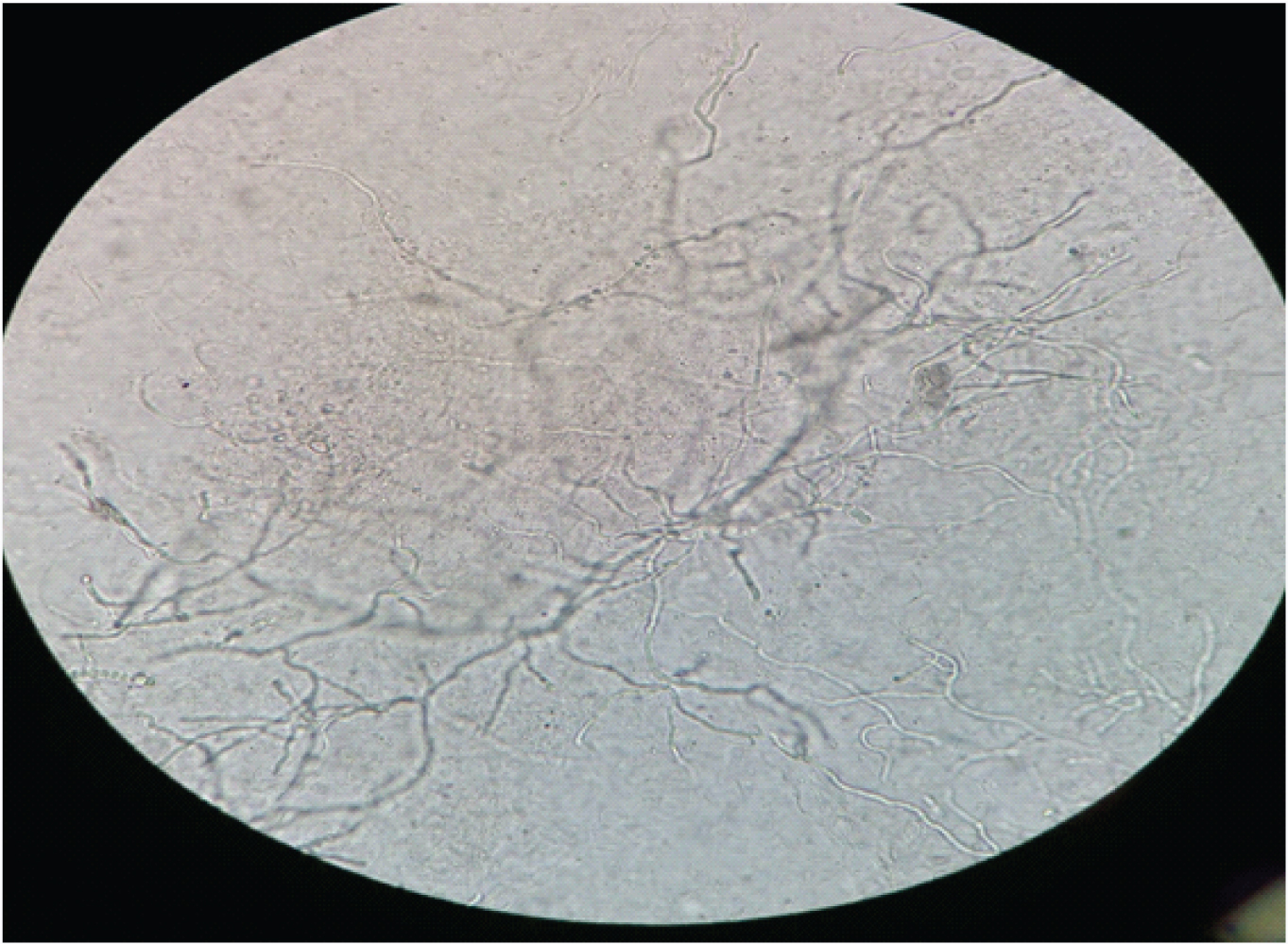
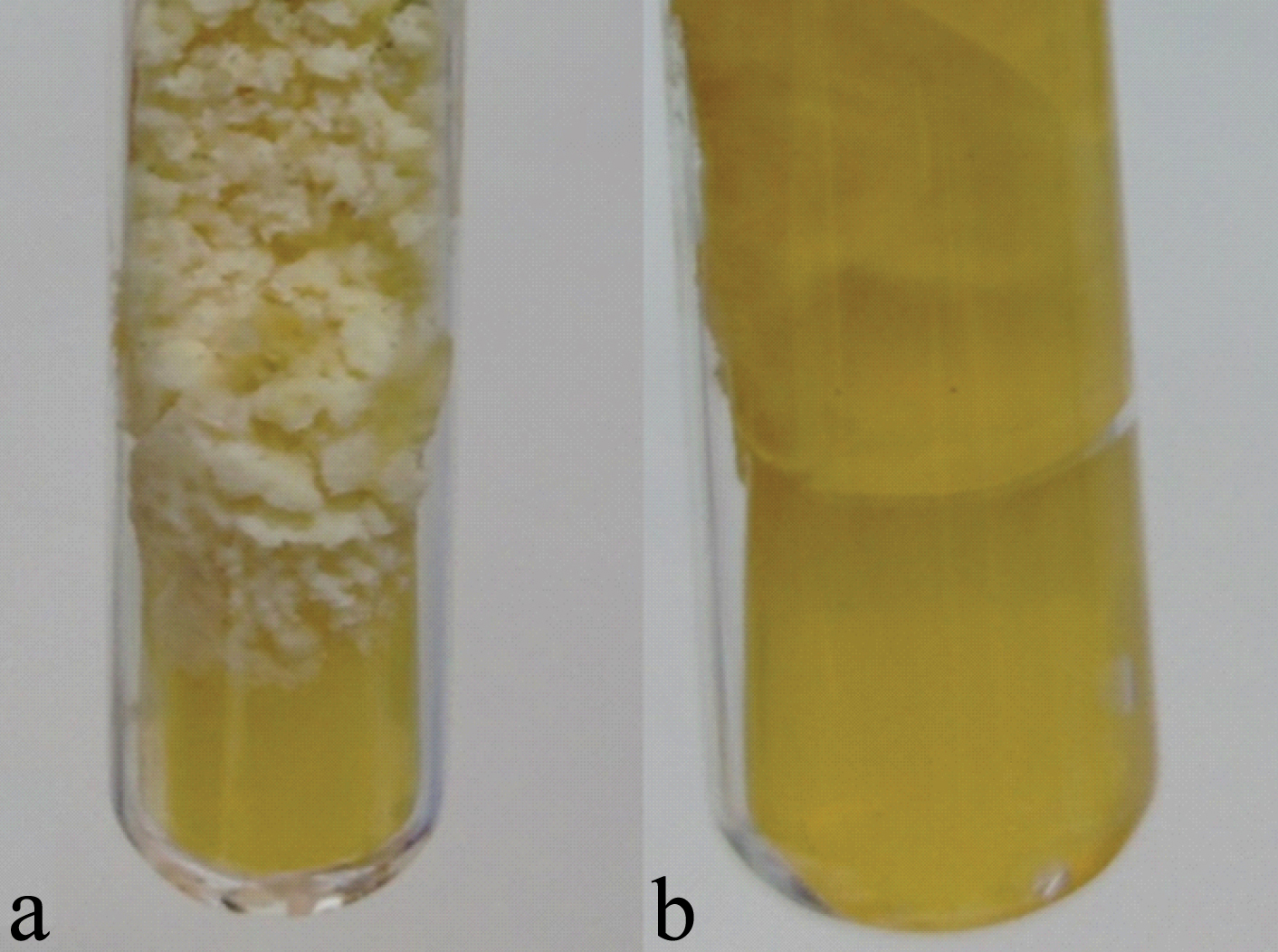
A 26-year-old female presented to Dermatology OPD with complaints of discolouration of fingernails along with change in texture of nails [Table/Fig-1]. As per the patient, the problem had started in the right hand thumb and index finger nail which gradually spread to other nails of same hand. As her symptoms progressed, she decided to take a consultation from a private physician. She was prescribed some medication for application (no document available). Two months later she presented to the dermatology department of our tertiary care hospital for further evaluation and treatment. On examination, yellowish discolouration along with thickening of fingernails was observed [Table/Fig-1]. Scalp, hair and genital region were free from any fungal infection. General physical examination revealed no other pathological abnormality. There was no history of chronic illness. Nail scraping from both hands were taken using sterile precautions for fungal microscopy and culture. Initial mycological examination on 20% KOH microscopy revealed hyaline hyphae with round blastoconidia and arthroconidia [Table/Fig-2]. Sample was further cultured on Sabouraud’s dextrose agar with Gentamycin, Chloramphenicol and Cycloheximide at 26°C and 37°C, respectively. After seven days of aerobic incubation at 26°C, a white, finely cerebriform growth was obtained. On further incubation, colour of the growth darkened along with cracking of agar [Table/Fig-3a,b]. The identification of the isolate was done using microscopic and biochemical characteristics (sugar assimilation, urease production) of the yeast grown at 26°C for 5-10 days on Corn meal agar using standard microbiological tests [1].
Discoloured and brittle thumb nail of patient on clinical presentation.

A 20% KOH mount of nail scraping showing hyaline hyphae.
Macroscopic characteristics of the isolate grown aerobically on SDA at 26oC: a) restricted, white, finely cerebriform growth on SDA; b) Reverse cracking of media.
Microscopically long cylindrical arthroconidia, blastoconidia, sarcinae and appressoria were observed [Table/Fig-4]. Urease test was positive. Myo-inositol was assimilated whereas melibiose was not. Afterwards a repeat sample obtained grew the same organism again, which was preliminarily identified as Trichosporon species. Based on the microscopic, macroscopic and biochemical characteristics, the isolate was identified as Trichosporon inkin; since no other Trichosporon species form sarcinae and appressoria. The patient was started on Itraconazole therapy (200 mg OD) for six weeks and is under follow up.
LPCB mount of isolate (at 40X) showing: Arthroconidia a), Appressoria b) and Sarcinae c).

Discussion
Onychomycosis is a common nail condition characterised by thickening and associated dystrophy. Symptoms range from cosmetic concern to painful experiences which hamper day to day activity. The fungal involvement in nail comprises of yeast as well as moulds [2].
Predisposing risk factors usually associated are exposure to water, misuse of antibiotics as well as derangement of immune status due to chronic diseases or immunosuppressive therapy [2].
Trichosporon species have been associated with superficial and systemic infections. Previously thought to be a contaminant in fungal culture, it is now being viewed as a pathogen of significance [3].
Recent changes in the taxonomy has expanded the genus members with six major human pathogens: T asahii, T. mucoides, T. ovoides, T. asteroides, T. cutaneum, and T. inkin [3].
Role of Trichosporon species as etiological agent of onychomycosis have been reported in recent studies [4].
In nail disorders, T. ovoides and T. cutaneum has been identified in different studies as the most commonly isolated member of Trichosporon genus [4].
T. inkin is commonly associated with white piedra of hair shafts in genital region [1]. This species has been reported from a variety of invasive infections in immunocompromised patients of haematological malignancies, peritoneal dialysis, endocarditis etc., [1,2].
Conventional laboratory methods for identification of species include colony morphology, biochemical test, slide culture or corn meal agar, sugar assimilation test and cycloheximide tolerance test [1].
Newer molecular methodologies for confirmation like sequencing of Intergenic spacer 1 region of the rRNA gene family are upcoming but they are currently available only at selected reference laboratory. Therefore, as of now, commonly performed test may provide a direction for identification [5].
As per best of our knowledge, only one other nail infection by T. inkin has been reported from a patient from Mexico with history of chronic ulcer and trauma [6].
The isolation of same agent from both the hand sample on dual occasion, gives strength to the assumption of T. inkin as a potential nail pathogen rather than just being a secondary colonizer.
As the susceptibility profile for antifungal vary according to the species, it is necessary to identify the isolate up to species level. This will help in epidemiological association of species to a clinical condition and thus help in guiding the therapy [7].
Similar to other studies, the infection here is also seen in a female. The possible reason could be constant damage to nail due to household work which can act as a predisposing risk factor [4,6].
T. inkin reports from India are limited to cases of white piedra of scalp and allergic fungal sinusitis [7,8].
Conclusion
T. inkin should be considered a potential pathogen in onychomycosis. Also, the emergence of Trichosporon species warrants more efforts for correct and timely identification. More data needs to be collected to form a knowledge base for both superficial and deep infections.
[1]. Hoogs GS, Guarro J, Gene J, Figueras MJ, In: Atlas of clinical fungiAmer Society for Microbio 2000 2th ed:1126 [Google Scholar]
[2]. Chabasse D, Pihet M, Mycological diagnosis of onychomycosisJ Mycol Med 2014 24(4):269-78.10.1016/j.mycmed.2014.10.00625458363 [Google Scholar] [CrossRef] [PubMed]
[3]. Mariné M, Brown NA, Riaño-Pachón DM, Goldman GH, On and under the skin: emerging basidiomycetous yeast infections caused by trichosporon speciesPLoS Pathog 2015 11(7):e100498210.1371/journal.ppat.100498226226483 [Google Scholar] [CrossRef] [PubMed]
[4]. Magalhães AR, Nishikawa MM, Mondino SS, Macedo HW, Rocha EM, Baptista AR, Trichosporon isolation from human ungueal infections: is there a pathogenic role?An Bras Dermatol 2016 91(2):173-79.10.1590/abd1806-4841.2016463227192516 [Google Scholar] [CrossRef] [PubMed]
[5]. Rastogi V, Honnavar P, Rudramurthy SM, Pamidi U, Ghosh A, Chakrabarti A, Molecular characterisation and antifungal susceptibility of clinical Trichosporon isolates in IndiaMycoses 2016 59(8):528-34.10.1111/myc.1251127144725 [Google Scholar] [CrossRef] [PubMed]
[6]. Ortega-Springall MF, Arroyo-Escalante S, Arenas R, Onycholysis and chromonychia: a case caused by trichosporon inkinSkin Appendage Disord 2016 1(3):144-46.10.1159/00044106527171745 [Google Scholar] [CrossRef] [PubMed]
[7]. de Almeida Júnior JN, Hennequin C, Invasive trichosporon infection: a systematic review on a re-emerging fungal pathogenFront Microbiol 2016 7:162910.3389/fmicb.2016.0162927799926 [Google Scholar] [CrossRef] [PubMed]
[8]. Shivaprakash MR, Singh G, Gupta P, Dhaliwal M, Kanwar AJ, Chakrabarti A, Extensive white piedra of the scalp caused by Trichosporon inkin: a case report and review of literatureMycopathologia 2011 172(6):481-86.10.1007/s11046-011-9454-221833760 [Google Scholar] [CrossRef] [PubMed]