Introduction
Person-Centred Care (PCC) relies on effective communication and emphasises on co-operation in care between patients and healthcare professionals. WHO advocates this type of care as a key component of quality health care.
Aim
To evaluate if person-centred nursing can improve treatment regimen adherence in patients with Myocardial Infarction (MI).
Materials and Methods
During August-November 2016, 101 patients with MI, of age ≤85 years were randomly assigned to person-centred nursing group and usual care group and followed for two months. In the intervention group, a person-centred nursing process was added to care, emphasising the patient as a partner in care. Care was provided in co-operation with the patient, registered nurse and researcher. Data were collected using self-report adherence to the treatment regimen questionnaire and were analysed using SPSS software version 22 and chi-square test, independent samples t-test and paired t-test were applied wherever required.
Results
Study results showed that the mean score of treatment regimen adherence did not have a significant difference before intervention, three weeks and two month after intervention in control group (p=0.692; p=0.581), but three weeks after intervention, the intervention group had a significant difference in the mean score of the treatment regimen adherence (p<0.001). Also, paired t-test results showed that two month after intervention the mean of adherence in person-centred nursing group was higher than control group (p<0.001).
Conclusion
Person-centered nursing improved treatment regimen adherence in patients with MI. Further work is needed to examine whether this intervention can be sustained to improve clinical outcomes.
Medication adherence, Medication non adherence, Nursing care plans, Nursing theories, Quality of care
Introduction
The quality of care that is provided to a person in the health system is dependent on the three elements of structure, process and results. The structure represents the physical environment, the process represents interactions of nurses and patients and results reflect the state of health care during discharge [1]. Quality health care is also described as accountability, respect, punctuality and confidence of staff. That is, a more PCC will provide high-quality care because its focus is not on task completion but personal customisation [2]. Nowadays, PCC and related concepts, such as patient involvement and patient participation, are receiving more attention [3].
PCC emphasises a partnership in care between patients and healthcare professionals and is advocated by WHO as a key component of quality health care [4]. In PCC, the emphasis is placed on recognising the patient as a human being with reason, will, feelings, and need, and on engaging the patient as an active partner in his/her care and treatment [5]. The most important part in PCC is the partnership between the patient and the therapist and to formulate a health plan together with the patient which includes both short-and long-term goals along with the actions needed to reach each goal [6].
The PCC concept has a long history in health care, so that the root of this concept can be found in the theory of Florence Nightingale [2]. The term ‘person-centered’ is widely used globally in health and social care [7].
Recent research into person-centeredness has attempted to clarify the meaning of the term, explore its implications in practice and determine the cultural and contextual challenges to implementing a person-centered approach [1]. Person-centeredness can be described as having three dimensions: staff attitudes and commitment, the environment and care processes in settings [8].
Non adherence to treatment is an important cause of increased cardiovascular disease, a risk of disability, morbidity and mortality rates and rising health care costs [9].
In Iran, several studies using methods such as self-promotion, continuous care model, continuous care model and telenursing, has been done to improve medication adherence which have been effective. However, the problem of poor adherence to the treatment regimen in people with heart disease still remains [10-12].
We, therefore, provided PCC in patients with MI to evaluate whether it has any effect on medication adherence.
Materials and Methods
In the present clinical trial, we included 101 MI patients admitted to the cardiac intensive care unit of hospitals affiliated with the Shahid Beheshti University of Medical Sciences, Tehran, Iran, from August 2016 to December 2016. The Clinical Trials registration number is IRCT2017022232730N1. Sampling was performed with the purposive sampling method based on inclusion criteria and using statistical methods to determine the sample size difference between the mean and variance in similar studies. Sampling formula used to calculate the sample size was:
Type I error probability=> = 0.05 → = 1.96 and power of test=>1 − = 0.8 → = 0.84
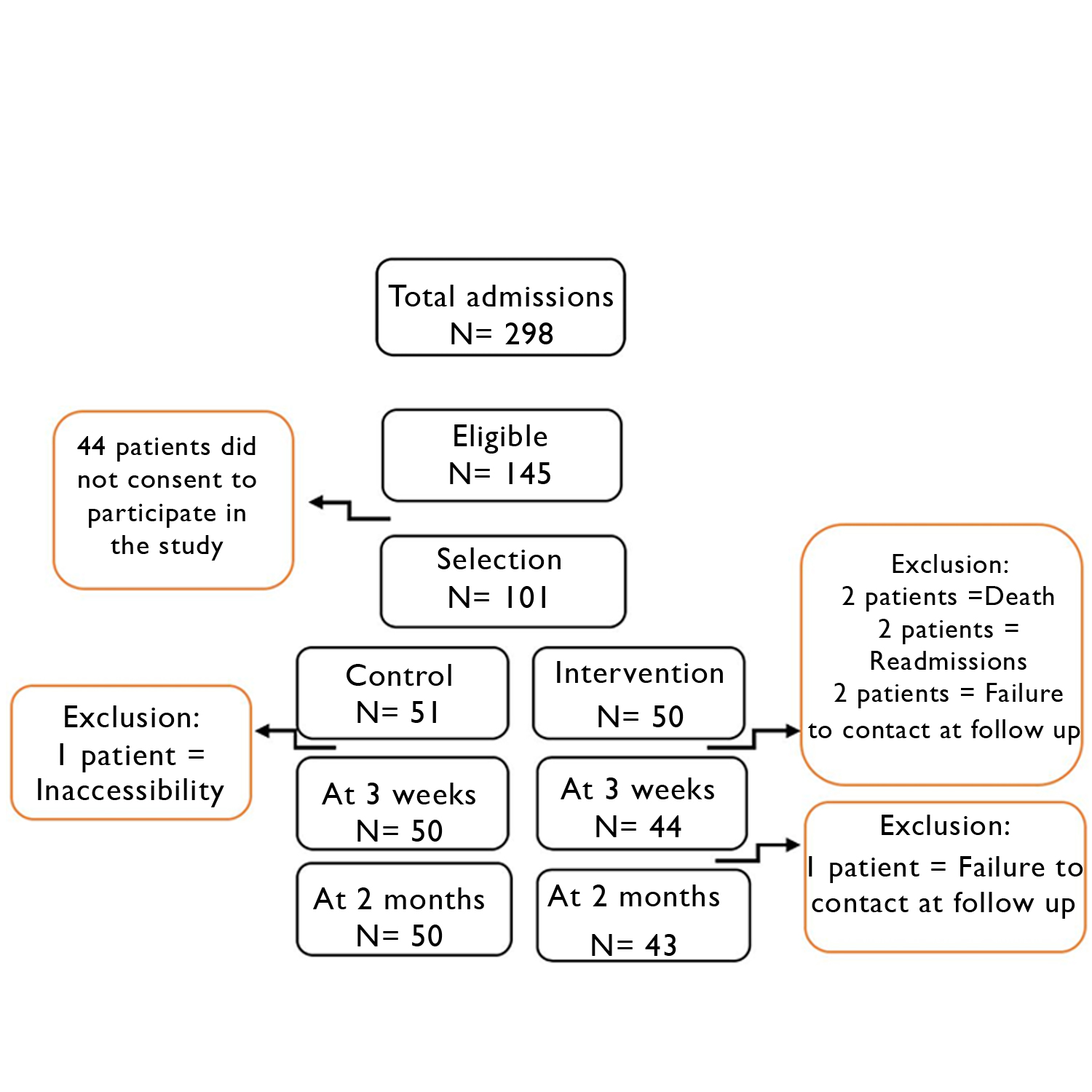
According to the results of Baljani E et al., [10] and Fors A et al., [13] studies, standard deviation in the population was considered 1.6. So, the sample size calculated was 44 patients in each group. Expected effect size considered between 10-15% and sample size in each group was increased to 50 patients [Table/Fig-1].
Inclusion criteria: MI patients hospitalised for at least 72 hours in the intensive care unit. Patients who had the ability to communicate verbally. Patients who did not have cognitive and vision impairment.
Exclusion criteria: Patients who had a recurrent heart attack during the study. Patients who did not wish to participate in the study.
Data Collection
A questionnaire was used for data collection of adherence to treatment, designed by Kamrani F et al., Before use of the questionnaire, the researcher had requested for permission and was granted. The language of the questionnaire was Persian [12].
The questionnaire was divided into two parts; the first part was about demographic data (gender, age, job, etc.) and the second part focussed on dimensions of the adherence to treatment regimen (including diet, medication and exercise). The diet section consisted of 33 questions about the types of food and patient’s eating habits which was rated using a five point Likert scale (never, rarely, sometimes, often or always). The score for each person in this field can range from 0 to 132. The domain of exercise consisted of 14 questions about a person’s exercise pattern. The individual’s response to questions was scored from 0-4. The score for each person in this field could range from 0 to 56. Domain of medication included nine questions regarding patient medication usage pattern. The individual’s response to the questions was scored with a score of 0 and 1. The final score for each person was at least 0 and at the most 9. The final score of the questionnaire, which indicated the degree of compliance with the treatment regimen, was obtained from the total score of the specified areas, and had a minimum score of 0 and a maximum of 197. The highest score indicated adherence to the treatment regimen as favourable. Adherence to the treatment regimen was classified into three categories. The range from 0 to 60 was placed in the poor adherence, the range from 61 to 120 was placed in the medium adherence and good adherence ranged from 121 to 197.
Content Validity Index (CVI) of the instrument was determined by 10 faculty members of the Nursing and Midwifery Faculty of Shahid Beheshti University of Medical Sciences [diet (0.92), medication (0.95), and exercise (0.91)]. The reliability was approved by 20 independent MI patients [Cronbach’s alpha for diet (0.83), medication (0.75) and exercise (0.71)].
After obtaining signed informed consent, eligible patients were informed that they would be treated according to the usual care routines for MI at cardiac intensive care unit of hospitals. They were also asked to complete questionnaires at baseline and follow up (3 weeks and 2 months).
PCC Intervention
Session 1–Person-centred nursing: A nurse with a bachelor’s degree was selected from among the nurses working in each cardiac care unit. These nurses, as a research fellow, were trained during a training session on how to provide PCC. These nurses intervened only to help the researcher in providing care to the group. The training and supervision of the work of these nurses was carried out by the researcher. Within 24 hours after randomisation patients were asked about their expectations, preferences and outcome of treatment. The nurse obtained information about the daily life of the patient, the patient’s social situation, the ability to perform daily tasks and severity of disease symptoms. The nurses respected the usual procedures of the patients and the patient himself set the hours of sleep and awakening. The patient would be free to study or write memories. Patient privacy was respected during all procedures. The nurse was present at the bedside to speak at any hour of the day if the patient requests. In addition, every nurse responded to questions from the patient in a tone of kindness using simple and understandable language. In addition to the above mentioned proceeding, the progress of the treatment and the improvement direction of the patient was expressed.
Session 2–Educational session: The aim of session 2 was to increase the patient’s knowledge regarding diet, physical activity, and medications. Training was provided both verbally and in writing to patients. Necessary training including some knowledge regarding heart attacks, cardiovascular risk factors, nutrition, and dietary regimens, familiarity with cardiac medications and their method of usage, exercise, and physical activity was given to the patient. The doctrines were presented to the patients on the last day of admission. The validity of educational content was confirmed by five faculty members of the Faculty of Nursing and Midwifery and a nutritionist and necessary changes were made.
Session 3–Follow up and continued co-operation: Every week, at least two phone calls were established with the patient and a meeting was arranged at three weeks and two months in the hospital clinic. During the meeting, the questionnaire was completed by a nurse to assess the achievement of goals.
Results
The trial profile is shown in [Table/Fig-1]. In total, 298 patients with MI were admitted. Of 145 who met the eligibility criteria, 44 declined to participate. In total, 101 patients were included in the trial, 50 patients in the person centred nursing intervention and 51 in the usual care group. Patients in both groups were similar in all demographic and disease characteristics [Table/Fig-2].
Demographic data of patients in the two groups.
| Demographical characteristics | Intervention (N=50) | Control (N=51) | p-value |
|---|
| Gender (male/female) | 31/19 | 39/12 | 0.117 |
| Mean age in years (SD) | 50 (20) | 52 (45) | 0.773 |
| Marital status (%) |
| Unmarried | 3 (6) | 1 (2) | 0.357 |
| Married | 44 (88) | 46 (90) |
| Divorced/Separated/Widowed | 3 (6) | 4 (8) |
| Educational degree, n (%) |
| None | 10 (20) | 4 (8) | 0.121 |
| Primaryschool | 12 (24) | 14 (27) |
| Middleschool | 6 (12) | 13 (25) |
| Highschool | 12 (24) | 15 (29) |
| University | 10 (20) | 5 (10) |
| BMI, mean (SD) | 25.13 (4.06) | 24.63 (4.12) | 0.538 |
| Lipids level (mg/dL) |
| Mean score (SD) | | | |
| LDL | 104 (41) | 100 (65) | 0.688 |
In the intervention group, the scores of three fields of treatment regimen adherence and total score increased after three weeks. Therefore, significant difference was detected in the mean score of treatment regimen adherence before and after the intervention (p<0.001) [Table/Fig-3]. In comparison between three weeks and two months after discharge, both groups had a significant decrease. This issue can be justified given that after two months, the acute stages of the disease have passed and the importance of illness has been reduced for the patients. However, it can affect some factors such as the fatigue of drug therapy. This finding has not been seen in other studies and requires further studies focusing on this subject. Comparing these means using t-test showed a significant difference between the score means of adherence to treatment in three weeks after the intervention and two months after intervention (p<0.001) [Table/Fig-4].
Comparing scores of treatment regimen adherence in the two groups before and after intervention.
| | | Dietary Adherence | Medication Adherence | Adherence to physical activity | Adherence to treatment regimen |
|---|
| Control group | N=51 | Before intervention Mean (±SD) | 81.92 (14.72) | 4.82 (2.6) | 17.20 (4.34) | 105.08 |
| N=51 | 3 weeks after intervention Mean (±SD) | 82.72 (13.44) | 5.03 (2.12) | 17.26 (4.96) | 105.68 |
| p-value | 0.211 | 0.562 | 0.903 | 0.692 |
| N=50 | 2 months after intervention Mean (±SD) | 82.42 (14.90) | 4.03 (2.22) | 16.94 (4.84) | 103.92 |
| p-value | 0.824 | <0.001 | 0.151 | 0.581 |
| Intervention group | N=50 | Before intervention Mean (±SD) | 79.60 (13.31) | 4.67 (2.2) | 16.58 (5.10) | 103.44 |
| N=44 | 3 weeks after intervention Mean (±SD) | 101.36 (7.03) | 7.77 (1.03) | 26.98 (4.12) | 136.56 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 |
| N=43 | 2 months after intervention Mean (±SD) | 100.28 (9.66) | 6.45 (1.43) | 26.00 (3.59) | 133.73 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 |
Comparing scores of treatment regimen adherence in the two groups three weeks and two months after intervention.
| Variables | Control group | | Intervention group | |
|---|
| 3 weeks after intervention Mean (±SD) | 2 months after intervention Mean (±SD) | p-value | 3 weeks after intervention Mean (±SD) | 2 months after intervention Mean (±SD) | p-value |
|---|
| Dietary Adherence | 82.72 (13.44) | 82.42 (14.90) | 0.882 | 101.36 (7.03) | 100.28 (9.66) | 0.221 |
| Medication Adherence | 5.03 (2.12) | 4.03 (2.22) | 0.000 | 7.77 (1.03) | 6.45 (1.43) | <0.001 |
| Adherence to physical activity | 17.26 (4.96) | 16.94 (4.84) | 0.436 | 26.98 (4.12) | 26.00 (3.59) | 0.004 |
| Adherence to treatment regimen | 105.68 (16.08) | 103.92 (17.89) | 0.454 | 136.56 (10.07) | 133.73 (12.82) | <0.001 |
Discussion
Findings from this study showed that the score of treatment regimen adherence in both groups before the intervention did not differ statistically. Three weeks after the intervention with PCC in the intervention group all three fields of adherence to treatment increased significantly but after two months the adherence to treatment in all three fields had decreased slightly but was not significant statistically. The reason behind slight decline seems that, the patients have passed through the acute phase of the disease which reduced the importance of the issue among them. In the control group the adherence to the treatment regimen did not significantly change over time.
The number of studies in the field of PCC is low. Our findings are consistent with the findings of the Fors A et al., [13] and Ekman I et al., [5] studies. Fors A et al., concluded in their study that PCC leads to improved self efficacy in patients with acute coronary syndrome and Ekman I et al., concluded that this care leads to improved quality of life and daily activities in patients with heart failure. Given that in this study we had weekly telephonic follow up for intervention group it can be said our findings are consistent with the results of Kamrani’s F et al., [12]. In the study by Kamrani F et al., telephone follow up group, showed a better compliance with the diet therapy compared to the control group and the non trained group.
Adherence to treatment is a complex behaviour, can be influenced by health beliefs, attitudes and expectations. Around 50% of patients in high-income countries do not obey their diet regimen. This statistic has been reported to be more than 50% in countries with low and medium income. Poor adherence to the treatment regimen is a serious risk for effectiveness of treatment and this is a vital issue in the field of public health, quality of life and economic health [14]. Adherence to treatment is a mulitfaceted phenomenon. Intervention with PCC seems to have a good effect on treatment adherence in the present study, so that not only patients but also healthcare workers, especially nurses play a vital role in changing the health behaviour of the patients.
Limitation
In PCC, all health personnel should be included based on person-centered principles, while in this study only nurses participated.
Conclusion
Due to the effectiveness of person-centered nursing, the healthcare providers may play an important role in improving medication adherence in patients with MI. PCC is provided by the nurses which is useful for the hospitalised patients as well as the patients at home. In addition, we can achieve the goal of treatment adherence using a combination of internal cognitive and external social supports and by developing meaningful patient perceptions regarding the value of medication adherence.
[1]. McCormack B, McCance TV, Development of a framework for person-centred nursingJournal of Advanced Nursing 2006 56(5):472-79.10.1111/j.1365-2648.2006.04042.x17078823 [Google Scholar] [CrossRef] [PubMed]
[2]. Morgan S, Yoder LH, A concept analysis of person-centered careJournal of Holistic Nursing 2012 30(1):6-15.10.1177/089801011141218921772048 [Google Scholar] [CrossRef] [PubMed]
[3]. Entwistle VA, Watt IS, Treating patients as persons: a capabilities approach to support delivery of person-centered careThe American Journal of Bioethics 2013 13(8):29-39.10.1080/15265161.2013.80206023862598 [Google Scholar] [CrossRef] [PubMed]
[4]. Ekman I, Wolf A, Olsson LE, Taft C, Dudas K, Schaufelberger M, Effects of person-centred care in patients with chronic heart failure: the PCC-HF studyEuropean Heart Journal 2012 33(9):1112-19.10.1093/eurheartj/ehr30621926072 [Google Scholar] [CrossRef] [PubMed]
[5]. Ekman I, Swedberg K, Taft C, Lindseth A, Norberg A, Brink E, Person-centered care—ready for prime timeEuropean Journal of Cardiovascular Nursing 2011 10(4):248-51.10.1016/j.ejcnurse.2011.06.00821764386 [Google Scholar] [CrossRef] [PubMed]
[6]. Lotzke H, Jakobsson M, Brisby H, Gutke A, Hägg O, Smeets R, Use of the PREPARE (PREhabilitation, Physical Activity and exeRcisE) program to improve outcomes after lumbar fusion surgery for severe low back pain: a study protocol of a person-centred randomised controlled trialBMC Musculoskeletal Disorders 2016 17(1):34910.1186/s12891-016-1203-827538757 [Google Scholar] [CrossRef] [PubMed]
[7]. McCance T, McCormack B, Dewing J, An exploration of person-centredness in practiceJournal of Issues in Nursing 2011 16(2):1 [Google Scholar]
[8]. McCormack B, Dewing J, McCance T, Developing person-centred care: addressing contextual challenges through practice developmentOnline J Issues Nurs 2011 16(2):3 [Google Scholar]
[9]. Lip GY, Laroche C, Popescu MI, Rasmussen LH, Vitali-Serdoz L, Dan GA, Improved outcomes with European Society of Cardiology guideline-adherent antithrombotic treatment in high-risk patients with atrial fibrillation: a report from the EORP-AF General Pilot RegistryEuropace 2015 17(12):1777-86.10.1093/europace/euv26926321406 [Google Scholar] [CrossRef] [PubMed]
[10]. Baljani E, Rahimi J, Heidary S, Azimpour A, Effects of self-management intervention on medication adherence and lifestyle in patients with coronary heart diseaseScientific Journal of Hamadan Nursing & Midwifery 2012 20(3):58-67. [Google Scholar]
[11]. Molazem Z, Rezaei S, Mohebbi Z, Ostovan MA, Keshavarzi S, Effect of continuous care model on lifestyle of patients with myocardial infarctionARYA atherosclerosis 2013 9(3):186 [Google Scholar]
[12]. Kamrani F, Nikkhah S, Borhani F, Jalali M, Shahsavari S, Nirumand-Zandi K, The effect of patient education and nurse-led telephone follow-up (telenursing) on adherence to treatment in patients with acute coronary syndromeCardiovascular Nursing Journal 2015 4(3):16-24. [Google Scholar]
[13]. Fors A, Ekman I, Taft C, Björkelund C, Frid K, Larsson ME, Person-centred care after acute coronary syndrome, from hospital to primary care—A randomised controlled trialInternational Journal of Cardiology 2015 187:693-99.10.1016/j.ijcard.2015.03.33625919754 [Google Scholar] [CrossRef] [PubMed]
[14]. Viswanathan M, Golin CE, Jones CD, Ashok M, Blalock SJ, Wines RC, Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic reviewAnnals of Internal Medicine 2012 157(11):785-95.10.7326/0003-4819-157-11-201212040-0053822964778 [Google Scholar] [CrossRef] [PubMed]