In India, many goddesses are worshipped as the symbol of power, wealth and blessing; but in reality most women are treated as trivial beings. Women are vulnerable not only because of enormous physiological variations experienced throughout their life but also because of the complexity of relation with the society. Depressive disorders evolve because of these complex biopsychosocial factors.
Overall, depression is the most common psychiatric disorder in the general population [1]. Globally, independent studies on depression show that women are twice as likely as men to suffer from clinical depression [2]. The lifetime prevalence of major depressive disorder is 10–25% for women, and 5–12% for men, in the world [3]. Work and home responsibilities, caring for children and ageing parents, abuse, and poverty may trigger a depressive episode in women, besides stressful life events [4]. Their toil on almost all the days of a year without any sick leave or casual leave makes them even more susceptible. Yet, mental health in women is conceived chiefly in terms of reproductive health, and other areas get little consideration [5].
The effects of depression extend beyond the individual patient, with negative impact on patients spouses and children [6,7]. It is also described as an important cause of premature mortality either from physical disorders or from suicides [8]. Universally, attempted suicides are around three times higher among women than men, especially among those suffering from depression [9].
Depression is the most common mental health condition in patients seeking primary care [10,11]. However, unless directly asked about their mood, patients omit information about depressive symptoms for a variety of reasons like fear of stigmatisation, issues of confidentiality and misconceptions related to the disease. In the absence of screening, it is estimated that only 50% of patients with major depression are identified [12,13].
Empirical knowledge of regional prevalence is fundamental to understanding the relative demand for services and to identify most appropriate avenues for intervention and health policy development. Also, understanding the socio-demographic determinants gives us a key to primary prevention.
Little is known about the status of the mental health morbidity of women residing in the urban areas of Uttarakhand. Therefore, this study was undertaken as an effort to find the burden of depression, to identify the related factors and also, to create awareness regarding various aspects of prevention and management of depressive disorders and reduce stigma, so that women confined in the four walls of their homes are able to get some ventilation and light.
Materials and Methods
The present cross-sectional study was conducted in urban field practice area of Government Medical College (GMC), Haldwani, District Nainital, Kumaon Region of Uttarakhand, India from June 2016 to May 2017. The field practice area is divided in four sectors with total population of 2637. This study was approved by the Institutional Ethics Committee.
Ever married women of age group 18-59 years residing in the area for more than six months and who gave written informed consent were included in the study. Women who were severely ill or intellectually disabled during the study and could not cooperate; had history of child birth within three months of interview and were pregnant at the time of data collection were excluded.
Sample size: Taking anticipated Prevalence (P) of depression as 24.9% (on the basis of study done in Kerala, India [14]) with 95% Confidence Interval and 5% precision, the sample size was estimated to be 276. Taking 15% non-response the final sample size was calculated as 320.
Study tool: Patient Health Questionnaire (PHQ)-9 Hindi for India version, freely available in public domain was used. The score of ≥10 were taken as possible depressive disorder (clinically significant depression) which has a sensitivity of 88% and a specificity of 88% for major depression. This scale can be administered by any trained person in the community, not necessarily a psychiatrist [15,16].
The women were asked about the listed symptoms being experienced in the past two weeks. The scale was administered by trained doctors posted at the urban health and training center of Department of Community Medicine, GMC, Haldwani, under the supervision of principal investigator. The training was done by one of the authors - working as a Psychiatrist at the associated tertiary care hospital of GMC, Haldwani.
Sampling and data collection: Population proportional to size method was used to determine the number of women to be interviewed from each of the four sectors described previously. Thereafter, individual households were selected by systematic random sampling. The purpose of the study was explained to the eligible women present in the selected households. If any household had more than one eligible woman, one woman was selected by draw method. If the women did not give consent for the study or if there were no eligible women in the selected household the adjacent household was taken and same process repeated until we had an eligible women consenting to participate in the study. In total, 324 women were interviewed. The data was collected using a pre-tested, semi-structured questionnaire along with the PHQ-9 scale administration. Effects of depression - able to perform daily activities (functionality) and presence of suicidal ideation - were also assessed. Privacy of participants and confidentiality of data was maintained at all stages of the study. The women who were screened positive for moderate to severe depression were referred to the Psychiatry Department, GMC, Haldwani, for further management.
Statistical Analysis
The data so collected was coded, entered and compiled in MS Excel, and tabulated and analysed using SPSS (version 17.0). Depression prevalence was calculated, and multivariate logistic regression was applied to assess associations between risk factors. The dependent variable (depression) was dichotomised. Univariate logistic regression analysis was performed using all relevant socioeconomic variables and variables with p-value <0.25 were considered in the multivariate logistic regression analysis. Chi-square test was used in analysis of functionality and suicidal ideation.
Results
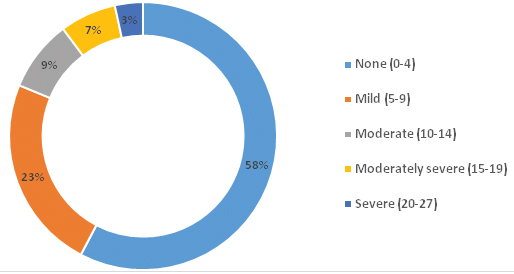
A total of 324 women agreed to participate in the present study. The doughnut-chart shows the severity of depression according to PHQ-9 scale [Table/Fig-1]. Clinically significant depression was present in 61 (18.8%) of the study subjects, out of which 11 (3.4%) had severe, 22 (6.8%) had moderately severe and 28 (8.6%) had moderate depression.
Doughnut-chart depicting the severity of depression (n=324).
The detailed socio-demographic and reproductive profile of the interviewed women along with the unadjusted and adjusted odds ratio of the variables studied is given in [Table/Fig-2].
Unadjusted and adjusted odds ratio for depression and socio-demographic and reproductive variables.
| S. No. | Variable | Frequency n (%) | Unadjusted odds ratio | Adjusted Odds Ratio |
|---|
| Odds ratio (95% CI) | p-value | Odds ratio (95% CI) | p-value |
|---|
| 1. | Women’s Age |
| <25 years | 27 (8.3) | 1 | | 1 | 0.741 |
| 25-34 years | 163 (50.3) | 0.446 (0.169 – 1.177) | 0.103 | 0.748 (0.158 – 3.544) | 0.714 |
| 35-44 years | 105 (32.4) | 0.989 (0.377 – 2.597) | 0.982 | 1.202 (0.203 – 7.122) | 0.839 |
| ≥45 years | 29 (9.0) | 0.457 (0.117 – 1.785) | 0.260 | 0.611 (0.075 – 4.991) | 0.646 |
| 2. | Age difference with husband |
| 0-3 years | 46 (14.2) | 1 | | -- | -- |
| 4-6 years | 155 (47.8) | 0.867 (0.375 – 2.006) | 0.739 |
| 7-9 years | 80 (24.7) | 0.798 (0.312 – 2.042) | 0.637 |
| ≥10 years | 43 (13.3) | 1.413 (0.520 – 3.841) | 0.498 |
| 3. | Women’s Education |
| Illiterate and Primary | 88 (27.2) | 1 | | 1 | 0.499 |
| Middle and Sec./Sen. Sec. | 154 (53.7) | 0.433 (0.235 – 0.795) | 0.007 | 1.004 (0.370 – 2.727) | 0.993 |
| Graduate and Postgraduate | 82 (25.3) | 0.104 (0.035 – 0.313) | 0.000 | 0.385 (0.062 – 2.375) | 0.304 |
| 4. | Husband’s Education |
| Illiterate and Primary | 51 (15.7) | 1 | | 1 | 0.804 |
| Middle and Sec./Sen. Sec. | 174 (53.7) | 0.429 (0.216 – 0.854) | 0.016 | 0.708 (0.215 – 2.334) | 0.571 |
| Graduate and Postgraduate | 99 (30.6) | 0.183 (0.075 – 0.448) | 0.000 | 0.870 (0.154 – 4.923) | 0.875 |
| 5. | Religion |
| Hindu | 269 (83.0) | 1 | | 1 | |
| Others | 55 (15.7) | 3.271 (1.718 – 6.229) | 0.000 | 2.408 (0.795 – 7.297) | 0.120 |
| 6. | Type of family |
| Nuclear | 273 (84.3) | 1 | | 1 | |
| Joint | 51 (15.7) | 1.867 (0.935 – 3.730) | 0.077 | 4.003 (1.400 – 11.44) | 0.010 |
| 7. | Type of House |
| Pucca* | 294 (90.7) | 1 | | 1 | |
| Kuchha/Semipucca** | 30 (9.3) | 2.895 (1.296 – 6.464) | 0.010 | 0.589 (0.167 – 2.077) | 0.411 |
| 8. | Ownership of House |
| Self | 202 (62.3) | 1 | | -- | -- |
| Rented | 122 (37.7) | 1.338 (0.758 – 2.364) | 0.315 |
| 9. | Marital Status |
| Currently married | 307 (94.8) | | | 1 | |
| Widow/Separated | 17 (5.2) | 3.355 (1.222 – 9.213) | 0.019 | 1.759 (0.383 – 8.084) | 0.468 |
| 10. | Age at Marriage |
| <18 years | 57 (17.6) | 1 | | 1 | 0.076 |
| 18-20 years | 132 (40.7) | 0.306 (0.154 – 0.607) | 0.001 | 0.655 (0.219 – 1.959) | 0.449 |
| 21-23 years | 86 (26.5) | 0.103 (0.039 – 0.275) | 0.000 | 0.133 (0.031 – 0.574) | 0.007 |
| 24-26 years | 30 (9.3) | 0.153 (0.041 – 0.563) | 0.005 | 0.232 (0.232 – 2.294) | 0.212 |
| >26 years | 19 (5.9) | 0.258 (0.067 – 0.985) | 0.047 | 0.645 (0.645 – 5.952) | 0.699 |
| 11. | Duration of Marriage |
| ≤5 years | 65 (20.1) | 1 | | -- | -- |
| 6-10 years | 83 (25.6) | 0.996 (0.419 – 2.369) | 0.993 |
| 11-15 years | 68 (21.0) | 1.052 (0.428 – 2.586) | 0.912 |
| ≥16 years | 108 (33.3) | 1.328 (0.600 – 2.943) | 0.484 |
| 12. | Infertility |
| No | 308 (95.1) | 1 | | -- | -- |
| Primary | 10 (3.1) | 1.929 (0.484 – 7.690) | 0.352 |
| Secondary | 06 (1.9) | 0.900 (0.103 – 7.855) | 0.924 |
| 13. | Conceptions |
| 0 | 10 (3.1) | 1 | | | 0.099 |
| 1-2 | 52 (16.0) | 0.194 (0.036 – 1.058) | 0.058 | 0.039 (0.002 – 0.620) | 0.022 |
| 2-3 | 188 (58.0) | 0.461 (0.113 – 1.880) | 0.280 | 0.046 (0.004 – 0.554) | 0.015 |
| ≥4 | 74 (22.8) | 0.987 (0.234 – 4.173) | 0.986 | 0.046 (0.003 – 0.640) | 0.022 |
| 14. | Living Children |
| 0 | 12 (3.7) | 1 | | -- | -- |
| 1-2 | 210 (64.8) | 0.443 (0.113 – 1.738) | 0.253 |
| 3-4 | 102 (31.5) | 1.250 (0.316 – 4.940) | 0.750 |
| 15. | Living Male Children |
| 0 | 64 (19.8) | 1 | | | 0.582 |
| 1-2 | 239 (73.8) | 0.719 (0.356 – 1.451) | 0.357 | 1.746 (0.516 – 5.907) | 0.370 |
| 3-4 | 21 (6.5) | 3.566 (1.247 –10.200) | 0.018 | 2.450 (0.375 – 16.016) | 0.350 |
| 16. | Living Female Children |
| 0 | 101 (31.2) | 1 | | -- | -- |
| 1-2 | 203 (62.7) | 0.899 (0.485 – 1.668) | 0.736 |
| 3-4 | 20 (6.2) | 1.850 (0.629 – 5.440) | 0.264 |
| 17. | Substance abuse in family |
| Not present | 277 (85.5) | 1 | | 1 | |
| Present | 47 (14.5) | 3.378 (1.725 – 6.614) | 0.001 | 4.494 (1.467 – 13.76) | 0.009 |
| 18. | Perceived Economic stability |
| Present | 214 (66.0) | | | 1 | |
| Not present | 110 (34.0) | 6.988 (3.774 – 12.941) | 0.000 | 3.856 (1.581 – 9.401) | 0.003 |
| 19. | Family relations |
| Good | 291 (89.8) | 1 | | 1 | 0.016 |
| Problem with in-laws | 18 (5.6) | 4.743 (1.770 – 12.707) | 0.008 | 3.016 (0.617 – 14.747) | 0.173 |
| Problem with husband | 15 (4.6) | 16.304 (4.959 – 53.600) | 0.000 | 8.124 (1.715 – 38.476) | 0.008 |
| 20. | Reasons related to children |
| Nil / Infertility | 136 (42.0) | 1 | 0.500 | 1 | 0.021 |
| Health | 12 (3.7) | 1.743 (0.346 – 8.770) | 0.500 | 0.843 (0.020 – 34.756) | 0.928 |
| Education | 105 (32.4) | 3.325 (1.653 – 6.691) | 0.001 | 5.365 (1.850 – 15.555) | 0.002 |
| Job/Livelihood/Girl’s Marriage | 71 (21.9) | 2.535 (1.157 – 5.556) | 0.020 | 2.306 (0.699 – 7.615) | 0.170 |
| 21. | Disease in family |
| Nil | 232 (71.6) | 1 | | 1 | 0.184 |
| Self / husband | 47 (14.5) | 2.986 (1.496 – 5.960) | 0.002 | 3.374 (1.193 – 9.537) | 0.022 |
| Children | 10 (3.1) | 2.259 (0.558 – 9.136) | 0.253 | 4.757 (0.217 – 104.46) | 0.322 |
| Anyone relative | 19 (5.9) | 0.293 (0.038 – 2.261) | 0.239 | 0.587 (0.054 – 6.418) | 0.662 |
| More than one member | 16 (4.9) | 1.216 (0.330 – 4.479) | 0.769 | 1.547 (0.201 – 11.922) | 0.676 |
| 22. | Self-image |
| Satisfactory | 280 (86.4) | 1 | | 1 | 0.030 |
| Unsatisfactory-Less educated | 28 (8.6) | 3.471 (1.523 – 7.911) | 0.003 | 3.674 (1.015 – 13.295) | 0.047 |
| Unsatisfactory-unable to work | 16 (4.9) | 3.218 (1.113 – 9.308) | 0.025 | 6.400 (0.918 – 44.619) | 0.061 |
* Pucca: all structure built with bricks and concrete
**Kuchha/Semipucca: walls and/or roof and/or floor-not made of concrete
In [Table/Fig-2] unadjusted odds ratio demonstrates depression to be less prevalent in women of higher age group but the results were not significant. Women with age difference of more than ten years with their husbands were found to be more depressed. Occurrence of depression decreased significantly with increase in the level of education of both the women and her husband. Women of faith other than Hindus were significantly more depressed. Also, the burden of depression among women staying in semi-pucca or kuchha house and the ones who were widowed or separated was significantly high.
The unadjusted odds of presence of depression was observed to be significantly lower in ladies married after 18 years than those married before attaining majority. Another finding of the present study was that although number of conceptions and number of children did not significantly affect incidence of depression, depression was seen to increase significantly if the women had more than three male children [Table/Fig-2].
The [Table/Fig-2] also shows results of multivariable model adjusted for various covariates selected on the basis of pre-decided cut-off for unadjusted odds ratio. The Hosmer and Lemeshow test was found to be not significant for the model (Chi-square 7.839, df 8, Sig. 0.449). Even when adjusted for other variables, women living in joint families were found to be significantly more afflicted with depression. It was also observed that there was significantly lower odds incidence of depression among ladies who were married between 21 and 23 years than any other age and also in the ladies who conceived at least once in comparison to the women never conceived.
In both univariate and multivariate analysis, significantly higher odds of developing depression was seen in women who stayed in families with issues of substance abuse, economic instability, and family disputes with husband. It was observed that education of children and also concern about their future acted as a more important factor in development of depression instead of the health of children, rather health issues in self or husband were more significant predictors of depression. The odds of presence of depression was more in women who felt that they were less educated, likewise the women who felt that they should have been working, although the result was significant for the later only [Table/Fig-2].
More than half of the subjects with severe and moderately severe depression found it very difficult to carry out their daily routine work. The association between functionality / functional health level and depression was statistically significant [Table/Fig-3]. The presence of suicidal ideas increasedsignificantly with the increase in severity of depression [Table/Fig-4].
Distribution of functionality of women with severity of depression.
| Depression Severity | Daily Activities |
|---|
| Not difficult | Somewhat difficult | Very difficult | Extremely difficult | Total |
|---|
| None-minimal | 169 | 17 | 1 | 0 | 187 |
| (79.3%) | (21.0%) | (4.3%) | (0.0%) | (57.7%) |
| (90.4%) | (9.1%) | (0.5%) | (0.0%) | (100.0%) |
| Mild | 40 | 36 | 0 | 0 | 76 |
| (18.8%) | (44.4%) | (0.0%) | (0.0%) | (23.8%) |
| (52.6%) | (47.4%) | (0.0%) | (0.0%) | (100.0%) |
| Moderate | 4 | 21 | 3 | 0 | 28 |
| (1.9%) | (25.9%) | (13.0%) | (0.0%) | (8.6%) |
| (14.3%) | (75.0%) | (10.7%) | (0.0%) | (100.0%) |
| Moderately Severe | 0 | 5 | 13 | 4 | 22 |
| (0.0%) | (6.2%) | (56.5%) | (57.1%) | (6.8%) |
| (0.0%) | (22.7%) | (59.1%) | (18.2%) | (100.0%) |
| Severe | 0 | 2 | 6 | 3 | 11 |
| (0.0%) | (2.5%) | (26.1%) | (42.9%) | (3.4%) |
| (0.0%) | (18.2%) | (54.5%) | (27.3%) | (100.0%) |
| Total | 213 | 81 | 23 | 7 | 324 |
| (100.0%) | (100.0%) | (100.0%) | (100.0%) | (100.0%) |
| (65.7%) | (25.0%) | (7.1%) | (2.2%) | (100.0%) |
Pearson Chi-sqaure=315.063, df=12, p-value<0.001
Relation of women with depression and suicidal ideation.
| Depression Severity | Suicidal Ideation |
|---|
| Suicidal ideas not present | Suicidal ideas present | Total |
|---|
| None-minimal | 187 | 0 | 187 |
| (65.2%) | (00.0%) | (57.7%) |
| (100.0%) | (00.0%) | (100.0%) |
| Mild | 76 | 0 | 76 |
| (26.4%) | (00.0%) | (26.4%) |
| (100.0%) | (00.0%) | (100.0%) |
| Moderate | 16 | 12 | 28 |
| (5.6%) | (33.3%) | (8.6%) |
| (57.1%) | (42.9%) | (100.0%) |
| Moderately Severe | 8 | 14 | 22 |
| (2.8%) | (38.9%) | (6.8%) |
| (36.4%) | (63.3%) | (100.0%) |
| Severe | 1 | 10 | 11 |
| (0.3%) | (27.8%) | (3.4%) |
| (9.1%) | (90.9%) | (100.0%) |
| Total | 288 | 36 | 324 |
| (100.0%) | (100.0%) | (100.0%) |
| (88.9%) | (11.1%) | (100.0%) |
Pearson Chi-sqaure=193.821, df=4, p-value<0.001
Discussion
In the present study, clinically significant depression present in 18.8% women. Our study result is consistent with the figures reported for developing countries (10–44%) by the WHO [17] and Poongothai S et al., [18]. Recently published National Mental Health Survey (NMHS) reported prevalence of depression as 2.7% in India. The difference in findings may be because the survey was conducted in both rural and urban populations and used Mini International Neuro-Psychiatric Inventory (MINI) as the screening tool; but, the same study also stated that prevalence of depressive disorders are higher in females and especially ones residing in urban areas [19].
In a study conducted in Karachi, Pakistan, comparatively higher burden of depression was observed which could have been due to difference in cultures; though in our study also we have found odds of presence of depression to be more in Muslim women [20].
Age of woman: In the present study, adjusted odds of depression was maximum in women belonging to 35-44 years followed by ones with age less than 25 years [Table/Fig-2]. However, study conducted by Poongothai S et al., reported prevalence of depression to increase with increasing age [18]; but Akram B and Khuwaja F, the mean comparison reflected higher depression level after 40 years [21].
The reason for the findings in our study may be that as lady reaches 35 years, concerns regarding future of their family, especially children, increase and also increase the responsibilities of taking care of the elders–this increases stress, and subsequently depression. However, as the age increases further, women get adjusted to the situations of life. The reason for women <25 years being more depressed may be the burden of adjustment required after marriage; also, there is hassle of changed lifestyles and competition for survival which has increased drastically in present times. Fahey N et al., have explained that the protective trend observed with increasing age is based on the change in women’s position in the patriarchal social construct [22]. Older women might experience greater autonomy and play a larger role in household decision making, which enables them to navigate stressful situations more effectively.
Age difference with husband: The cause of women with age difference of more than ten years with their husbands being more depressed may be the underlying difference in maturity, experiences, social position and financial control [Table/Fig-2]. Similar results have been reported in study conducted by Kim JH et al., [23].
Education: Occurrence of depression decreased significantly with increase in the level of education of both the women and her husband in bivariate analysis [Table/Fig-2]. This finding is also supported by other studies [18,21,22,24,25]. Education enhances self-esteem, autonomy and coping capability of women, which might be the underlying mechanism for the observed protective effects.
Notably, in our study, when adjusted for other variables, depression was marginally high in women educated up to middle and secondary/senior secondary level [Table/Fig-2]. The reason comprehensible during the interview was that these women were educated enough to understand the importance of being self-dependent but not to the extent so as to be so in reality.
Religion: In our study, presence of depression was found to be significantly higher among females belonging to religion other than Hindu [Table/Fig-2]. Similar findings were reported in the study conducted by Nandi DN et al., [26].
Marital status: As in our study, significantly higher depression among women with disrupted married life was found by multiple studies conducted in Indian subcontinent [18,22,24].
Type of family: Burden of depression was observed to be significantly higher in women living in joint families [Table/Fig-2]. This is consistent with the finding of systematic review by Mirza I and Jenkins R [24]; but is in contrast to the findings of Akram B and Khuwaja F, who observed that the working women who lived in nuclear family system reported higher depression [21]. Different observation in our study may be due to the different cultural and societal structure of the countries and also because our study participants were all homemakers. Sethi BB and Sharma M also found depression to be higher in nuclear families; but their study was conducted in 1980’s and times have changed drastically since then [27] . In the present scenario of transitional societies, women find themselves more burdened–physically, mentally, and socially while living in joint families. Possibility of more autonomy and independency may be enjoyed in nuclear family.
Type and ownership of house: The burden of depression among women staying in semi-pucca or kuchha house and residing in rented house was high in bivariate analysis [Table/Fig-2]; obvious reason being–these women are usually of poor socioeconomic condition with little or no hope of betterment, which itself is a risk factor for depression.
Age at marriage: Depression was significantly less in women married between 21-23 years and it was high in women married before 18 years [Table/Fig-2]. In Indian social context, this age-group is usually said to be appropriate age of marriage for girls, as at this age they are mature enough to handle the family responsibility but not old enough so as not being able to adjust in the new surroundings. Our findings are consistent with those published by Uecker JF [28]. Shabbir S et al., also observed that the females who got married in early age have high score on depression [29].
Number of conceptions and total living children: The odds of developing depression more in women who had never conceived [Table/Fig-2]; as these women may feel lonely and insecure because in Indian culture children are considered to strengthen the marriage relationship in a positive way.
Bivariate analysis in [Table/Fig-2] showed that women with more than two living children were more depressed. This is understandable as children are dependents and more children means more money and energy needed for them to be raised. A study done by Akram B and Khuwaja F in Pakistan showed that the children number plays a significant role in development of depression [21].
Male and female children: The odds of presence of depression was more in women who had any number of male children [Table/Fig-2]. The reason behind this apparently ironic finding may be the increased stress for providing the male children so that each can grow successful, and also, in some families, due to added wish for atleast one girl child in the family. In spite of best search no original articles were found to support these findings and arguments.
No significant relation was observed between the number of female children and presence of depression in women [Table/Fig-2].
Substance abuse in family: Substance abuse in some form was present in 14.5% of the families and the odds for presence of depression in the homemakers was 4.5 times which was statistically significant [Table/Fig-2]. The substance abuser was mainly the husband, only in four cases substance abuse was also reported in other family members. This finding is omnipresent in similar researches [25,30,31]. Prevalence of mental, behavioural problems like, violence and physical morbidities, are more in substance users than in general population. These families also suffer from economic glitches. Women dependent on their husbands can compound the helplessness and psychological stress, thus contributing eventually to depression.
Perceived Economic Stability: In the present study, around one-third women were disturbed by the economic condition of their family, and this was significant risk factor for presence of depression [Table/Fig-2]. Independent studies and a review have found a close relationship between economic problems and poor mental well-being [32-34], although Diener E et al., found no or weak association [35].
Family Relations: In multivariate analysis, depression was observed to be significantly higher in women with disturbed relation with husband [Table/Fig-2]. Studies had found that symptoms of depression in women were best predicted by low level affection exchange with husband [36,37]. In Indian society, where after marriage maternal family of the women becomes distant, husband is the only psychological and social support, troubled relation with the husbands with added taunts from relatives is obvious reason of depression.
Reasons related to children: Around one-third of the study participants were worried about the education of their children–mainly due to the finances involved in higher education or because their children did not pay sufficient attention towards their studies; also one-fifth of them were concerned about their future i.e., job, marriage of girl child, earning livelihood issues. Burden of depression was significantly higher among them [Table/Fig-2]. Empirical research on the role of issues related with children and depression in homemakers is scant.
Self-image: In the present study, significantly higher odds of presence of depression in women with perceived distorted self-image were appreciated. Women felt that due to being less educated they were usually not thought to be competent enough to take part in important decisions of the family. Some (4.9%) were depressed for being not able to work and be independent/financially support their families [Table/Fig-2]. Also, most housewives felt that their work is not appreciated or recognised by other family members and their contribution is almost always taken for granted. Similar findings have been seen in other studies [18,20,22,38].
Difficulty in doing daily activities: More than half (54.5%) of the ladies with severe depression found it very difficult and 27.3% found it extremely difficult to carry out their daily routine work. Women screened for moderate depression were also observed to be facing the similar difficulty [Table/Fig-3]. It is obvious that in depression the person might face impairment in functioning in different domains of life. This is also one of the diagnostic criteria for depression according to DSM-5 [39].
Suicidal Ideation: In our study, suicidal ideas increased directly with the increase in severity of depression and it was statistically significant [Table/Fig-4]. Attempted suicide and death ideas were more common among those with major depressive disorder according to Atay IM et al., [40]. Asgard U, found a high prevalence of minor depressive disorders in suicides among Swedish women [41]. Depressive episode was seen as significant clinical condition in people attempting suicide in a systematic review done by Ahmed HU et al., [42].
Limitation
Prevalence of depression was based on self-reported data, which may be subject to recall bias and cultural factors. Another limitation is that being a cross-sectional study, no cause effect relationship could be determined.
Conclusion
Our study indicates that a relatively high number of homemakers residing in urban areas of Haldwani block are having clinically significant depression. Age, education, living conditions, marital factors and number of living children were associated with depression in this population. All these factors except age, are modifiable and should be targeted through multiple mechanisms. Also, we recommend integration of mental health care with general health care along with routine screening of all ever married women at urban health facilities for depressive symptoms. Other studies for establishing cause-effect relationship are also needed.
* Pucca: all structure built with bricks and concrete
**Kuchha/Semipucca: walls and/or roof and/or floor-not made of concrete
Pearson Chi-sqaure=315.063, df=12, p-value<0.001
Pearson Chi-sqaure=193.821, df=4, p-value<0.001