Idiopathic Unilateral Gynaecomastia in Prepubertal Age: A Rare Presentation and Review of Literature
Kamal Nain Rattan1, Dayanand Hota2, Jasbir Singh3, Ahmad Khursheed4
1 Senior Professor and Head, Department of Paediatrics Surgery, Pt.B.D. Sharma, PGIMS, Rohtak, Haryana, India.
2 Junior Resident, Department of Paediatrics, Pt.B.D. Sharma, PGIMS, Rohtak, Haryana, India.
3 Senior Resident, Department of Paediatrics, Pt.B.D. Sharma, PGIMS, Rohtak, Haryana, India.
4 Junior Resident, Department of Paediatrics, Pt.B.D. Sharma, PGIMS, Rohtak, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dayanand Hota, Room No 23, Doctors Hostel, PGIMS, Rohtak-124001, Haryana, India.
E-mail: dayanandhota@gmail.com
Unilateral idiopathic gynaecomastia of prepurtal age is a rare presentation. Complete evaluation of unilateral gynaecomastia should be done to identify etiology. We managed a case of unilateral gynaecomastia in a 10-year-old male child by surgical excision without any post-operative complications.
Child, Immature, Prepuberty
Case Report
A 10-year-old male child presented to outpatient department of paediatric surgery with complaint of enlargement of right breast. It had progressed to present size over the last six months. There was no history of pain, discharge or redness over swelling. Child was not on any medication or had previous hospitalisation for any disease. No obvious family history of similar problem was found.
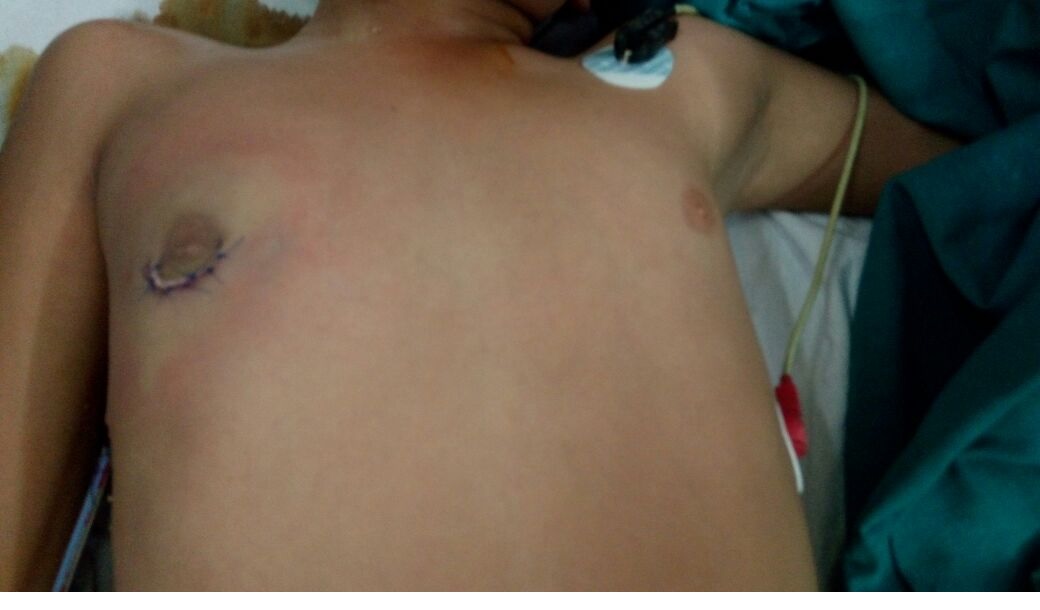
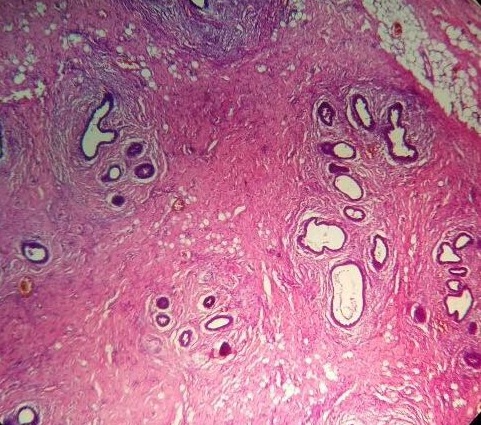
On examination, right breast was 5×5 cm in size [Table/Fig-1]. It was Non tender, smooth and soft but on deep palpation mild tenderness was present (tanner Stage 3). Left breast was normal in size. Child was non obese with BMI of 19.1 kg/m2. Normal phallus, testis size tanner Stage 1 with no ambiguity was observed. Ultrasonography of lump revealed glandular tissue with no cystic or solid mass. Child was investigated for endocrinal abnormality but hormonal assay showed all levels within normal limit [Table/Fig-2]. Hence, diagnosis of idiopathic unilateral gynaecomastia was made and surgical excision of enlarged right breast was performed through circumareolar incision. The breast tissue was dissected under vision from skin to pectoral muscle and whole of the fibro glandular breast tissue was excised. A small piece of fatty tissue was left behind to maintain normal anatomical shape [Table/Fig-3]. Wound was closed with a drain. Post-operative period was uneventful and the drain was removed after 72 hours. Histopathology [Table/Fig-4] of tissue showed ductal hyperplasia with stromal fibrosis without any feature of malignant transformation. At six months follow up, post-surgery the child showed normal breast.
Showing right breast enlargement (5×5 cm) and normal size of left breast.

Hormonal profile of patient.
| Hormones | Patient’s value | Normal value |
|---|
| Total testosterone | 6.1 ng/dL | 5.0-50.0 |
| DHEAS SO4 | 44.78 mcg/dL | 0.0-138.0 |
| Androstenedione | 89.0 ng/dL | 12-221 |
| Cortisol | 12.05 mcg/dL | 1.4-27.0 |
| FSH | 2.21 mIU/L | 1.5-12.4 |
| LH | 1.745 | 1.7-8.6 |
| E2 Estradiol | 5.00 | 5.0-10.0 |
| HCG beta subunit | 0.161 | 0.0-5.0 |
| T3 | 162.2 ng/dL | 67.0-180.0 |
| T4 | 8.22 mcg/dL | 4.7-10.4 |
| TSH | 2.43 mIU/L | 0.5-4.3 |
DHEAS SO4: dehydroepiandrosterone sulfate, FSH: follicle stimulating hormone, LH: leutinizing hormone, HCG :human chorionic gonadotropin, TSH: thyroid stimulating hormone
After surgical excision with drain in situ.
Histopathology of resected tissue; Hematoxylin and Eosin stained section showing proliferation of ducts without proliferation of lobules. Periductal fibrosis and stromal oedema is also visible in above section.
Discussion
Gynaecomastia refers to enlargement of breast tissue in males usually due to benign proliferation of glandular tissue. It may be pseudogynaecomastia in obese or true gynaecomastia which is characterised by palpable fibroglandular tissue present in areolar and nipple region. It is generally associated with excessive estrogen levels (Increased estrogen/androgen ratio) in most of the cases [1]. Higher prevalence can be observed in the neonatal period, pubertal phase and in males over age of 50 years [2]. Gynaecomastia have various aetiological factors and many studies have shown that approximately 20-25% cases are due to persistent pubertal gynaecomastia, 10%-25% are drug-induced and 25% are idiopathic [3]. It may be present as bilateral or unilateral enlargement of breast. Pubertal gynaecomastia is usually bilateral and in most cases physiological. However, cases with a breast enlargement ≥ Grade 3 (tanner staging) require endocrinal and oncological evaluation to exclude any pathology.
In contrast to pubertal gynaecomastia, prepubertal gynaecomastia especially unilateral are rare [4]. but it should be extensively evaluated by taking detailed family history, laboratory tests for endocrinal abnormality and clinical examination for aberrant sexual development and physical maturity. Neoplastic disorders should be ruled out by histopathological assessment [5,6]. Various aetiological factors seen in children and adults such as Trauma, Torsion of testis, Chemoradiotherapy, Malignancies (bronchogenic carcinoma), alcoholism, congenital adrenal hyperplasia, liver cirrhosis, renal failure, thyrotoxicosis lead to development of gynaecomastia. Certain drugs such as cimetidine, proton pump inhibitors, isoniazid [7]. Spironolactone, alkylating agents, human chorionic gonadotropin, ketoconazole and androgen inhibitors such as flutamide are all associated with the occurrence of gynaecomastia. Athelets using anabolic steroid usually present with bilateral gynaecomastia. Babigian A and Silverman RT [8] reported a series of 20 cases of gynaecomastia which were associated with usage of anabolic steroid. Lavender oil containing products has been also linked to development of gynaecomastia whic resolves after discontinuation of product. Drugs usually causes bilateral gynaecomastia which resolve spontaneously after stoppage of offending agents [9]. In a series of 581 patients of gynaecomastia, only 29 patients of prepubertal gynaecomastia (5%) were there, of which 27 were idiopathic with seven unilateral Cases (4 right sided and 3 left sided) and only in two cases the cause was identified as hyperaromatase syndrome [4]. Hyperaromatase syndrome is an autosomal dominant disease in which peripheral conversation of androgens to estrogen is enhanced by aromatase enzyme in extraglandular tissue. It is a rare familial disorder and also has endocrinal abnormality i.e. increased estrogen to androgen ratio. Hyperaromatase syndrome is characterised by pubertal gynaecomastia, accelerated growth and testicular failure and causes prepubertal breast enlargement [10]. In obese children there is increased peripheral conversation of androgen to estrogen so they present with bilateral gynaecomastia. Our case had unilateral gynaecomastia and did not show any history of familial Gynaecomastia, obesity, hormonal dearrangement or growth abnormality. Other genetic causes for gynaecomastia in prepubertal phase are Klinefelter syndrome, Androgen insensivity syndrome, neurofibromatosis Type-1 (NF-1, von Recklinghausen’s disease). Gynaecomastia and impaired phallic growth are frequently observed in adults with partial androgen insensivity syndrome but may be ameliorated by androgen therapy. Gynaecomastia in puberty, and increased levels of testosterone, estradiol and LH, but normal FSH, should be suspected of partial androgen insensivity syndrome and should undergo genetic testing for autosomal recessive mutations [11]. Andersen PS et al., presented a 3-year-old boy with unilateral gynaecomastia. In this patient, karyotype analysis from peripheral blood revealed normal 46,XY chromosomal pattern and 47,XXY mosaicism in the breast epithelial cells and it was hypothesized that the X-chromosome aneusomy in the excised breast tissue may have caused an autonomous proliferation [12]. Dursun F et al., described gynaecomastia associated with sertoli cell tumour [13]. Although we could not perform a karyotype analysis in breast tissue in our case. Neoplastic disorder of breast in male are rare, therefore, pre operative evaluation is not necessary, especially in children. Lapid O et al., in a case series of 5113 breast histological examination showed only few cases of carcinoma which were mostly found in adult patients [14].
Demirbilek H et al., also reported 2 cases of idiopathic unilateral gynaecomastia which was managed surgically [15]. Gynaecomastia can resolve spontaneously, it should be observed for self regression, however size more than Grade 3 of tanner staging or enlarged breast affects social life of children or causes psychological problems thus, it should be surgically resected. In our case, we decided to manage with surgery because it was tanner Stage 3 and child was uncomfortable with enlarged breast. A significant reduction of glandular tissue removal was achieved and this technique has allowed us to combine a good aesthetic result. In the literature, the surgical approach to the treatment of gynaecomastia shows a wide variation. Webster technique is widely accepted which advocate semicircular periareolar incision with removal of all glandular tissue [16]. New technique of liposuction such as suction-assisted lipectomy technique or ultrasound-assisted liposuction is used in recent years with good outcome [17].
Conclusion
Unilateral gynaecomastia is a rare presentation and exact aetiology is still unclear. To identify the underlying cause it should be thoroughly investigated. In idiopathic gynaecomastia, surgical resection is the treatment of choice. In our case, we surgically excised the whole glandular tissue leaving some fatty tissue in the subareolar region to maintain normal anatomy of male breast.
DHEAS SO4: dehydroepiandrosterone sulfate, FSH: follicle stimulating hormone, LH: leutinizing hormone, HCG :human chorionic gonadotropin, TSH: thyroid stimulating hormone
[1]. Kronenberg HM, William’s Textbook of Endocrinology Melmed S, Polonsky KS, Larsen PR. Eds 2008 ed.11thSaunders Elsevier:669-71. [Google Scholar]
[2]. McKiernan JF, Hull D, Breast development in the newbornArch Dis Child 1981 56(7):525-29.10.1136/adc.56.7.5257271286 [Google Scholar] [CrossRef] [PubMed]
[3]. Braunstein GD, GynecomastiaN Engl J Med 1993 328(7):490-95.10.1056/NEJM1993021832807088421478 [Google Scholar] [CrossRef] [PubMed]
[4]. Einav-Bachar R, Phillip M, Aurbach-Klipper Y, Lazar L, Prepubertal gynaecomastia: aetiology, course and outcomeClin Endocrinol (Oxf) 2004 61(1):55-60.10.1111/j.1365-2265.2004.02059.x15212645 [Google Scholar] [CrossRef] [PubMed]
[5]. Braunstein GD, Clinical practice. GynecomastiaN Engl J Med 2007 357(12):1229-37.10.1056/NEJMcp07067717881754 [Google Scholar] [CrossRef] [PubMed]
[6]. Johnson RE, Murad MH, Gynecomastia: Pathophysiology, Evaluation, and ManagementMayo Clin Proc 2009 84(11):1010-15.10.1016/S0025-6196(11)60671-X [Google Scholar] [CrossRef]
[7]. Goud BKM, Devi OS, Nayal B, Devaki RN, A rare case of unilateral gynecomastia during antituberculous chemotherapy with isoniazidIndian J Pharmacol 2012 44(4):521-22.10.4103/0253-7613.9934023087519 [Google Scholar] [CrossRef] [PubMed]
[8]. Babigian A, Silverman RT, Management of gynecomastia due to use of anabolic steroids in bodybuilders Plast Reconstr Surg 2001 107:240-42.10.1097/00006534-200101000-0003911176630 [Google Scholar] [CrossRef] [PubMed]
[9]. Henley DV, Lipson N, Korach KS, Bloch CA, Prepubertal Gynecomastia Linked to Lavender and Tea Tree OilsN Engl J Med 2007 356(5):479-85.10.1056/NEJMoa06472517267908 [Google Scholar] [CrossRef] [PubMed]
[10]. Stratakis CA, Vottero A, Brodie A, Kirschner LS, DeAtkine D, Lu Q, The aromatase excess syndrome is associated with feminization of both sexes and autosomal dominant transmission of aberrant P450 aromatase gene transcriptionJ Clin Endocrinol Metab 1998 83(4):1348-57. [Google Scholar]
[11]. Hellmann P, Christiansen P, Johannsen TH, Main KM, Duno M, Juul A, Male patients with partial androgen insensitivity syndrome: a longitudinal follow-up of growth, reproductive hormones and the development of gynaecomastiaArch Dis Child 2012 97(5):403-09.10.1136/archdischild-2011-30058422412043 [Google Scholar] [CrossRef] [PubMed]
[12]. Andersen PS, Petersen BL, Juul A, Andersen M, Prepubertal unilateral gynecomastia and the presence of 47,XXY mosaicism in breast epithelial cells: a case reportJ Pediatr Surg 2013 48(2):e21-e23.10.1016/j.jpedsurg.2012.11.05123414896 [Google Scholar] [CrossRef] [PubMed]
[13]. Dursun F, Su Dur SM, Şahin C, Kırmızıbekmez H, Karabulut MH, Yörük A, A Rare Cause of Prepubertal Gynecomastia: Sertoli Cell Tumor [Internet]Case Reports in Pediatrics 2015 [cited 2017 Oct 10] Available from: https://www.hindawi.com/journals/cripe/2015/439239/10.1155/2015/43923926366315 [Google Scholar] [CrossRef] [PubMed]
[14]. Lapid O, Jolink F, Meijer SL, Pathological findings in gynecomastia: analysis of 5113 breastsAnn Plast Surg 2015 74(2):163-66.10.1097/SAP.0b013e3182920aed23788148 [Google Scholar] [CrossRef] [PubMed]
[15]. Demirbilek H, Bacak G, Baran RT, Avcı Y, Baran A, KeleŞ A, Prepubertal Unilateral Gynecomastia: Report of 2 CasesJ Clin Res Pediatr Endocrinol 2014 6(4):250-53.10.4274/jcrpe.147725541897 [Google Scholar] [CrossRef] [PubMed]
[16]. Longheu A, Medas F, Corrias F, Farris S, Tatti A, Pisano G, Surgical management of gynecomastia: experience of a general surgery centerG Chir 2016 37(4):150-54.10.11138/gchir/2016.37.4.15027938530 [Google Scholar] [CrossRef] [PubMed]
[17]. Wong KY, Malata CM, Conventional versus ultrasound-assisted liposuction in gynaecomastia surgery: a 13-year reviewJ Plast Reconstr Aesthetic Surg 2014 67(7):921-26.10.1016/j.bjps.2014.03.00424731803 [Google Scholar] [CrossRef] [PubMed]