Case Report
A 25-year-old female presented to Neurology Emergency with history of sudden onset behavioural change, inability to identify attendants and with irrelevant talking since two weeks which was noticed by her family members. An hour after the admission she developed inability to walk which was followed by two episodes of generalised tonic-clonic seizures. Thereafter, patient became unconscious and was admitted into the Intensive Care Unit (ICU). During her stay in ICU she was given antiplatelet-acetylsalicylic 150 mgHS; lipid lowering agent-atorvastatin 10 mg HS; analgesic-acetylaminophen 500 mg q4hr PRN; for headache. Detailed enquiry from the relatives revealed an episode of severe, continous pain in the central abdomen accompanied with vomiting that happened four months back. The pain lasted for 10 days. This was relieved by medication from a local doctor. Details of the medical treatment were not available with the patient. There was no past history for any medical illness or any chronic drug use. General physical examination was unremarkable. Laboratory investigations were done and revealed normal complete blood count, Erythrocyte Sedimentation Rate (ESR), liver function tests and kidney function tests. Cerebrospinal Fluid (CSF) analysis was also within normal limits. Since patient presented with history of pain abdomen and neurological changes urinary porphobilinogen was done which came out to be normal. Abdominal sonography was done which revealed normal visceral organs without any hepatosplenomegaly with normal major abdominal vessels and their branches. MRI brain with MR Angiography (MRA) was done which showed multifocal areas of hyperintensities on T2WI with diffusion restriction in bilateral fronto-parietal lobes involving cortex and subcortical white matter [Table/Fig-1a,b]. On MRA diffuse multifocal segmental areas of luminal narrowing with skip areas were seen, giving beaded appearance in proximal segments of bilateral Anterior Cerebral Arteries (ACA), Middle Cerebral Arteries (MCA) and Posterior Cerebral Arteries (PCA) [Table/Fig-1c,d]. No Evidence of Subarachnoid Haemorrhage (No e/o SAH). Possibilities of primary angitis of brain and RCVS were kept.
a) Axial T2WI image and b) Axial DWI image displaying multifocal areas of cortical and subcortical hyperintensities in bilateral fronto-parietal region consistent with acute infarcts with diffusion restriction.
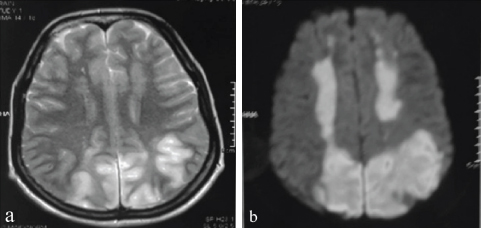
c) TOF (Time of Flight) MR Angiography in coronal and d) axial projection showing multifocal segmental areas of luminal narrowing (arrows) with skip areas giving a beaded appearance involving bilateral A1 and A2 segments of ACA (white arrow heads); bilateral M1 and M2 segments of MCA (black open arrow heads) and bilateral P1 and P2 segments of PCA (black open arrows).
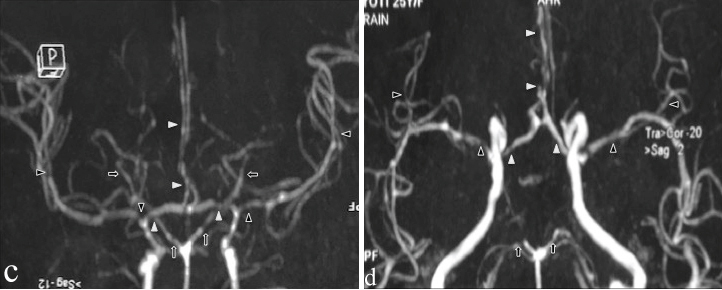
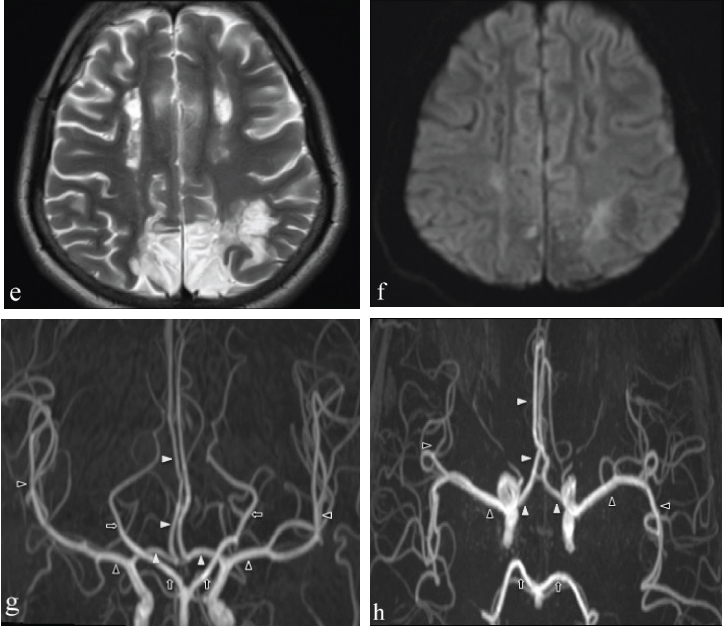
During the course in ICU, patient regained complete consciousness after 15 days and was able to identify the relatives and became self ambulatory. She complained of loss of vision in the left half of her field of vision. Patient was discharged from the hospital and was explained to come for follow up in the Outpatient Department (OPD). MRI brain with MRA was repeated after three months which revealed chronic infracts [Table/Fig-1e,f] in the areas corresponding with diffusion restriction in previous scans and a normal MRA [Table/Fig-1g,h]. Based on the aforementioned findings along with demonstrable reversibility of intra-cranial arterial stenosis and residual chronic infarcts a diagnosis of RCVS was suggested. Patient was discharge on the same medical treatment which was given in ICU. Presently, the patient is on three monthly follow up in the OPD and is doing well without any recovery of her vision.
Follow up MRI images after 3 months: e) Axial T2WI image; f) Axial DWI image; g) TOF MR Angiography coronal projection and; h) TOF MR Angiography axial projection, reveal gross reduction of hyperintensities in fronto-parietal region on DWI (f) consistent with chronic infracts in T2W axial image (e) in the areas corresponding to earlier lesions of acute infarct with diffusion restriction. Corresponding TOF MR Angiography coronal and axial images (g and h) showing complete resolution of multifocal narrowing’s in bilateral A1 and A2 segments of ACA (white arrow heads); bilateral M1 and M2 segments of MCA (black open arrow heads) and bilateral P1 and P2 segments of PCA (black open arrows).
Discussion
Reversible cerebral vasoconstriction syndrome is a syndrome historically known by various names viz., migrainous vasospasm, Postpartum vasospasm, sexual vasospasm, drug induced vasospasm, Call-Flemming vasospasm etc, but is now been unified as RCVS by Calabrese LH et al., [1].
RCVS is a well known syndrome mimicking diverse conditions both clinically and radiologically. Because of diverse spectrum, it may represent common endpoint to various conditions [1,2]. Pathologically, there is altered cerebral vascular tone without histological evidence of active inflammation/vasculitis which may lead to ischaemic stroke, associated complications or even death. Various mechanism have been postulated to play role in manifestation of RCVS such as: (a) sympathetic over activity as evidenced by correlation of disease activity with blood pressure changes; (b) oxidative stress -increase urine levels of prostaglandin; and (c) endothelial dysfunction because of similar radiological picture as Posterior Reversible Encephalopathy Syndrome (PRES) [1-3].
It can occur spontaneously or secondary to various inciting triggers (both hormonal and biochemical) and factors such as migraine, postpartum state, exposure to vasoactive substances or drugs, tumours such as pheochromocytoma, bronchial carcinoid tumour, paraganglioma, trauma, surgery, dissection, unruptured aneurysm, various medical conditions such as antiphospholipid syndrome and thrombocytopenic purpura etc., [1,4-6].
It typically affects patients in 4th decade (mean age group); however, children and adolescent can be affected with female to male ratio being 2:1 [3].
Clinically, RCVS most commonly presents as hyper acute thunderclap headache having waxing and waning course [7,8]. Alternatively in association or as sequelae there may be focal neurological deficit, generalised seizures, altered mental status, transient ischaemic attack, cerebral infarction, visual disturbances, aphasia, hemiparesis, convexity subarachnoid haemorrhage or concomitant PRES etc., [1,4-6].
It poses a great diagnostic dilemma; however, knowledge of symptoms and radiological manifestations can help in accurate diagnosis and treatment [1]. Diagnostic work-up includes laboratory and radiological evaluation to document and monitor cerebral vasoconstriction and to rule out potential differential diagnosis and complications.
Proposed diagnostic criteria by Calabrese LH et al., [1] which has been modified by International Health Society includes [5]: 1) hyperacute thunderclap headache with/without neurological deficit; 2) monophasic course with no fresh symptom at one month; 3) normal/mild elevated CSF proteins <80 mg/dL; Leukocyte level <10/mm3; normal glucose level; 4) CT/MR/catheter angiography -multisegmental cerebral artery vasoconstriction; 5) reversibility of angiographic abnormalities within 12 weeks, if death occurs then rule out other possible differentials on postmortem. These criteria have not been validated but provide useful clinical diagnosis.
Diagnostic work-up includes laboratory and radiological evaluation. Biochemical analysis includes ESR, CRP and CSF analysis (WBC and protein levels) all of these usually being within normal limits or minimally elevated [2,3].
Imaging evaluation mainly includes non invasive tests such as transcranial Doppler, CT/MRA or invasive study such as catheter angiography [3,9]. Imaging is done mainly to document and monitor cerebral vasoconstriction with near total reversal after 12 weeks and rule out potential differential diagnosis and complications (stroke, haemorrhage, vasogenic oedema) [1,9,10].
According to published reports in literature [11,12] typically findings of RCVS on MRA are multifocal narrowing with skip areas giving beaded appearance involving medium and large size cerebral arteries with reversal within three months which were similar to findings in present case suggesting RCVS. However, there was an atypical clinical presentation in present case as there was no thunderclap headache; which is the most common clinical presentation though the laboratory as well as imaging findings on MRI was quite typical of RCVS. However, no specific aetiology could be attributed to cause of RCVS in the present case hence presumed to be of spontaneous aetiology.
The initial angiographic findings may be unremarkable for first 4-5 days in patients suspected of RCVS; in fact in upto one-third of patients, cerebral vasoconstriction may not be visualised during the first week following symptom onset [10]. This finding may be attributed to segmental vasoconstriction beginning in small, peripheral/distal arterioles which then proceed to involve medium and large cerebral arteries [13]; as suggested by Ducros A et al., [4].
For evaluation of cerebral vasculature, Digital Subtraction Angiography (DSA) is the gold standard; which may detect cerebral vasoconstriction in small calibre peripheral/distal cerebral vessels even when initial CTA/MRA. findings appear unremarkable [12,14,15]. Ducros A et al., found sensitivity of MRA and CTA for detecting RCVS-vasoconstriction to be 80% as compared with conventional angiography [4]. However, if cerebral vasoconstriction is not demonstrated on initial imaging and after exclusion of other diagnosis, the patient should be managed as possible or probable RCVS [1].
Recent advances in imaging includes vessel wall imaging using high resolution 2D/3D imaging with acquisition of high resolution T2-weighted images along with pre/post contrast T1-weighted images and perfusion imaging [16].
Main differential diagnosis to be considered are primary angiitis of CNS, aneurysmal Subarachnoid haemorrhage related vasospasm; however, there are many potential alternative diagnosis such as migraine, PRES, cortical vein thrombosis, amyloid angiopathy, hypertensive haemorrhage, giant cell arteritis and meningitis etc., [5,10].
Prognosis is usually good with complete symptomatic resolution in three weeks and no new symptoms thereafter and vasoconstriction reversal at three months. However, a minority of patients may have worsening of symptoms and rarely few might develop fulminant course leading to permanent disability or death [8].
Treatment is guided mostly on symptomatic relief such as use of calcium channel blocker for headache, vasodilators, withdrawal of suspected trigger etc. Alternatively intra-arterial vasodilator therapy or balloon angioplasty can also be done [1].
Conclusion
Diagnosis of RCVS may pose difficulties as it may mimic potential differential diagnosis both clinically and radiologically such as primary angitis of CNS/vasculitis, PRES, SAH etc. Knowledge of typical clinical course with careful search for any potential triggers or vasoactive substances along with characteristic laboratory and radiological evidences help in diagnosing RCVS for appropriate patient treatment and minimising complications.
[1]. Calabrese LH, Dodick DW, Schwedt TJ, Singhal AB, Narrative review: Reversible cerebral vasoconstriction syndromesAnn Intern Med 2007 146:34-44.10.7326/0003-4819-146-1-200701020-0000717200220 [Google Scholar] [CrossRef] [PubMed]
[2]. Gupta S, Zivadinov R, Ramasamy D, Ambrus JL, Reversible cerebral vasoconstriction syndrome (RCVS) inantiphospholipid antibody syndrome (APLA): the role of centrally acting vasodilators- case series and review of literatureClin Rheumatol 2014 33(12):1829-033.10.1007/s10067-013-2434-924277114 [Google Scholar] [CrossRef] [PubMed]
[3]. Sheikh HU, Mathew PG, Reversible cerebral vasoconstriction syndrome: updates and new perspectivesCurr Pain Headache Rep 2014 18(5):41410.1007/s11916-014-0414-724658747 [Google Scholar] [CrossRef] [PubMed]
[4]. Ducros A, Boukobza M, Porcher R, Sarov M, Valade D, Bousser MG, The clinical and radiological spectrum of reversible cerebral vasoconstriction syndrome: a prospective series of 67 patientsBrain 2007 130(12):3091-101.10.1093/brain/awm25618025032 [Google Scholar] [CrossRef] [PubMed]
[5]. Miller TR, Shivashankar R, Mossa-Basha M, Gandhi D, Reversible cerebral vasoconstriction syndrome, part 1: epidemiology, pathogenesis, and clinical courseAm J Neuroradiol 2015 36(8):1392-99.10.3174/ajnr.A421425593203 [Google Scholar] [CrossRef] [PubMed]
[6]. Chen SP, Fuh JL, Lirng JF, Chang FC, Wang SJ, Recurrent primary thunderclap headache and benign CNS angiopathy: spectra of the same disorder?Neurology 2006 67(12):2164-69.10.1212/01.wnl.0000249115.63436.6d17190937 [Google Scholar] [CrossRef] [PubMed]
[7]. Ducros A, L37: Reversible cerebral vasoconstriction syndrome-distinction from CNS vasculitisPresse Med 2013 42(4):602-04.10.1016/j.lpm.2013.01.03723481360 [Google Scholar] [CrossRef] [PubMed]
[8]. Ducros A, Bousser MG, Reversible cerebral vasoconstriction syndromePract Neurol 2009 9(5):256-67.10.1136/jnnp.2009.18785619762885 [Google Scholar] [CrossRef] [PubMed]
[9]. Marder CP, Donohue MM, Weinstein JR, Fink KR, Multimodal imaging of reversible cerebral vasoconstriction syndrome: a series of 6 casesAmerican Journal of Neuroradiology 2012 33(7):1403-11.10.3174/ajnr.A296422422190 [Google Scholar] [CrossRef] [PubMed]
[10]. Miller TR, Shivashankar R, Mossa-Basha M, Gandhi D, Reversible cerebral vasoconstriction syndrome, part 2: diagnostic work-up, imaging evaluation, and differential diagnosisAm J Neuroradiol 2015 36(9):1580-88.10.3174/ajnr.A421525614476 [Google Scholar] [CrossRef] [PubMed]
[11]. Lee WJ, Yeon JY, Jo KI, Kim JS, Hong SC, Reversible cerebral vasoconstriction syndrome and posterior reversible encephalopathy syndrome presenting with deep intracerebral hemorrhage in young womenJournal of Cerebrovascular and Endovascular Neurosurgery 2015 17(3):239-45.10.7461/jcen.2015.17.3.23926523259 [Google Scholar] [CrossRef] [PubMed]
[12]. Chen SP, Fuh JL, Wang SJ, Chang FC, Lirng JF, Fang YC, Magnetic resonance angiography in reversible cerebral vasoconstriction syndromesAnn Neurol 2010 67(5):648-56. [Google Scholar]
[13]. Sattar A, Manousakis G, Jensen MB, Systematic review of reversible cerebral vasoconstriction syndromeExpert Rev CardiovascTher 2010 8:1417-21.10.1586/erc.10.12420936928 [Google Scholar] [CrossRef] [PubMed]
[14]. Villablanca JP, Rodriguez FJ, Stockman T, Dahliwal S, Omura M, Hazany S, MDCTangiographyfor detection and quantification of small intracranial arteries: comparison with conventional catheter angiographyAJR Am J Roentgenol 2007 188(2):593-602.10.2214/AJR.05.214317242273 [Google Scholar] [CrossRef] [PubMed]
[15]. Agid R, Andersson T, Almqvist H, Willinsky RA, Lee SK, TerBrugge KJ, Negative CT angiography findings in patients with spontaneous subarachnoid hemorrhage: when is digital subtraction angiography still needed?AJNR Am J Neuroradiol 2010 31(4):696-705.10.3174/ajnr.A188419942709 [Google Scholar] [CrossRef] [PubMed]
[16]. Obusez EC, Hui F, Hajj-Ali RA, Cerejo R, Calabrese LH, Hammad T, Jones SE, High-resolution MRI vessel wall imaging: spatial and temporal patterns of reversible cerebral vasoconstriction syndrome and central nervous system vasculitisAJNR Am J Neuroradiol 2014 35(8):1527-32.10.3174/ajnr.A390924722305 [Google Scholar] [CrossRef] [PubMed]