Intracardiac Air Embolism in the Newborn: Presentation of Two Cases and Review of the Literature
Shilpa Kalane1, Sheela Patil2, Rajan Joshi3, Uday Devaskar4
1 Neonatologist, Department of Neonatology, Deenanath Mangeshkar Hospital, Pune, Maharashtra, India.
2 Respiratory Therapist, Department of Neonatology, Deenanath Mangeshkar Hospital, Pune, Maharashtra, India.
3 Head Paediatrics, Department of Neonatology, Deenanath Mangeshkar Hospital, Pune, Maharashtra, India.
4 Chief Neonatologist, Department of Neonatology, UCLA Hospital, Los Angeles, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shilpa Kalane, Neonatologist, Department of Neonatology, 3rd Floor, Super Specialty Building, Deenanath Mangeshkar Hospital, Pune 411004, Maharashtra, India.
E-mail: drshilpakalane@gmail.com
Intracardiac air embolism is a rare but potentially life threatening event with a very high mortality. It should be suspected in any infant with sudden cardiopulmonary decompensation. Hereby, we describe cases of two preterm neonates with sudden cardiopulmonary decompensation. Retrospectively, it was diagnosed to be due to cardiac air embolism on chest radiograph. One of the neonate responded to aggressive treatment and survived. The prognosis for this condition remains poor and it may improve with early recognition and aggressive therapy.
Cardiac, Neonate, Therapy
Case Report
Case 1
A male neonate (26 weeks gestation, weight 0.9 Kg) was born by spontaneous vaginal delivery to a primigravida mother. At birth, the baby developed respiratory distress syndrome, was intubated and was transferred to DMH for further treatment. The infant was treated with two doses of exogenous surfactant. Subsequently, the infant was treated according to the Neonatal Intensive Care Unit (NICU) protocol including insertion of umbilical venous and arterial catheter. At eight hours of life, baby was noticed to be in shock manifested by severe hypotension (mean BP<20 mmHg) with sinus tachycardia (HR 180-200 beats/min) assessed by electrocardiography. Serum electrolytes, ionized calcium, magnesium, cortisol concentrations were normal. Sepsis screen was negative. Hypotension was treated with infusion of normal saline, Dobutamine, Dopamine, Adrenaline, Hydrocortisone and Vasopressin. Despite aggressive pharmacotherapy, haemodynamic status remained unstable for 54 hours. Echocardiogrphy revealed haemodynamically significant Patent Ductus Arteriosus (PDA) of size 3.5 mm which was treated with Ibuprofen.
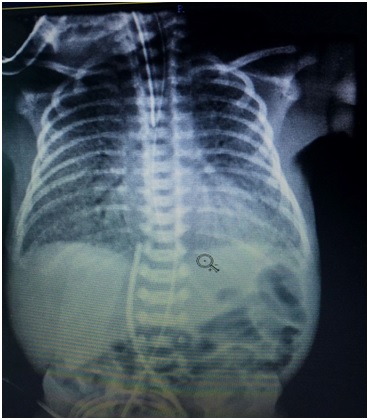
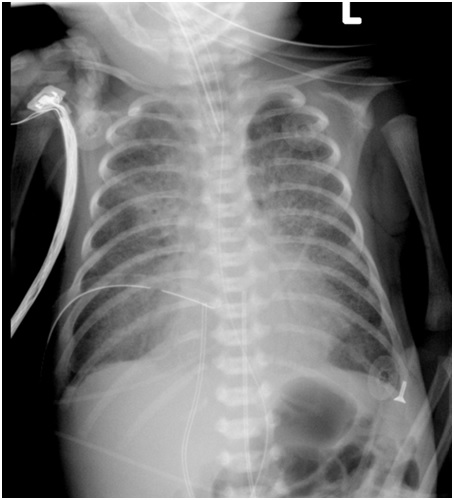
Cardiopulmonary status improved at 70 hours of life. He was discharged home at three months of age. Patient is four years old now and his developmental milestones are appropriate for the age. Intracardiac Air Embolism (ICAE) was diagnosed after a thorough retrospective review of the chest radiographs performed during the sudden onset of cardiopulmonary deterioration [Table/Fig-1]. It showed hyperlucency within left cardiac border suggestive of ICAE. Chest radiograph at 72 hours of life showed complete resolution of ICAE [Table/Fig-2]. Even though, the diagnosis of ICAE was retrospective during the clinical audit meeting. After debriefing session, it was concluded that air was not accidentally introduced via umbilical arterial or venous catheter.
An anteroposterior chest radiograph of case 1 showing an area of hyperlucency within left cardiac border suggestive of intracardiac air embolism.

An anteroposterior chest radiograph of case 1 showing resolution of the intracardiac air embolism.
Case 2
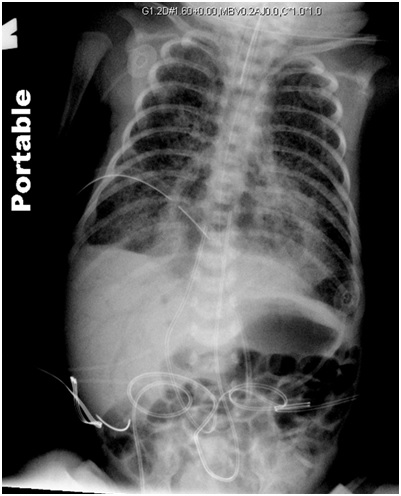
A male neonate (30 weeks gestation, weight 1.36 kg) was delivered by a caesarean section for worsening prenatally diagnosed idiopathic non-immune hydrops. Baby was apnoeic at birth and required extensive resuscitation including insertion of endotracheal tube, thoracotomy and pericardiotomy. During the subsequent five days, the baby was treated appropriately according to the hospital NICU protocol [insertion of umbilical arterial and venous catheters, exogenous surfactant, positive pressure ventilation (conventional and high frequency oscillatory ventilation), infusion of dopamine (10 mcg/kg/min), dobutamine (10 mcg/kg/min) and hydrocortisone (5 mg/kg), inhalational nitric oxide (20 parts per million)]. Serial Chest radiograph at 24 hours, 60 hours and 72 hours of life showed presence of pneumothorax (right), pulmonary interstitial emphysema and pulmonary oedema at separate times. These findings were resolved by the end of the fourth day [Table/Fig-3]. On the fifth day, while the baby was in a very stable condition, he developed severe bradycardia (HR <60 beats/min), hypotension (mean BP <16 mmHg) and desaturation needing extensive Cardiopulmonary Resuscitation (CPR). Chest radiograph [Table/Fig-4] done during the resuscitation demonstrated the presence of air in the right and the left side of the heart, inferior vena cava and hepatic veins. Despite giving extensive CPR the baby died. After detailed investigations among the NICU staff, it was concluded that sudden development of ICAE was not due to accidental introduction of air via umbilical venous/arterial catheter or abnormal functioning of thoracotomy tube. Parents declined autopsy.
An anteroposterior chest radiograph of case 2 before resuscitation with umbilical arterial and venous catheter and a right intercostal drain in situ.
An anteroposterior chest radiograph of case 2 during cardiopulmonary resuscitation showing an area of hyperlucency within the right and left cardiac borders suggestive of ICAE.
Discussion
In a sick newborn baby with respiratory failure while treated with assisted ventilation, life threatening conditions like tension pneumothorax, pneumo-pericardium, pulmonary embolism, pericardial or pleural effusion, cardiac arrhythmia, ventricular fibrillation, myocardial infarction or cardiac arrest due to electrolyte imbalance like hyper- or hypokalemia and a rare occurrence of ICAE can develop unexpectedly [1]. We report development of ICAE in two premature babies, one of whom survived. Brief review of the literature is discussed.
Intracardiac air embolism is a rare but potentially life threatening event with a very high mortality that occurs because of the entrapment of air in the vasculature [1]. Symptoms vary from no to severe life threatening events. Respiratory distress is almost a universal finding of venous air embolism while the symptoms of arterial embolism vary depending on the organ affected [2]. While systemic air embolisation to the pulmonary veins, right ventricle and superior and inferior vena cava are common, ICAE is rare and it is typically heralded by an abrupt deterioration of cardiopulmonary status and can be suspected clinically by sudden hypotension, tachycardia or aspiration of air from umbilical venous/arterial catheter if the catheter is in place [1]. The diagnosis should be considered in an infant who is rapidly deteriorating on the ventilator. In present case report, the first case neonate presented with sudden refractory hypotension while the second case neonate had sudden deterioration in the form of sudden hypotension and bradycardia requiring extensive resuscitation. Arterial blood gas may show hypoxia and hypercarbia. The diagnosis is best made by performing a radiograph and demonstrating air in the heart, intravascular space or organs [1]. Diagnosis in both cases was made by chest radiography which showed hyperlucent area within cardiac borders. In addition, echocardiography has been used to document the presence of air and may show ventricular strain pattern, evidence of acute right ventricular dilation and pulmonary artery hypertension [3]. Computed tomography, magnetic resonance imaging or ventilation perfusion scan have also been performed to further aid in the diagnosis [4]. Air may be rapidly absorbed from the circulation while waiting for the diagnostic imaging. Based upon a high index of suspicion and the exclusion of other life-threatening processes, ICAE is typically a retrospective clinical diagnosis. It may even go undetected at autopsy because of the rapid absorption of intravascular gas after death, especially pure oxygen [5].
For air embolism to occur following must be present: A direct communication and pressure gradient between source of air and vasculature favouring the passage of air into the circulation [6]. Risk factors for ICAE are trauma, vascular interventions, barotrauma from mechanical ventilation or resuscitation and air leak syndromes [7-9]. Premature infants are at increased risk of ventilator associated air embolism. Risk factors in our cases were same as above. Exact source of air is not known in both cases. After analysing both cases in detail and looking at the time line of clinical deterioration and underlying risk factors, barotrauma from mechanical ventilation may have caused ICAE.
There is no consensus about the optimum management of these infants. However, when an ICAE is suspected, the neonate should be assessed for airway, breathing and circulation. Appropriate supportive treatment should be started while other investigations are underway. Positioning infant in left lateral decubitus, trendelenburg or left lateral decubitus head down for venous embolism and supine for arterial air embolism is a simple bedside management to prevent embolism [10]. Administration of high fraction of inspired oxygen using soft rubber catheters for draining pneumothorax and maneuvers like early aspiration of air from right ventricle via umbilical artery or venous catheter have shown to be beneficial especially if the air leak is small and self-sealing [10]. In adults, other therapies like hyperbaric oxygen, anticoagulation, glucocorticoids, lidocaine have been attempted without proven benefits.
Since, the prognosis of this condition remains poor, efforts should be made to reduce the risk of air embolism. For neonates treated with mechanical ventilator, strategy of permissive hypercapnia should be considered to avoid barotrauma. Maneuvers like occluding the hub of the central venous catheter during insertion, keeping all connections to a central line closed and locked when not in use, withdrawing blood and injecting medications with the neonate supine (i.e., below the level of the heart) should be done [11]. Similar principles should apply to the insertion, removal, use, and manipulation of arterial catheters.
Conclusion
The incidence for ICAE is likely to increase with the improved survival of extremely premature neonates. The incidence is under reported because of the lack of recognition of acute event and the rapid loss of signs after death. Barotrauma from ventilation may have caused intracardiac air embolism in our patients.
[1]. Smith J, Els I, Intracardiac air-the ‘hospital killer’ identified? Case reports and review of literatureSouth African Medical Journal 2003 93(12):922-27. [Google Scholar]
[2]. Mirski MA, Lele AV, Fitzsimmons L, Toung TJ, Diagnosis and treatment of vascular air embolismAnesthesiology 2007 106(1):164-77.10.1097/00000542-200701000-0002617197859 [Google Scholar] [CrossRef] [PubMed]
[3]. Muth CM, Shank ES, Gas embolismN Engl J Med 2000 342(7):476-82.10.1056/NEJM20000217342070610675429 [Google Scholar] [CrossRef] [PubMed]
[4]. Bedford RF, Marshall WK, Butler A, Welsh JE, Cardiac catheters for diagnosis and treatment of venous air embolism: A prospective study in manJ Neurosurg 1981 55(4):610-14.10.3171/jns.1981.55.4.06106792326 [Google Scholar] [CrossRef] [PubMed]
[5]. Rudd PT, Wigglesworth JS, Oxygen embolus during mechanical ventilation with disappearance of signs after deathArch Dis Child 1982 57(3):237-39.10.1136/adc.57.3.2377073306 [Google Scholar] [CrossRef] [PubMed]
[6]. Jorens PG, Van Marck E, Snoeckx A, Parizel PM, Nonthrombotic pulmonary embolismEur Respir J 2009 34(2):452-74.10.1183/09031936.0014170819648522 [Google Scholar] [CrossRef] [PubMed]
[7]. Schmitt HJ, Hemmerling TM, Venous air emboli occur during release of positive end-expiratory pressure and repositioning after sitting position surgeryAnesth Analg 2002 94(2):400-03.10.1097/00000539-200202000-0003211812707 [Google Scholar] [CrossRef] [PubMed]
[8]. Qazi AQ, Haider ZA, Najam Y, Fatal systemic air embolism in a neonate after cardiopulmonary resuscitationAPSP Journal of Case Reports 2015 6(1):11-12. [Google Scholar]
[9]. Timpa JG, O’Meara C, McILwain RB, Dabal RJ, Alten JA, Massive systemic air embolism during extracorporeal membrane oxygenation support of a neonate with acute respiratory distress syndrome after cardiac surgeryJ Extra Corpor Technol 2011 43(2):86-88. [Google Scholar]
[10]. Alvaran SB, Toung JK, Graff TE, Benson DW, Venous air embolism: Comparative merits of external cardiac massage, intracardiac aspiration, and left lateral decubitus positionAnesth Analg 1978 57(2):166-70.10.1213/00000539-197803000-00003565152 [Google Scholar] [CrossRef] [PubMed]
[11]. Pronovost PJ, Wu AW, Sexton JB, Acute decompensation after removing a central line: Practical approaches to increasing safety in the intensive care unitAnn Intern Med 2004 140(12):1025-33.10.7326/0003-4819-140-12-200406150-0001315197020 [Google Scholar] [CrossRef] [PubMed]