Giant Cells Tumour of the Distal Phalanx of the Finger- A Case Report
Selim Daas1, Med Ali Sbai2, Sana Ben Slama3, Adel Khorbi4
1 Assistant Professor, Department of Orthopaedic Surgery, MT Maamouri Hospital, University Tunis El Manar, Faculty of Medicine of Tunis, Nabeul, Tunisia.
2 Professor, Department of Orthopaedic Surgery, MT Maamouri Hospital, University Tunis El Manar, Faculty of Medicine of Tunis, Nabeul, Tunisia.
3 Assistant Professor, Department of Pathology, M. Slim Hospital, University Tunis El Manar, Faculty of Medicine of Tunis, Tunisia.
4 Professor, Department of Orthopaedic Surgery, MT Maamouri Hospital, University Tunis El Manar, Faculty of Medicine of Tunis, Nabeul, Tunisia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sana Ben Slama, Assistant Professor, Department of Pathology, M. Slim Hospital, 2046 Sidi Daoued, Tunis, Tunisia.
E-mail: mallouli.sana@gmail.com
Giant Cell Tumour (GCT) of the hand phalangeal bones are rare but with local aggressiveness and high risk of recurrence. Their treatment is exclusively surgical. We report a case of GCT occurring in the third phalanx of the index. A 83-year-old woman, right-handed, presented with a painful tumefaction of the distal phalanx of the right index finger. Examination revealed a swelling of the distal phalanx, of hard consistency, fixed, slightly painful to the palpation. The radiography showed an expensive lytic lesion taking up the entire third phalanx. A surgical biopsy revealed an aspect of a GCT invading bone, soft tissue and dermis. It was Stage 2 of the radio histological classification of enneking. In view of the local progression of the GCT, a proximal trans-phalangeal amputation to the index was performed. Until her last follow up after 24 months, the patient didn’t show any recurrence or metastasis. The location of GCT in the metacarpal bones is rare. The diagnosis is based on the clinical, radiological and histopathological findings. After surgery, the prognosis is related to rate of recurrence.
Amputation, Hand, Ungual dystrophy
Case Report
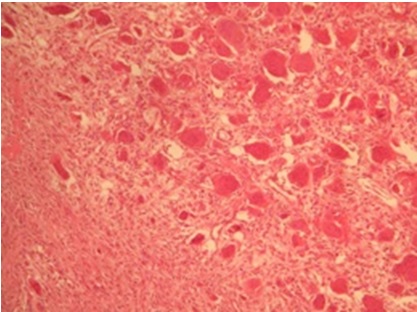
A 83-year-old woman, right-handed, presented with a painful tumefaction of the distal phalanx of the right index finger which had gradually increased in size over two years period. Finger examination revealed a swelling of the distal phalanx, of hard consistency, fixed, slightly painful to the palpation, associated with ulcerated skin and ungual dystrophy. The distal interphalangeal joint of the index finger was stiff [Table/Fig-1a]. Radiographic examination (X-ray) showed an expansile lytic lesion taking up the entire third phalanx, with distal interphalangeal joint involvement [Table/Fig-1b]. The diagnosis suggested was malignant bone tumuor with cutaneous extension, the other differential diagnosis was a simply osteitis of the distal phalanx. A surgical biopsy was done. Histopathology examination revealed an aspect of a GCT invading bone, soft tissue and dermis [Table/Fig-2]. It was Stage 2 of the radio histological classification of enneking [1]. In view of the local progression of the GCT, an amputation of both proximal intermediate phalanx of the index was performed. Until her last follow up after 24 months, the patient didn’t show any recurrence or metastasis on both physical and radiological examinations.
a) Clinical view with cutaneous extension.; b) Radiograph shows expansive lytic lesion of the distal phalanx.

Microscopy’s aspect of the giant cell tumour: multinucleated giant cells (osteoclast-like giant cells) and spindle shaped cells (Section stained with hematoxylin and Eosin).
Discussion
Giant cell tumour of the hand phalangeal bones are rare. GCT are usually benign but locally aggressive with bone and adjacent soft tissue destruction [2,3]. Metastases are rare, mainly pulmonary, and their risk can be increased by the number of recurrences [4,5]. GCT have slow development [3,5]. The metacarpal and phalangeal lesions represent a very rare localisation with less than 1% of all the sites [5]. To our knowledge, less than 100 cases of GCT of the hand phalangeal were described [6,7]. Patients are often in the fourth decade. Our presentation is particular because of the advanced age of our patient. Symptoms are dominated by pain, swelling and skin involvement. The diagnosis of GCT is suggested on the standard radiograph (X-ray) showing typically lytic and swollen lesion, aspects of honeycomb rather in the aggressiveness of the tumour [7]. CT and MRI are not common practice for diagnosis. They are performed in case of suspected malignancy to determine local extension. If clinical and radiographic aspects are not suggestive, such as for our patient, pathological examination is essential to confirm the diagnosis and to study the evolution of the tumour [2,5]. The main differential diagnosis is giant cell granulomas and aneurysmal bone cyst [5,8]. GCTs treatment involves several therapeutic methods. Curettage with bone grafts presents a risk of local recurrence in the order of 87%, which makes it ineffective [9]. Surgical cement is also used after curettage [2]. Cryotherapy associated with curettage has been proposed by other authors to reduce the risk of recurrence [5,10]. Although, amputation remains a mutilative method both functionally and aesthetically, it is useful especially in distal locations and for aggressive tumors [11]. In our case, only a limited amputation was performed with no recurrence or metastasis until 24 months follow up.
Conclusion
Until the location of GCT in the metacarpal bones is rare and its development is slow, surgery is recommended. The level of amputation will be as limited as possible depending on age and medical history of the patient.
[1]. Enneking WF, Spanier SS, Goodman MA, A system for the surgical staging of musculoskeletal sarcomaClin Orthop Relat Res 1980 (153):106-20.10.1097/00003086-198011000-00013 [Google Scholar] [CrossRef]
[2]. Ouarab M, Hattoma N, Ouali Idrissi M, Hachimi K, Trafeh M, Giant cell tumor of the third metacarpal bone: a case reportChir Main 2003 22(3):158-62.10.1016/S1297-3203(03)00042-8 [Google Scholar] [CrossRef]
[3]. Saikia KC, Bhuyan SK, Borgohain M, Saikia SP, Bora A, Ahmed F, Giant cell tumour of bone: an analysis of 139 Indian patientsJ Orthop Sci 2011 16(5):581-88.10.1007/s00776-011-0033-721833611 [Google Scholar] [CrossRef] [PubMed]
[4]. Lopez-Barea F, Rodriguez-Peralto JL, Garcia-Giron J, Guemes-Gordo F, Benign metastasizing giant-cell tumor of the handClin Orthop Relat Res 1992 (274):270-74.10.1097/00003086-199201000-00027 [Google Scholar] [CrossRef]
[5]. Ropars M, Kaila R, Cannon SR, Briggs TWR, Primary giant cell tumours of the digital bones of the handJ Hand Surg Eur Vol 2007 32(2):160-64.10.1016/J.JHSB.2006.11.00917222953 [Google Scholar] [CrossRef] [PubMed]
[6]. Saikia KC, Bhuyan SK, Goswami S, Bora A, Rare site giant cell tumors: report of two cases on phalanges of the finger and review of literatureJ Orthop Traumatol 2009 10(4):193-77.10.1007/s10195-009-0067-119787427 [Google Scholar] [CrossRef] [PubMed]
[7]. De Medeiros FC, de Medeiros FC, de Campos Carvalho Lopes I, Medeiros GC, de Medeiros EC, Giant cell tumor in the proximal phalanx with pulmonary metastasis: case report and literature reviewRev Bras Ortop 2015 46(2):205-10.10.1590/S0102-3616201100020001627027012 [Google Scholar] [CrossRef] [PubMed]
[8]. Gouin F, Grimaud E, Redini F, Moreau A, Passuti N, Heymann D, Metatarsal giant cell tumors and giant cell reparative granuloma are similar entitiesClin Orthop Relat Res 2003 (416):278-84.10.1097/01.blo.0000093016.90435.f614646771 [Google Scholar] [CrossRef] [PubMed]
[9]. Prashant K, Bhattacharyya TD, Frank H, Ram P, An unusual case of giant cell tumor of first metatarsal: a rare case report and review of literatureJ Orthop Case Rep 2016 6(5):03-06. [Google Scholar]
[10]. Wittig JC, Simpson BM, Bickels J, Kellar-Graney KL, Malawer MM, Giant cell tumor of the hand: superior results with curettage, cryosurgery and cementationJ Hand Surg Am 2001 26(3):546-55.10.1053/jhsu.2001.2252511418922 [Google Scholar] [CrossRef] [PubMed]
[11]. Slesarenko YA, Sampson SP, Gould ES, Giant cell tumor of the distal phalanx of the handHand Surg 2005 10(2-3):289-91.10.1142/S021881040500276016568530 [Google Scholar] [CrossRef] [PubMed]