Early Intestinal Obstruction in Iron Toxicity – An Unheard of Occurrence
Bharadhwaj Ravindhran1, K Karthikeyan2, Vivekanandan Jayakumar3, Nivedita Mitta5, SG Subramanyam5
1 Junior Resident, Department of Surgery, St John’s Medical College Hospital, Bengaluru, Karnataka, India.
2 Assistant Professor, Department of Surgery, St John’s Medical College Hospital, Bengaluru, Karnataka, India.
3 Senior Resident, Department of Surgery, St John’s Medical College Hospital, Bengaluru, Karnataka, India.
4 Assistant Professor, Department of Surgery, St John’s Medical College Hospital, Bengaluru, Karnataka, India.
5 Professor and Head, Department of Surgery, St John’s Medical College Hospital, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bharadhwaj Ravindhran, 123 Richfield Apartments, Outer Ring Road, Marathahalli, Bengaluru-560037, Karnataka, India.
E-mail: bharadhwaj.r@stjohns.in
Deliberate self-harm by overdosing on iron tablets although rare is an emergency and requires early recognition and intervention. We present the case of a 19-year-old girl who presented with abdominal distension, colicky abdominal pain, obstipation and intractable vomiting two days after an attempt at deliberate self-harm with ingestion of 30 iron tablets. She was admitted at another hospital, underwent gastric lavage and was monitored in their intensive care unit (ICU) for two days following which she was asymptomatic at discharge. At our hospital, abdominal radiographs showed multiple air fluid levels and dilated bowel loops. CECT showed focal thickening of the distal ileum with luminal occlusion, mesenteric hyperemia and fat stranding. She made complete recovery after conservative management with bowel rest, Deferoxamine (DFO) therapy and supportive care. Segmental enteritis caused by iron ingestion has not been well described and its sequelae causing luminal occlusion leading to intestinal obstruction within a week is very rare. Due to the infrequent occurrence of this condition and lack of evidence, management of intestinal obstruction following iron toxicity is case based. However, rigorous monitoring and follow up until complete resolution of symptoms is essential.
Deliberate self-harm, Ferrous sulphate, Segmental enteritis
Case Report
A 19-year-old female patient presented to the emergency room with complaints of abdominal distension, colicky abdominal pain, obstipation and intractable vomiting for a day. She gave history of deliberate self-harm by consuming 30 iron tablets (335 mg strength with 100 mg elemental iron) following an altercation with her family. Total dose ingested was 3000 mg (~46 mg/kg). She was taken within an hour of consumption to a nearby healthcare facility and underwent gastric lavage and supportive care with no record of deferoxamine administration. She was admitted in their ICU for observation and discharged after two days on supportive medications. She was reportedly well until 12 hours after discharge when she noticed colicky lower abdominal pain followed by abdominal distension, obstipation and persistent vomiting.
The patient was drowsy, tachycardic, hypotensive and tachypneic at admission. She had crepitations over bilateral infra-axillary and infra scapular areas. The cardiovascular system was unremarkable. Examination of the abdomen revealed distension, supra pubic and right iliac fossa tenderness and absent bowel sounds with no overt signs of peritonism. Per-rectal and per-vaginal examinations were also normal. The arterial blood gas revealed elevated lactate levels of 3.2 and compensated metabolic acidosis. She was resuscitated and admitted under our ICU for further management.
Laboratory investigations revealed leukocytosis (20,752/μL) with Neutrophilia (91%), elevated prothrombin time (19 seconds), INR of 1.6, conjugated hyperbilirubinemia (total bilirubin – 6.5 mg/dL and conjugated = 4.85 mg/dL), AST – 98 IU/L, ALT – 737 IU/L, ALP – 82 IU/L, GGT – 59 IU/L. Serum Iron level was 340 μg/dL, ferritin level was 4759 ng/mL, percentage saturation was 39 and TIBC was 96 μg/dL. The plasma ammonia levels were 57 μmol/L, blood glucose level of 156 mg/dL, blood urea of 58 mg/dL and Creatinine of 1.3 mg/dL. Serum and urine toxicology screening was negative for paracetamol, opiates benzodiazepines, or ethanol.
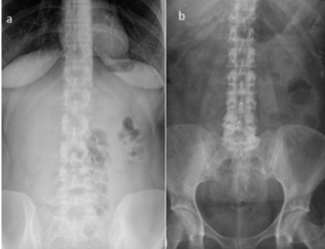
An acute abdominal series was done which showed no residual tablets, but showed multiple air fluid levels in the erect film and grossly dilated small bowel loops in the supine film [Table/Fig-1]. CECT scans were performed which revealed dilated jejunal and ileal loops with maximum calibres of 4 cm and 3.2 cm respectively. Multiple air fluid levels were noted. The distal ileum showed focal thickening with hyper enhancement causing occlusion of the lumen with mesenteric hyperemia and fat stranding. No obvious transition point was noted. Small bowel was dilated until the terminal ileum with collapsed large bowel. Minimal free fluid was noted in the right Para-colic gutter [Table/Fig-2].
a) Erect X-ray of the abdomen showing multiple air fluid levels; b) supine X-ray of the abdomen showing multiple dilated small bowel loops.

a,b) Contrast enhanced CT scans revealed dilated jejunal and ileal loops with distal ileum showing focal thickening with hyper enhancement causing occlusion of the lumen Mesenteric hyperemia, fat stranding and; c) multiple air fluid levels were also noted.

She was monitored in our ICU and was started on deferoxamine dose of 5 mg/kg/hour for the first 24 hours. Empirical antibiotics and supportive care was started. She was intubated in view of respiratory distress shortly after admission into the ICU and was managed conservatively with adequate hydration and bowel rest.
Her arterial blood gas improved gradually over the next 24 hours, she was extubated and did not require oxygen supplementation there after. The repeat investigations also showed improvement, with a decreasing total white cell count (15,100/μL), prothrombin time of 15 seconds and an INR of 1.3. The liver function also showed improvement with a decrease in enzyme levels and bilirubin values. The repeat serum iron levels were 230 μg/dL and ferritin levels were 3560 ng/mL,% saturation of iron was 35 and TIBC was 122 μg/dL. She was shifted out of the ICU in view of hemodynamic stability and improvement of her metabolic profile. No haemodialysis or exchange transfusion was planned due to improvement of symptoms.
She improved symptomatically; the abdominal distension and pain gradually subsided. She was started on clear fluids on day 4 of hospitalisation. Repeat X-rays showed no air fluid levels or dilated bowel loops [Table/Fig-3]. She was gradually started on diet which she tolerated well. The repeat investigations showed improvement with a total serum iron of 144 μg/dL, TIBC of 152 μg/dL, % saturation of 28.4, ferritin level of 965 ng/mL, total bilirubin of 1.64 mg/dL and conjugated bilirubin of 1.42 mg/dL. She underwent upper GI endoscopy which was normal. She was discharged on day 8 of hospitalisation. She underwent colonoscopy after three weeks which showed few mucosal erosions in the ascending colon. She was reviewed on outpatient basis after six weeks and had made complete recovery.
Repeat abdominal X-rays taken after one week - supine (a) and erect (b) showing resolution of dilated bowel loops and air fluid levels.
Discussion
Iron-induced tissue damage is mainly caused by free radical production and lipid peroxidation [1]. Toxic effects of iron on cells include mucosal necrosis, inhibition of enzymatic processes especially of the Kreb’s cycle, uncoupling of oxidative phosphorylation, disruption of the mitochondrial lipid membrane, direct vasodilation and inhibition of serum proteases [2-6]. Classically five phases of clinical manifestations have been described which usually overlap. Namely the GI phase (<6 hours), latent phase (6 to 24 hours). Shock phase with metabolic derangement (4hours to 4 days), the hepatotoxic phase (<2 days) and bowel obstruction (2 to 4 weeks). The iron from circulation is cleared rapidly (<8 hours) and is deposited in tissues where chelation is not completely effective [1,7]. A dose greater than 30 mg/kg may be potentially toxic, as in our patient [8].
Our patient initially presented with symptoms suggestive of the GI phase after which she was temporarily better. However she later exhibited signs of the shock phase and uncharacteristic early symptoms of bowel obstruction. While most of the complications following iron overload/toxicity have been adequately described in literature, Iron induced bowel obstruction has seldom been described. Symptoms of bowel obstruction appearing earlier than a week after iron ingestion has never been described so far, to the best of our knowledge. Morse SB et al., had reported a unique case in which a 13 months old child with ingestion of >100 mg/kg of iron tablets passed away in less than 13 hours prior to presentation. The case also reported that the patient’s three year old sibling was also evaluated for overdose following ingestion of prenatal vitamins and iron tablets 12 hours earlier and dealt with the need for emergency physicians to enquire about other children at home, in order to avoid preventable tragic consequences [4].
The initial CT scans of our patient revealed features suggestive of intestinal obstruction secondary to possible segmental enteritis caused by iron ingestion. She gradually improved with conservative management including DFO therapy, bowel rest, adequate hydration and supportive care. The administration of steroids was contemplated to reduce the mucosal oedema, which was thought to be the cause of intestinal obstruction. However, steroids were not given and DFO therapy was given only for the first 24 hours.
Acute iron overdose or toxicity in adults is infrequent and occurrences are sporadic, which may be the reason for lack of evidence based management. Therefore, management of iron toxicity is case based. The symptomatology although well described is highly variable. Segmental enteritis caused by iron ingestion has not been well described and its sequelae causing intestinal obstruction has not been described thus far.
Conclusion
Iron toxicity is an emergency which requires early recognition and intervention. The symptoms of iron toxicity may present in two stages like in our patient and therefore, rigorous monitoring and follow up until complete resolution of symptoms is imperative. Segmental enteritis presenting as intestinal obstruction following iron ingestion although rare must be kept in mind. Conservative management may be attempted in such patients with rigorous monitoring, GI decompression, DFO therapy and supportive care.
[1]. Tenenbein M, Toxicokinetics and toxicodynamics of iron poisoningIn: Toxicology Letters 1998 :653-56.10.1016/S0378-4274(98)00279-3 [Google Scholar] [CrossRef]
[2]. Mills KC, Curry SC, Acute iron poisoningEmerg Med Clin North Am 1994 12(2):397-413. [Google Scholar]
[3]. Viers BR, Boorjian SA, Frank I, Tarrell RF, Thapa P, Karnes RJ, Pretreatment Neutrophil-to-Lymphocyte Ratio Is Associated with Advanced Pathologic Tumor Stage and Increased Cancer-specific Mortality Among Patients with Urothelial Carcinoma of the Bladder Undergoing Radical CystectomyEur Urol 2014 66(6):1157-64.10.1016/j.eururo.2014.02.04224630414 [Google Scholar] [CrossRef] [PubMed]
[4]. Morse SB, Hardwick WE, King WD, Fatal iron intoxication in an infantSouth Med Journal 1997 90(10):1043-47.10.1097/00007611-199710000-000159347819 [Google Scholar] [CrossRef] [PubMed]
[5]. Walker SE, Paton TW, Cowan DH, Manuel MA, Dranitsaris G, Bioavailability of iron in oral ferrous sulfate preparations in healthy volunteersCMAJ 1989 141(6):543-47. [Google Scholar]
[6]. Robotham JL, Lietman PS, Acute iron poisoning. A reviewAm J Dis Child 1980 134(9):875-79.10.1001/archpedi.1980.021302100590166998282 [Google Scholar] [CrossRef] [PubMed]
[7]. Little M, Toxicology emergencies. In: Cameron P, Jelinek G, Kelly A-M, Brown A, Little M, edsTextbook of Adult Emergency Medicine 2015 4th edPhiladelphia, PAElsevier Churchill Livingstone:996-97.chap 29 [Google Scholar]
[8]. Madiwale T, Liebelt E, Iron: not a benign therapeutic drugCurr Opin Pediatr 2006 18(2):174-79.10.1097/01.mop.0000193275.62366.9816601499 [Google Scholar] [CrossRef] [PubMed]