Cerebral palsy is an early life neurological disorder that occurs due to injury or abnormal development of foetus brain. Among the spastic cerebral palsy children, 22% suffer from hemiplegia [1]. Hemiplegic Cerebral Palsy (HCP) presents with muscle paralysis, movement dysfunctions and abnormal deformity to one side of the body [2]. These primary impairments produce the secondary impairments such as muscle weakness and contracture that affects hand function in HCP children. The tactile sensory dysfunction additionally contributes the reduction of the upper limb motor function in HCP children. Defective thalamocortical projections are one of the most common primary pathophysiologies for the sensory disturbance in HCP children. Later, the HCP child tends to develop poor registration of tactile and proprioceptive sensory function as consequences of both motor and sensory problems. Poor registration of tactile and proprioceptive sensory information affects grasping and releasing the objects in HCP children which are essential for dexterous manipulation and activities of daily living [3-6]. Over the period of time, the HCP children develop “learned non-use” of the hemiplegic side for activities of daily living [7].
Constraint-Induced Movement Therapy (CIMT) and hand arm bimanual intensive training are best among the goal-oriented activities to improve upper limb function in HCP children [8]. Task-Oriented Training (TOT) is a neurological approach, which practices the repetitive and meaningful goal-oriented activities to improve the voluntary function of the hemiparetic side. It is easy to practice and it improves the upper limb functions such as reaching, grasping, releasing and other activities of daily living in HCP children [2,9]. Compared with other intensive therapies, TOT gains some advantages in feasibility and continuous active participation aspects in cerebral palsy management [10]. However, TOT also has the major concern to improve the motor recovery and there is no evidence available on sensory function recovery in HCP children.
Therapists use the sensory intervention to manage many adult neurological disorders by either individual sensory facilitation techniques or combined with other sensory function or motor function training [11,12]. This type of training is generally called as Sensorimotor Training (SMT). The SMT aimed to improve motor response by increasing sensory input in dynamic environments [13].
Similarly, little evidence has showed administration of somatosensory electrical stimulation improving motor learning in normal human and stroke patients [14-16]. Kita K et al., found the usefulness of TENS in stroke patients to manage the sensory deficit [17]. TENS is cheap and easily available in all physiotherapy practice [18]. Even though the rising evidence for TENS as motor control intervention in cerebral palsy children are available [19,20], but the safety and efficacy were remained unanswered. Due to that, a preliminary study was conducted by Satheeskumar D et al., which reported that TENS is a safe and feasible intervention to manage in hemiplegic cerebral palsy children [21].
Sakzewski L et al., stated no similarity among the intensive models of upper limb intervention in HCP children [10]. Combination therapies are effective to improve motor functions and are becoming popular in the management of cerebral palsy children [22]. There were no studies found that combined TENS with Sensorimotor Training and Task Oriented Training (SM-TOT) to improve the hand function and explored the sensory role of TENS in HCP children. So, this study was hypothesised by combining the TENS with SM-TOT to augment the HCP children’s hand function in multi-factorial (sensory, motor and functional) aspects. Thus, this study was aimed to find out the effectiveness of TENS combined with SM-TOT to improve hand function in HCP children.
Materials and Methods
This was a randomised, placebo-controlled and multi-centered study design. This study was conducted at K.S Hegde Charitable Hospital, Mangaluru, Karnataka, India and P.P.G. College of Physiotherapy Hospital and Ashwin Multispecialty Hospital, Coimbatore, Tamil Nadu, India, from March 2014 to November 2016. Total 60 spastic HCP children of both male and female, ages between four to 12 years and who responded to 4.56 log of Semmes-Weinstein Monofilament (SWM) were included in this study [23]. We excluded the children who scored more than three on five point scale of Modified Ashworth (MAS) [24], the Manual Ability Classification System (MACS) for children with cerebral palsy and communication function classification system for the individual with cerebral palsy [25,26]. The children with a history of epilepsy, undergone any antispastic drugs, botulinum toxin injection, orthopaedic surgery or neurosurgery within the past 12 months were also not included in this study. This study adhered to regulations of Institutional Central Ethical Committee and informed consents were obtained from HCP children’s parents before the start of the interventions.
The sample size was calculated by using G-power software (3.1 version). The calculated effect size was 0.34 according to the pilot data. The calculated sample size was 54 after applied power at 80% and significance level at 0.05. So the total sample size was set as 60, including the 10% of drop out.
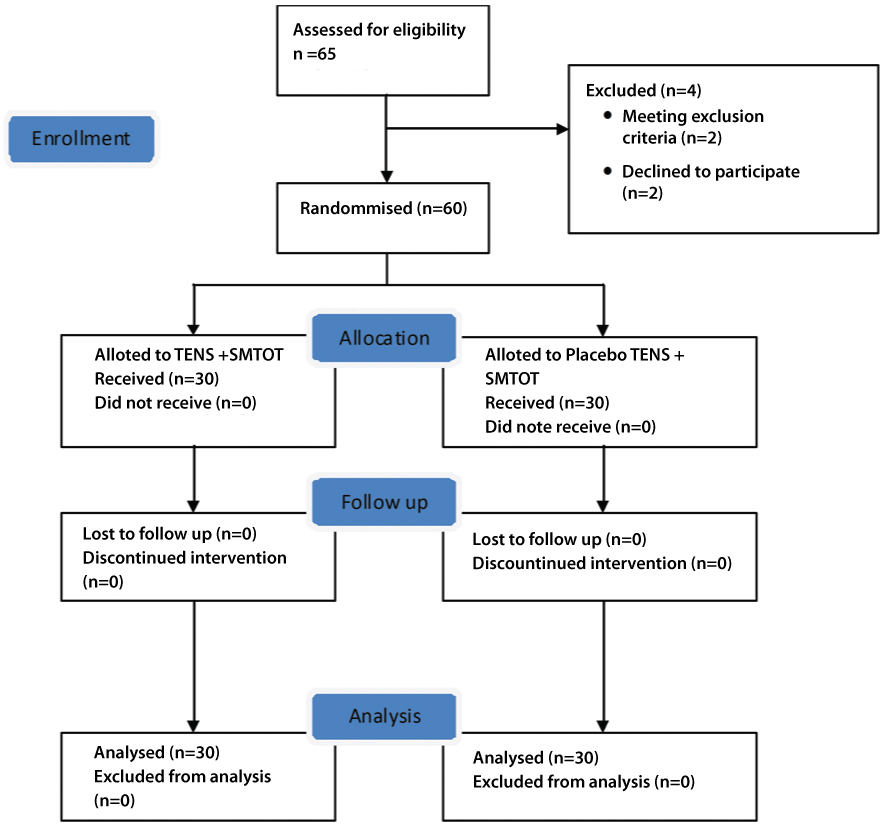
The study procedure was given in CONSORT flow diagram [Table/Fig-1]. Total 60 HCP children were allotted randomly into two groups by using generated random numbers. The randomisation was stratified according to age wise to maintain the similarity between the groups. The Group-A received TENS with SM-TOT and the Group–B received Placebo-TENS with SM-TOT. The research intervention as per group allotment was provided by the clinical physiotherapist for three days per week for continuous eight weeks. Pre-test and post-test measures were evaluated by an experienced physiotherapist who is blinded to group allotment. The group allocation was blinded to parents also.
Flow chart according to CONSORT guidelines.
TENS-Transcutaneous Electrical Nerve Stimulation, SM-TOT-Sensorimotor Training and Task Oriented Training
Intervention
The experimental protocol for Group-A started with TENS for 60 minutes by using TENS (DigiTENS pro-BMS) machine at the parameters of pulse frequency 100 Hz, pulse width 200 μs and two to three times of sensory threshold. The pair of electrodes was placed over forearm flexor and extensor group muscles. The sensory threshold was determined by increasing intensity of TENS current from 0.01 mA until the subject felt the initial current sensation. The threshold level of the intensity was confirmed by using children anxiety and pain scale to confirm the child’s comfort level [27]. The SM-TOT consisted two sections, first 30 minutes of specific sensory-motor training was focussed on tactile discrimination function. Identification, exploring and matching games were given by using familiar texture and shapes to train the tactile discrimination function. Initially, all subjects received visual guidance which was reduced gradually in subsequent training sessions. Remaining 30 minutes practiced TOT to improve unilateral and bilateral upper limb functions in HCP children. Paralysed arm function focussed on holding a cup, drinking water, eating snacks from a plate and taking a dice out of a container. Bimanual arm function focussed on wrapping/unwrapping the chocolate, zipping up down jacket and unscrewing a bottle cap. Activities were selected after the detailed analysis and mutual agreement with the parents/caregiver. The unaffected side upper limb was blocked during the paretic arm function exercises. Children were asked to repeat the selected sensory–motor task for a minimum of 20 trials. Who all completed the task faster was asked to do more repetition, up to a maximum of 30 times. The verbal, visual and tactile sensory guidance were given at initial and during the performance. The sensory feedback was given at end of each task. The sensory advice was reduced day by day after the improvements. This protocol was followed for three days per week for eight weeks.
The Group-B received placebo-TENS with SM-TOT for three days in a week for eight weeks. The placebo-TENS was given for 60 minutes by not delivering current but the beep sound of the timer was kept on to assure the TENS machine was running. The children was instructed as they could not possibly feel the TENS stimulation. The SM-TOT protocol was followed similar to Group-A.
The home based CIMT protocol added along with group’s intervention program to maintain the learned task oriented movements [28]. Custom made garment was provided to reduce the unaffected hand participation during the task training. All children were encouraged to wear this garment during training at home for a minimum of two hours per day for five days in a week for eight weeks. All these therapy details were maintained in given daily log. The daily log was given by principal investigator to parents and it was focussed on the feasibility of all treatment protocol, missing of any treatment schedule or any other side effects due to the treatment protocol.
Outcome Measures
Tactile Registration (TR) was measured with 2.83 size filament to apply pressure three times over the pulp of thumb, index, ring and little finger randomly by using 20 set kit of SWM. The least size monofilament was identified by asking the child to respond in all selected fingers accurately. The Tactile Localisation (TL) was measured by using the large size SWM pressed over front or back or side of the thumb, index, ring and little finger for 12 times. The correct response out of 12 times was noted. Two-Point Discrimination (TPD) was measured by asking the child to identify the least size of two point contact by using Disk-Criminator [29]. Stereognosis (STG) was tested by asking the name of the known 12 objects with eyes closed and the correct response were recorded out of 12 attempts [30]. Nine-Hole peg test (NHPT) was used to measure the dexterity skill by recording the time taken to complete the task [31]. Grasp domain of the Quality of Upper Extremity Skill Test (QUEST) was used to assess the grasp (unimanual) function of HCP children and ABILHAND-Kids questionnaire was used to analyse the utilisation of both upper limb (bimanual) functions for the activities of daily living [32,33].
Statistical Analysis
Statistical analysis was performed by using the SPSS 22.0. Demographic information was summarised using means, standard deviations, and frequency. Descriptive analysis was performed by using Independent t-test and Chi-square test for the baseline value. Inferential statistics performed by using Paired t-test and Wilcoxon Signed rank test for within group comparison and independent t-test and Mann-Whitney U test for between groups comparison. The significance level was set at p <0.05.
Results
The demographic characteristic and baseline values of 60 participants are described in [Table/Fig-2].
Baseline characteristics of both groups.
| Group | | TENS+SM-TOT | Placebo-TENS +SM-TOT |
|---|
| No. of subjects | (n) | 30 | 30 |
| Age | Mean±SD | 6.02±1.95 | 6.5±1.89 |
| Gender | Male (n) | 21 | 17 |
| Female (n) | 9 | 13 |
| Hemiparetic side | Right | 15 | 20 |
| Left | 15 | 10 |
| MAS | Score 1 | 4 | 6 |
| Score 2 | 12 | 8 |
| Score 3 | 14 | 16 |
| MACS | Level I | 4 | 9 |
| Level II | 18 | 14 |
| Level III | 8 | 7 |
| Tactile registration | Mean±SD | 7.03±1.16 | 6.4±1.57 |
| Tactile localisation | Mean±SD | 8.9±1.42 | 9.3±1.29 |
| Two point discrimination | Mean±SD | 6.2±1.28 | 5.8±1.29 |
| Stereognosis | Mean±SD | 6.03±1.73 | 6.9±1.07 |
| Nine-hole peg test | Mean±SD | 123.6±24.9 | 118.5±28.2 |
| QUEST-Grasp | Mean±SD | 19.5±6.51 | 18.4±4.86 |
| ABILHAND-Kids Questionnaire | Mean±SD | 26.56±6.09 | 27.82±6.28 |
Abbrevations: TENS–Transcutaneous electrical nerve stimulation; SM-TOT–Sensorimotor task oriented training; n–Number of participant; SD-Standard deviation; MAS–Modified ashworth’s scale; MACS–Manual ability classification system; QUEST–Quality of upper extremity skill test.
The [Table/Fig-2] shows that there was no significant difference found between the groups in age, gender, hemiplegic side, MAS and MACS. No significant difference was found between groups in TR, TL, TPD, STG, NHPT, QUEST and ABILHAND-Kids score at baseline measure. The log book of treatment dairy showed that none of the patients missed the treatment session and parents were able to continue the prescribed exercise in the home environment. These indicate that the TENS combined with SM-TOT is feasible to apply in upper limb rehabilitation of HCP children.
Sensory Functions after the Intervention
The statistical analysis of both group’s sensory functions is showed in [Table/Fig-3]. Group–A showed the mean improvement in TR (1.3), TL (1.9), TPD (1.5) and STG (1.34) score after the eight weeks of TENS with SM-TOT and it was statistically significant at p <0.05 level. Likewise, Group-B showed the mean improvement in TR (0.8), TL (0.97), TPD (1.23) and STG (1.34) score after the eight weeks of TENS with SM-TOT. These mean improvement score was statistically significant at p <0.05 level.
Comparison of sensory function in both groups.
| Sensory component | Group | n | Pretest (Mean±SD) | Posttest (Mean±SD) | Within group comparison | Between groups comparison |
|---|
| MD | p-value | MD | p-value |
|---|
| Tactile registration | TENS+SM-TOT | 30 | 7.03±1.16 | 5.73±1.08 | 1.3 | 0.001* | 0.5 | 0.013* |
| Placebo-TENS+SM-TOT | 30 | 6.43±1.57 | 5.63±1.43 | 0.8 | 0.001* | |
| Tactile localisation | TENS+SM-TOT | 30 | 8.9±1.42 | 10.8±1.36 | 1.9 | 0.001* | 0.93 | 0.003* |
| Placebo-TENS+SM-TOT | 30 | 9.27±1.29 | 10.2±1.27 | 0.97 | 0.001* | |
| Two point discrimination | TENS+SM-TOT | 30 | 6.23±1.28 | 4.73±1.26 | 1.5 | 0.001* | 0.27 | 0.328 |
| Placebo-TENS+SM-TOT | 30 | 5.8±1.29 | 4.57±1.14 | 1.23 | 0.001* | |
| Stereognosis | TENS+SM-TOT | 30 | 6.03±1.73 | 7.37±1.75 | 1.34 | 0.001* | 0.26 | 0.251 |
| Placebo-TENS+SM-TOT | 30 | 6.97±1.07 | 8.57±0.57 | 1.6 | 0.001* | |
Abbreviations: TENS–Transcutaneous electrical nerve stimulation; SM-TOT–Sensorimotor task oriented training; n–Number of participant; SD-Standard deviation; MD–Mean difference.
*Significant difference at p<0.05
Upper Limb Functions after the Intervention
Group-A showed the mean improvement of 16.47 in NHPT, 6.26 in QUEST and 2.89 in ABILHAND-Kids score. These improvements were statistically significant at p <0.05 level. Even, the Group-B showed mean improvement of 13.53 in NHPT, 2.83 in QUEST and 2.07 in ABILHAND-Kids score and these improvements were statistically significant at p <0.05 level. Group-A showed the mean improvement of 2.94 in NHPT and 3.43 in QUEST score than Group-B at the end of eighth week. These scores were statistically significant with p-value <0.05. However, the Group–A showed the mean improvement of 0.82 than Group-B in ABILHAND-Kids score and it was not statistically significant at p <0.05 level. These details are summarised in [Table/Fig-4].
Comparison of hand function in both groups.
| Functional component | Group | n | Pretest (Mean±SD) | Posttest (Mean±SD) | Within groups comparison | Between groups comparison |
|---|
| MD | p-value | MD | p-value |
|---|
| Nine-Hole Peg Test | TENS+SM-TOT | 30 | 123.6±24.9 | 107.1±24.9 | 16.47 | 0.001* | 2.94 | 0.031* |
| Placebo-TENS+SM-TOT | 30 | 118.5±28.1 | 104.9±26.9 | 13.53 | 0.001* |
| Grasp–QUEST (unimanual function) | TENS+SM-TOT | 30 | 19.59±6.51 | 25.85±7.78 | 6.26 | 0.001* | 3.43 | 0.003* |
| Placebo-TENS+SM-TOT | 30 | 18.41±4.86 | 21.24±6.58 | 2.83 | 0.001* |
| ABILHAND-Kids Questionnaire (Bimanual function) | TENS+SM-TOT | 30 | 26.56±6.09 | 29.45±6.79 | 2.89 | 0.001* | 0.82 | 0.120 |
| Placebo-TENS+SM-TOT | 30 | 27.82±6.28 | 29.89±6.34 | 2.07 | 0.001* |
Abbreviations: TENS–Transcutaneous electrical nerve stimulation; SM-TOT–Sensorimotor task oriented training; n–Number of participant; SD-Standard deviation; QUEST–Quality of upper extremity skill test.
*Significant difference at p<0.05 level
Discussion
This study focussed on to find the effect of TENS combined with SM-TOT to improve hand function in HCP children. According to the available literature evidence, I believed that the TENS create enriched sensory information to enhance the motor learning process. Due to this reason, the TENS intervention was incorporated to administer along with SM-TOT. The carefully selected HCP children were divided into two groups. Each group was followed by the specified protocol for eight weeks of intervention. This protocol was novel and child-centric. Similar to the preliminary study reports, this study found that all the children participated actively and also the parents well implemented the prescribed treatment protocol in a home environment [21]. The SWM was useful to reproduce the results in an accurate manner to measure the improvement in HCP children’s TR and TL functions [34]. This study, probably is the first to register the effectiveness of TENS combined with SM-TOT to improve hand function in HCP children.
Sensorimotor Task-Oriented Training
Organising and implementing the SM-TOT was challenging to the therapist. Identification of suitable task and setting the criteria for the task to carry out in the home environment was an important factor to improve hand function in HCP children. All of the prescribed tasks were well adapted, met the functional level of each individual and tested the emerging skills of hand function in HCP children. This study results also showed an observable sensory-motor improvement in upper limb function of moderate sensory disturbed HCP children in both groups. This proved that the sensory motor intervention has a definitive role to improve the hand function in HCP children. Similar to this study, Choi KS and Lo KH showed the visual and haptic cues improved the handwriting skill in cerebral palsy children [35]. Even Robert MT et al., reinforced this study finding by strongly supporting the relation between the sensory status of children and faster response in motor skill learning, which can be transferred to similar movement patterns [36].
TENS Combined with Sensorimotor Task-Oriented Training on Sensory Functions
The mean improvement score of TR, TL, two point discrimination and STG were respectively 1.3, 1.9, 1.5 and 1.34. Among these results, the TR and TL score of Group-A showed significant improvement than Group-B. This proves that the eight weeks of TENS combined with SM-TOT is effective to improve the upper limb TR and TL in HCP children. Kattenstroth JC et al., explained that the repetitive sensory stimulation improved the motor performance by altering the sensory threshold and improving other multiple sensory functions in chronic cerebral lesion patients [37]. In another study, Kita K et al., explained that the sensory level stimulation of TENS achieved the higher level manual dexterity function by increasing the feedback control loop in stroke patients [17]. The TPD and STG are the strong factors to determine the improvement in paralysed side spatial tactile perception function [6]. However, this study showed similar pattern of improvement in TPD and STG in HCP children after eight weeks of intervention in both groups. TENS current applied at single point of skin could create more tactile awareness from the point of contact rather than proprioceptive and fine force differentiation control [38,39]. These might be the reason that TENS did not create a major impact in TPD and STG function. So, these results must be analysed in detail to explore the TENS efficacy to improve upper limb sensory function in HCP children.
TENS Combined with Sensorimotor Task-Oriented Training on Motor Functions
The Group-A children showed a significant improvement in NHPT and grasp function of QUEST score than Group-B. This result demonstrated that the hand function of HCP children improved after the eight weeks of TENS combine with SM-TOT training. These details are given in [Table/Fig-4]. This study result supported by Conforto AB et al., by showing that the peripheral sensory stimulation delivered at subsensory level triggered the excitability at the motor cortex and intracortical regions. This excitation facilitated the motor training and modulated the motor function in subacute stage of stroke patients. These effects were also maintained after 30 days of the intervention [16]. This study was further supported by Veldman MP et al., by showing 6% of improvement in motor skill performance after the somatosensory electrical stimulation was added with motor practice in healthy adults [14]. Similar to this finding, this study result also showed that the TENS is one of the important supportive interventions to improve grasp (unimanual motor) function in HCP children. Even though, the HCP children showed statistically significant improvement in unimanual function and not in bimanual activities (ABILHAND-Kids Questionnaire) after eight weeks of TENS with SM-TOT training. This study’s SM-TOT training included more unilateral motor activities than bimanual activities and further TENS was achieved by mild improvement in spatial tactile perceptual function of paralysed side. These reasons would have reduced the bimanual activity improvement in ABILHAND-Kids questionnaire after the eight weeks of TENS with SM-TOT training compared with placebo TENS with SM-TOT training. This bimanual function results need to be addressed in detail in future studies.
Effects of Placebo TENS Combined with Sensorimotor Task Oriented Training
Placebo-TENS with the SM-TOT group showed an improvements in sensory and motor function but, not superior to the TENS with SM-TOT intervention. Borstad AL et al., highlighted the improvement of touch perception, wrist proprioception and shape discrimination in mild sensory disturbed stroke patients after the two weeks of sensory motor training [13]. And Kim Y and Lee BH showed the benefit of child-centered TOT to improve motor function in cerebral palsy children [40]. Like these previous studies, this study also used a comprehensive SM-TOT that could facilitate more neural information from upper limb receptor, create more awareness in the cerebral cortex and generate controlled motor pattern in HCP children. This proves that the SM-TOT has played an important role in facilitating sensory-motor function and placebo-TENS does not have an effect to improve sensory and motor function in HCP children.
Limitation
Transcutaneous electrical nerve stimulation combined with SM-TOT improved the TR function but the mechanism of the spatial tactile function improvement need to be analysed in future studies. Other factors such as spasticity level, different dosimetry and variety of cerebral palsy children are greater challenges for the TENS combined with SM-TOT protocol in future.
Conclusion
This study concluded that the TENS combined with SM-TOT is effective to enhance the hand function in HCP children. Moreover, the HCP children achieved faster recovery in few sensory motor functions when TENS was combined with SM-TOT. Therefore, further studies are required to evaluate the role of the TENS in enhancing sensory motor recovery in HCP children.
Abbrevations: TENS–Transcutaneous electrical nerve stimulation; SM-TOT–Sensorimotor task oriented training; n–Number of participant; SD-Standard deviation; MAS–Modified ashworth’s scale; MACS–Manual ability classification system; QUEST–Quality of upper extremity skill test.