Regenerative Endodontic Procedure: Clinical and Radiographic Evaluation of Two Cases
Monalisa Das1, Shabnam Zahir2, Gautam Kundu3
1 Clinical Tutor, Department of Dentistry, Murshidabad Medical College and Hospital, Berhampore, West Bengal, India.
2 Professor, Department of Paedodontics, Gurunanak Institute of Dental Science and Research, Kolkata, West Bengal, India.
3 Professor and Head, Department of Paedodontics, Gurunanak Institute of Dental Science and Research, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Monalisa Das, No. 2, Durganagar, Sripally, Chakdaha-741222, West Bengal, India.
E-mail: monalisa.das43@gmail.com
The regenerative endodontic procedures can re-establish the vitality of teeth to some extent and retain the physiological functions. The endodontic treatment of permanent as well as deciduous teeth supported with regenerative procedures, may be the treatment of choice in regular day-to-day practice. This procedure may help to abolish the era of dentistry practicing conventional endodontic treatment compromising the vitality of teeth. This article reports two cases of non-vital young teeth (each with different maturation of apices and periodontal health) treated with Lesion Sterilisation and Tissue Repair (LSTR) and revascularisation procedure.
Non-vital tooth Odontoblast, Sterilisation, Revascularisation
Case Report
Case 1
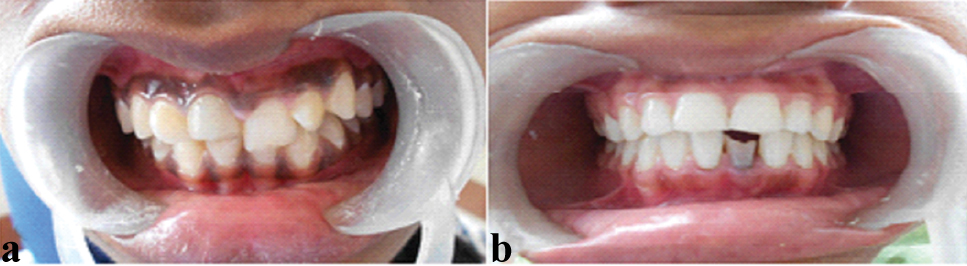
A 10-year-old boy reported with the complaint of discolouration of front tooth from one year. Patient gave history of sports injury five years back and was associated with mild pain and sensitivity. Clinical examination revealed Elli’s class IV fracture in relation to (i.r.t.) 11 [Table/Fig-1a].
Clinical presentation of case 1 and case 2.
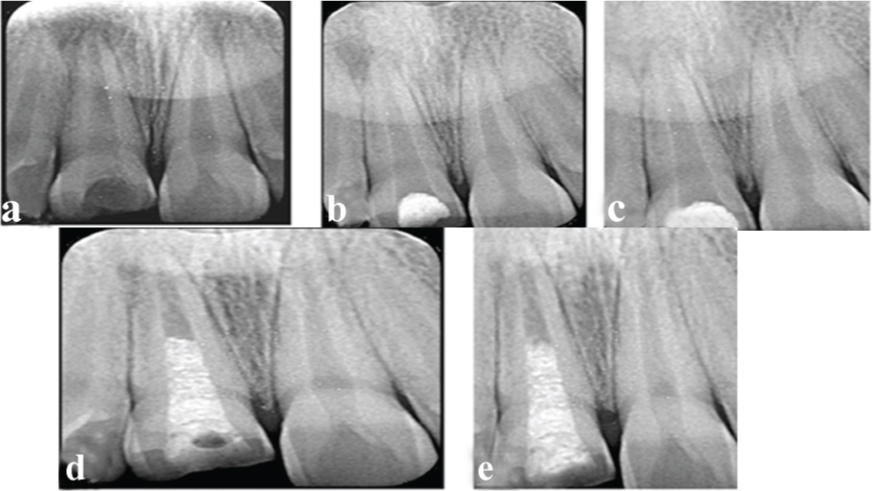
The tooth was irresponsive to pulp vitality test (thermal test). Intraoral Periapical Radiograph (IOPAR) showed periapical radiolucency i.r.t. 11, measuring approximately 4 mm in size with wide open apex. After thorough evaluation of the case and patient’s informed consent, LSTR procedure was planned followed by revascularisation. In the first appointment, access opening was done i.r.t. 11 under local anaesthesia. Necrotic tissue was removed and copious irrigation done with 5.25% sodium hypochlorite diluted with normal saline. After proper drying of the root canal, freshly mixed tri-antibiotic paste (ciprofloxacin, metronidazole and minocycline in 1:1:1 ratio as proposed by Hoshino E et al., in 1996) was inserted and temporary restoration placed [1]. The patient was recalled after 14 days and radiographic evaluation (IOPAR) was done. Sign of healing was noted in the periapical region of 11. Further, intracanal medicament was altered and the patient again recalled after 21 days. In the 3rd appointment, complete radiographic healing was observed and revascularisation procedure planned. A sterile 15 no. 25 mm K-file (Dentsply) was inserted periapically i.r.t 11 and rotated half a turn to induce fresh bleeding. A blood clot was produced to the level of the cementoenamel junction to provide a scaffold for the in growth of new tissue. The coronal portion of the root canal was sealed with Mineral Trioxide Aggregate (MTA) followed by composite restoration. The patient was followed up after one, six and 12 months and the tooth was found to be sound clinically and radiographically. There was evidence of radiographical root lengthening and root wall thickening in 6th and 12th month appointments [Table/Fig-2a-e].
a) Preoperative IOPAR of 11 (Case 1); b) Postoperative after 14 days; c) Complete radiographic healing after 21 days; d) Postoperative after 6 months; e) after 12 months.
Case 2
A 14-year-old girl reported with esthetic concern in the lower front tooth. She gave history of injury from hand pump at her early schooling age (six years). The tooth gradually turned black over a period of three years and was associated with mild, dull, spontaneous, intermittent pain which was relieved by medication taken from a local pharmacy. There was no history of blood or purulent discharge. On clinical examination, 41 were fractured, discoloured and irresponsive to heat and cold tests [Table/Fig-1b]. An IOPAR showed periapical radiolucency i.r.t. 41 with widening of periodontal space, horizontal bone loss and apex about to mature. Although, this was not an ideal case for LSTR and revascularisation, patient’s informed consent was taken for the same and an attempt made. Similar procedure was being followed as case 1 and complete radiographic healing was noted after 21 days. The revascularisation procedure was performed as done previously. The patient was followed up after one and six months and the tooth was found to be sound clinically. Radiographically, apical closure and root lengthening was not noted except root wall thickening. After a period of 12 months, radiographic examination revealed reappearance of periapical radiolucency and widening of periodontal spaces i.r.t. 41 with asymptomatic clinical findings [Table/Fig-3a-e].
a) Preoperative IOPAR of 41 (Case 2); b) Postoperative after 14 days; c) Complete radiographic healing after 21 days; d) Postoperative after 6 months; e) After 12 months showing recurrence of periapical pathology.
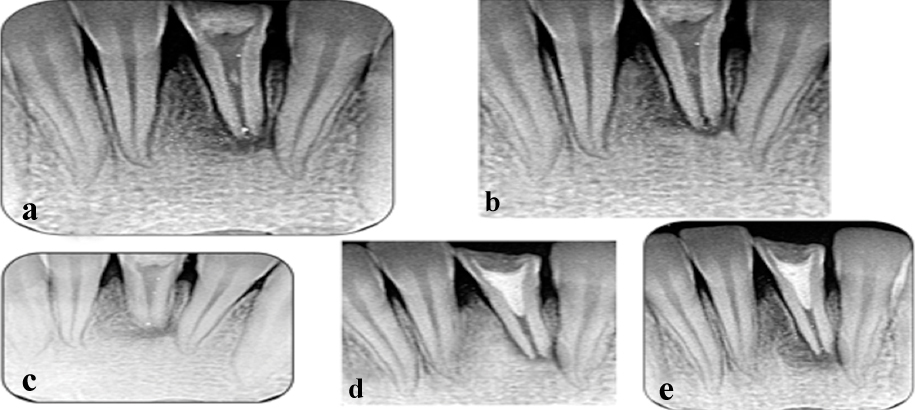
The focal source of infection was thought to be periodontal (widening of periodontal ligament space) and thorough oral prophylaxis performed. The patient was again recalled after a month but the periapical radiolucency persisted as before with no clinical symptoms.
Discussion
Over the past decades, endodontic treatments have shown a high rate of success in retention of teeth [1,2]. The disadvantage of this conventional treatment is mainly restoration of teeth without replacement of blood supply and innervations. The increased brittleness of the teeth ultimately results in premature loss, therefore diminishing the quality of life of an individual. Hence, an ideal form of treatment modality should be taken into consideration, consisting of regenerative approach in which diseased, necrotic pulp tissues are removed and replaced with healthy pulp tissue to revitalise the teeth [2].
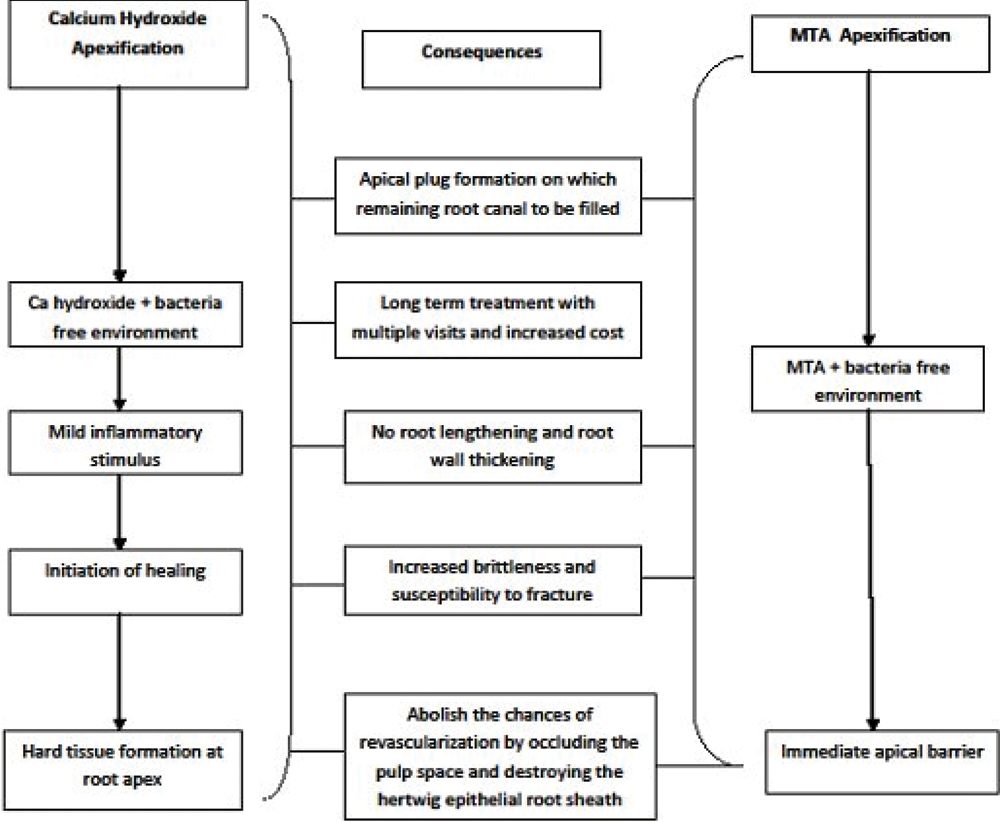
In the conventional calcium hydroxide apexification, an apical hard tissue barrier is formed wherein MTA apexification (comparatively newer method), an immediate apical barrier is formed [3,4]. In both circumstances, the pulpal regeneration is not evident suggesting the necessity of a novel procedure for pulpal revascularisation that promotes optimum healing of the tooth [Table/Fig-4].
The need of regeneration: Drawbacks of calcium hydroxide and MTA.
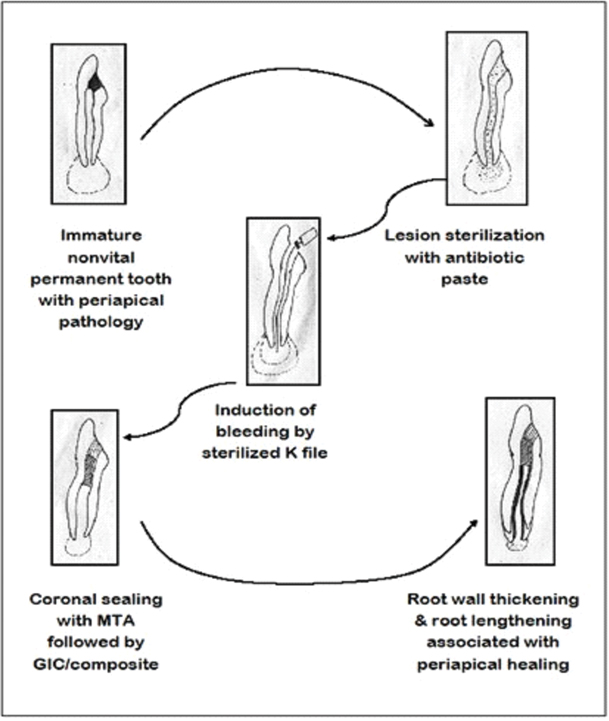
Pulp revascularisation has a unique concern because of lack of collateral blood supply. Henceforth, the periapical cells are of great importance for pulpal angiogenesis. The non-vital teeth with open apices are the best candidate for pulpal regeneration as they allow the periapical cell migration into the root canals in a sterilised condition. Minimum of 1.1mm opening at apex is crucial for periapical tissue to flow into the canals [3]. The basic rule of revascularisation in non-vital tooth is disinfection of root canals followed by induction of bleeding into root canal system via over instrumentation. The stem cells of remaining vital pulp or periapical region are the best source when using endodontic regeneration through blood clotting. The dental papilla of the root apex contains stem cells from apical papilla that may survive in infected condition and in association with Hertwig’s Epithelial root sheath, differentiate into odontoblasts, allowing root lengthening and root wall thickening. The induced blood clot may act as a scaffold and good source of growth factors (fibroblast growth factor, platelet derived growth factor, bone morphogenetic proteins and transforming growth factors and, colony stimulating factor, insulin like growth factor, nerve growth factor and interleukins) [4]. Scaffold, a three dimensional biodegradable porous polymer framework is needed for the growth of stem cells. It acts as a carrier on which stem cells are seeded and initiation of cell differentiation starts in presence of signaling molecules [5]. These two cases were performed with LSTR and revascularisation procedure [Table/Fig-5].
Clinical procedures: LSTR and revascularisation.
Current research directs the knowledge towards periapical stem cell stimulation and proliferation. Huang GT, suggested that dental stem cells may have the potential to regenerate bone, periodontal ligaments, possibly the whole tooth [6]. Shah N et al., introduced a technique named “Seal Bio” comprising of apical clearing, apical foramen widening and over-instrumentation into periapical region to induce bleeding near apical foramen [3]. Another recent approach called Apexum is introduced to enhance the healing kinetics of periapical lesions by minimally invasive removal of pathology through root canal access [7]. All the methods aim to achieve a larger apical opening to grow the healthy periapical tissue to the canals so that the vitality of the tooth is regained. The success of Regenerative Endodontic Procedure (REP) depends on the status of the pulp, maturity of the tooth, periodontal health, presence of systemic disease and lastly the immunity of the patient. Sterilisation of the root canal system is another important concern in REP. Antibiotic paste is preferred to sterilise the root canals prior to any revascularisation procedure. Hosino E et al., introduced a three mix antibiotic paste system that was re-evaluated by Takushige T et al., [1,8]. Root canals are commonly infected by both aerobic and anaerobic organisms; therefore, single antibiotic has not proved to be effective for the complete sterilisation. Mehdi HE and Hakima C demonstrated sterilisation of root canals with mixture of tri antibiotic paste in LSTR procedure of primary molars successfully [9].
The first case was ideal for LSTR and revascularisation as it fulfills the minimum requirements for the success i.e., young immature non-vital tooth with wide apical opening and blander bass canal. In the second case, an attempt was made in a periodontally compromised non-vital tooth about to mature, resulting in reappearance of periapical pathology with no clinical symptoms. Therefore, it can be proved that the maturity of the tooth and periodontal health are crucial factors for the success in REP.
Conclusion
Therefore, mentioned cases signify the importance of regenerative endodontic procedures in reestablishment of the vitality of teeth which can be considered the treatment of choice in regular day-to-day practice. LSTR and revascularisation procedure has been proved to be effective in young immature permanent teeth without any periodontal source of infection.
[1]. Hoshino E, Kurihara-Ando N, Sato I, Uematsu H, Sato M, Kota K, In vitro antibacterial susceptibility of bacteria from infected root dentin to a mixture of ciprofloxacin, metronidazole and minocyclineInt Endod J 1996 29:125-30.10.1111/j.1365-2591.1996.tb01173.x9206436 [Google Scholar] [CrossRef] [PubMed]
[2]. Nakashima M, Akamine A, The application of tissue engineering to regeneration of pulp and dentin in endodonticsJ Endod 2005 31(10):711-18.10.1097/01.don.0000164138.49923.e516186748 [Google Scholar] [CrossRef] [PubMed]
[3]. Shah N, Logani A, Bhaskar U, Aggarwal V, Efficacy of revascularization to induce apexification/apexogenesis in infected, nonvital, immature teeth: a pilot clinical studyJ Endod 2008 34(8):919-25.10.1016/j.joen.2008.05.00118634921 [Google Scholar] [CrossRef] [PubMed]
[4]. Sharma S, Sikri V, Sharma NK, Sharma VM, Regeneration of tooth pulp and dentin: trends and advancesAnnals of Neurosciences 2010 17(1):31-43.10.5214/ans.0972.7531.2010.170109 [Google Scholar] [CrossRef]
[5]. Banches F, Trope M, Revascularization of an immature permanent tooth with apical periodontitis: new treatment protocol?J Endod 2004 30(4):196-200.10.1097/00004770-200404000-0000315085044 [Google Scholar] [CrossRef] [PubMed]
[6]. Huang GT, A paradigm shift in endodontic management of immature teeth: conservation of stem cells for regenerationJ Dent 2008 36(6):379-86.10.1016/j.jdent.2008.03.00218420332 [Google Scholar] [CrossRef] [PubMed]
[7]. Metzger Z, Huber R, Tabis I, Better H, Enhancement of healing kinetics of periapical lesions in dogs by the Apexum procedureJ Endod 2009 35(1):40-45.10.1016/j.joen.2008.10.00219084122 [Google Scholar] [CrossRef] [PubMed]
[8]. Takushige T, Cruz EV, Moral AA, Hoshino E, Endodontic treatment of primary teeth using a combination of antibacterial drugsInt Endod J 2004 37(2):132-38.10.1111/j.0143-2885.2004.00771.x14871180 [Google Scholar] [CrossRef] [PubMed]
[9]. Mehdi HE, Hakima C, Lesion sterilization and tissue repair therapy (LSTR) of necrotic primary molars: case reportInternational Journal of Research Studies in Medical and Health Sciences 2017 2(4):01-04.10.22259/ijrsmhs.0204001 [Google Scholar] [CrossRef]