Labial Agglutination in a Pubertal Girl
Pushpawati1, Vinita Singh2, Snehil Sinha3, Amrita Singh4
1 Associate Professor, Department of Obstetrics and Gynaecology, AIIMS Raipur, Raipur, Chhatisgarh, India.
2 Associate Professor, Department of Obstetrics and Gynaecology, AIIMS Raipur, Raipur, Chhatisgarh, India.
3 Senior Resident, Department of Obstetrics and Gynaecology, AIIMS Raipur, Raipur, Chhatisgarh, India.
4 Senior Resident, Department of Obstetrics and Gynaecology, AIIMS Raipur, Raipur, Chhatisgarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vinita Singh, Associate Professor, Department of Obstetrics and Gynaecology, AIIMS Raipur, Raipur-492001, Chhatisgarh, India.
E-mail: ddvinitasingh@gmail.com
Labial agglutination is a state of partial or complete adhesion of the labia minora. It occurs in prepubertal or postmenopausal women and usually associated with low estrogen levels. Labial agglutination is rare in women of reproductive age group due to abundance of estrogen. We are presenting a neglected case of labial agglutination in pubertal girl of 16 years age due to its rare presentation and different approach for treatment in this age group who was suffering since birth. After taking detailed history, thorough clinical examination and all required laboratory and imaging investigations we could reach to the correct diagnosis which was followed by skilful surgery. This approach cured her distorted vestibular anatomy without any complication. Patient was treated by surgery i.e. labial adhesinolysis under vaginoscopic guided approach using our standard hysteroscope light and camera. Labial adhesion can be treated both medically and surgically however treatment is individualised in every case ranging from medical treatment to minimally invasive surgery or invasive skilful surgery.
Labial adhesiolysis, Labial adhesion, Labial fusion
Case Report
A 16-year old, non sexually active girl was presented with the chief complaint of post micturition dribbling of urine and dysmenorrhoea since one year. Her mother noticed that the vaginal opening was not visible and she passed urine through small opening. She had a history of regular menstrual cycles since menarche. She attained her menarche at an age 12. Her medical history was that she had pulmonary tuberculosis four years back and she took complete course of Antitubercular treatment. She also had history of urinary tract infection for which she took treatment and had recovered. In her family history her mother was known case of diabetes mellitus and hypertension. She had no history of any genital trauma or sexual assault.
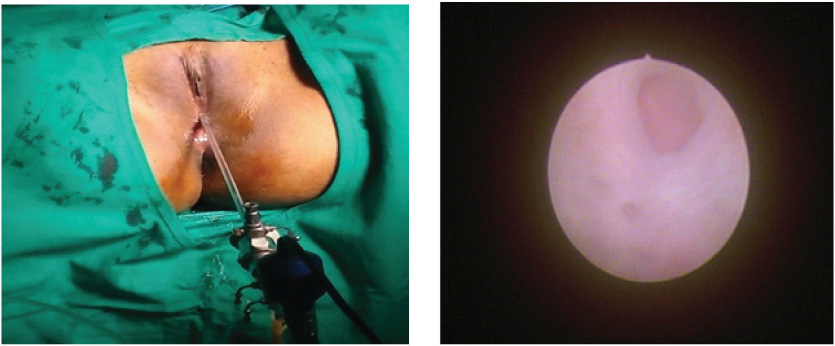
On examination she had B4 stage of breast development P4 satge of pubic hair development and A3 stage of axillary hair development. On local examination she had well developed labia majora. There seemed to be no dermatological disorder of vulva and no signs of local infection. Labia minora was fused together in the midline, dense adhesion was present from the clitoris to the posterior vestibule. There was complete fusion of labia minora with obliteration of the vaginal introitus and urethral meatus with a pin hole opening for urine and menstrual blood flow and anal opening was in normal position [Table/Fig-1]. Urine routine, microscopic and culture were negative for infection. Pelvic transabdominal ultrasonography showed normal size and shape of uterus and ovaries as well as normal urinary tract. clinical diagnosis of labial agglutination was made.
Preoperative view (Pre procedure appearance of labial adhesion) complete fusion of labia minora with obliteration of the vaginal introitus and pinhole external urethral meatus.

Surgery was planned under general anaesthesia. After proper preoperative preparation and after obtaining anaesthesia and medical clearance patient was taken up in operation theatre with guardian consent. Labial adhesinolysis under vaginoscopic guided approach using our standard hysteroscope light and camera was done [Table/Fig-2]. We approached through the only pin point opening using fine scissors cutting the adhesion bands from a dense adhesion present from the clitoris to the posterior vestibule [Table/Fig-3]. After surgery vagina, vaginal and urethral opening were found absolutely normal anatomically and physiologically. Vaginal bleeding was minimal and patient stood the procedure well.
Intraoperative view (vaginoscopic view) of Labial adhesion.
Early postoperative view of the case after labial adhesinolysis. Normal vestibular anatomy restored. Normal introitus, vaginal length and urethral opening.
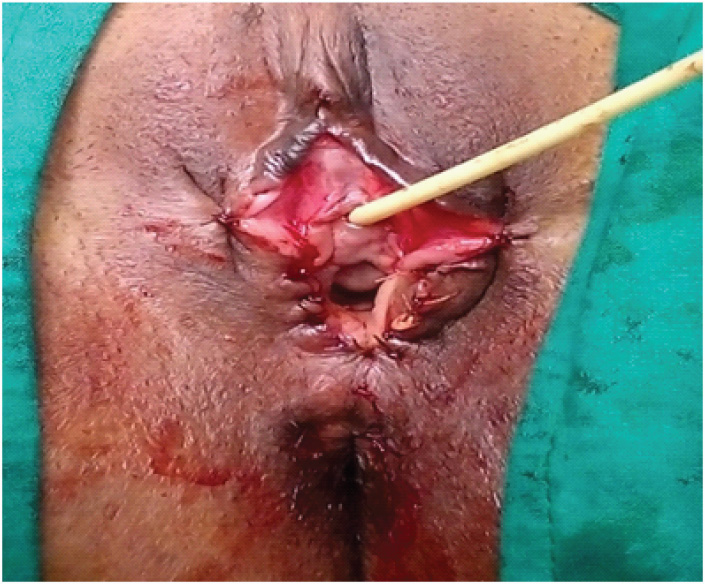
Post-operative period was uneventful. Patient was asked to apply estrogen cream locally for four weeks. Patient was followed after a week, month and one year. On follow up she had normal labia majora and minora, introitus and urethral opening with no urinary difficulty and no recurrence of labial adhesion.
Discussion
Labial fusion is a state of partial or complete adhesion of the labia minora generally occuring in young girls or post-menopausal women, but is extremely rare in females after attaining puberty [1]. The relative hypoestrogenic environment is suggested as the main predisposing factor of this condition in prepubertal girls [2]. The condition usually resolves once they attain puberty so aggressive treatment is not recommended unless patient is symptomatic of any urinary problem. In adults including postmenopausal women, labial fusion is more associated with recurrent urinary tract infections, vulvovaginal infections, poor personal hygiene, genital trauma, hypoestrogenism, underlying dermatological disease, lack of sexual activity [3-5]. In the present case low estrogen status was excluded to be the cause of her labial agglutination because patient had history of regular menses, normal ovaries in ultrasound and fully developed secondary sexual character. She had no history of genital trauma or sexual abuse. Labial adhesion is rare in female of reproductive age group due to abundance of estrogen. In literature search only few cases of labial fusion has been reported in reproductive age women [6-8]. Medical and surgical management were described in various literature for treatment of labial adhesion. Topical estrogen application is considered as first line treatment for labial adhesions for superficial labial adhesions in prepubertal girls and postmenopausal women [9]. In addition, manual separation of adhesions with care and maintenance of local hygiene have also been reported to resolve paediatric labial adhesions [10]. Surgical adhesiolysis is the treatment of choice and local estrogen might not prove to be that beneficial [2,8]. In our case we opted for vaginoscopic approach followed by adhesiolysis due to thick adhesion.
Conclusion
Labial fusion is a relatively common condition in prepubertal girl but rare in women of reproductive age group. Both medical and surgical treatment is effective but reoccurrence is common in both the variety of treatment. In literature search no large studies were found for management of labial adhesions. So most of the treatment were based on the own experience of operating surgeon. However, it is better to rule out all the underlying causes and then proceed to surgical separation under anaesthesia with proper postoperative care for better results.
[1]. Tsujita Y, Asakuma J, Kanbara T, Yoshii T, Azuma R, Sumitomo M, A case of labial adhesion in a reproductive womanHinyokika Kiyo 2010 56(8):463-65. [Google Scholar]
[2]. Mayoglou L, Dulabon L, Martin-Alguacil N, Pfaff D, Schober J, Success of treatment modalities for labial fusion: A retrospective evaluation of topical and surgical treatmentsJournal of Pediatric and Adolescent Gynecology 2009 22(4):247-50.10.1016/j.jpag.2008.09.00319646671 [Google Scholar] [CrossRef] [PubMed]
[3]. Lambert B, Complete adult vulvar fusion: A case reportJournal of Obstetrics and Gynaecology Canada 2004 26(5):501-02.10.1016/S1701-2163(16)30661-2 [Google Scholar] [CrossRef]
[4]. Awang NA, Viegas C, Viegas OA, Incomplete bladder emptying due to labial fusion in a pubertal girl: A delayed consequence of female circumcisionAust N Z J Obstet Gynaecol 2004 44(4):372-73.10.1111/j.1479-828X.2004.00261.x15282020 [Google Scholar] [CrossRef] [PubMed]
[5]. Norbeck JC, Ritchey MR, Bloom DA, Labial fusion causing upper urinary tract obstructionUrology 1993 42(2):209-11.10.1016/0090-4295(93)90650-Y [Google Scholar] [CrossRef]
[6]. Kumar RK, Sonika A, Charu C, Sunesh K, Neena M, Labial adhesions in pubertal girlsArch Gynecol Obstet 2006 273(4):243-45.10.1007/s00404-005-0060-816189695 [Google Scholar] [CrossRef] [PubMed]
[7]. Ozekinci M, Yucel S, Sanhal C, Akar ME, Labial fusion causing coital and voiding difficulty in a young womanAdvances in Sexual Medicine 2013 3(1):11-13.10.4236/asm.2013.31002 [Google Scholar] [CrossRef]
[8]. Erdo du E, Demirel C, Tahao lu AE, Özdemir A, Labial fusion: A rare cause of urinary retention in reproductive age woman and review of literatureTurk J Urol 2017 43(1):98-101.10.5152/tud.2017.5889728270959 [Google Scholar] [CrossRef] [PubMed]
[9]. Dirim A, Hasirci E, Labial fusion causing urinary incontinence and recurrent urinary tract infection in a postmenopausal female: A case reportInt Urogynecol J 2011 22(1):119-20.10.1007/s00192-010-1205-220571766 [Google Scholar] [CrossRef] [PubMed]
[10]. Watanabe T, Matsubara S, Fujinaga Y, Asada K, Ohmaru T, Suzuki M, Manual separation followed by local cleanliness for paediatric labial adhesionJ Obstet Gynaecol Res 2010 36(3):667-70.10.1111/j.1447-0756.2010.01192.x20598054 [Google Scholar] [CrossRef] [PubMed]