Reversible Sinusoidal Obstruction Syndrome with Nodular Regenerative Hyperplasia Following Oxaliplatin-Based Chemotherapy
Khalil Aloreidi1, Maheedar Gedela2, Dheera Keerthi Kattula3, David Bean4, Lokesh Jha5
1 Resident, Department of Internal Medicine, University of South Dakota - Sanford School of Medicine, Sioux Falls, South Dakota, USA.
2 Resident, Department of Internal Medicine, University of South Dakota - Sanford School of Medicine, Sioux Falls, South Dakota, USA.
3 Student, Rangaraya Medical College, Kakinada, Andhra Pradesh, India.
4 Radiologist, Department of Radiology, Sanford Radiology Clinic, Sioux Falls, South Dakota, USA.
5 Hepatologist, Department of Hepatology, Sanford Radiology Clinic, Sioux Falls, South Dakota, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Khalil Aloreid, 1400 W, 22nd Street, Sioux Falls, South Dakota, USA.
E-mail: khalil.aloreidi@usd.edu
Sinusoidal Obstruction Syndrome (SOS) is a form of hepatic injury characterized by damage to small hepatic vessels resulting in occlusion of the terminal hepatic venules and hepatic sinusoids. Oxaliplatin has been associated with distinct side effects; one of them reported recently which is SOS. We report a patient with history of colon cancer who presented with elevated liver enzymes and liver nodules. After extensive evaluation, the patient found to have a severe form of SOS which is the Nodular Regenerative Hyperplasia (NRH) as a result of oxaliplatin based chemotherapy. We also report the reversibility of this condition after treatment cessation which is something that is not always feasible. The diagnosis of this case was challenging as the liver nodules thought to be metastases initially and that is why we believe recognizing this entity is crucial to prevent misdiagnosis and consequent unnecessary surgical intervention.
Colon cancer, Oxaliplatin, Drug-induced liver injury
Case Report
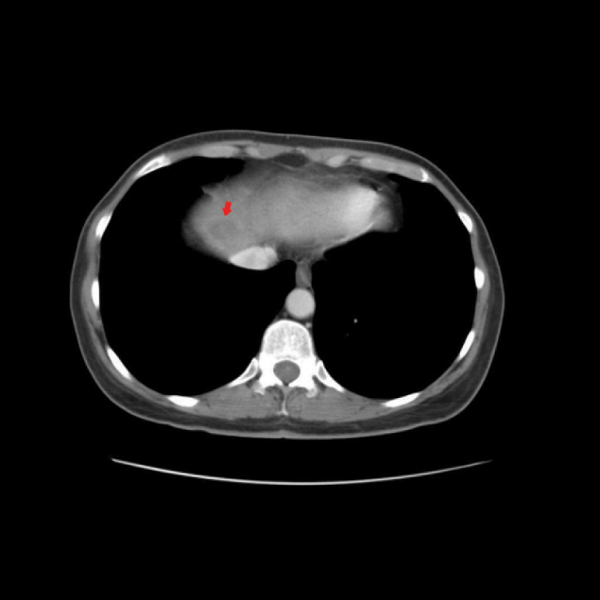
A 61-year-old female with a history of stage IIIB (pT3, pN1b, cM0) adenocarcinoma of the colon after post-laparoscopic-assisted resection of the sigmoid and left colon. She was started on adjuvant chemotherapy with oxaliplatin and capecitabine. Two months later, she was found to have elevated liver enzymes. Her Alanine Aminotransferase (ALT) was 71 U/L, Aspartate Aminotransferase (AST) was 80 U/L, and Alkaline Phosphatase (ALP) was 134 U/L. Her vital signs were normal and on her physical examination there were no signs of liver disease. Computed Tomography (CT) of the abdomen showed multiple linear nodular hypo densities within the liver, most noticeable on the delayed images along with hypodensity within the dome of the liver, suggesting metastasis [Table/Fig-1]. These findings were not present in the CT scan done prior to chemotherapy initiation. Because the lesions were seen only on the delayed images of CT abdomen, the liver biopsy was done which showed mild steatosis with no significant fibrosis as the nodular lesions were probably missed in non-contrast CT guided biopsy.
CT scan showing hypodensity within the dome of the liver (Red Arrow).
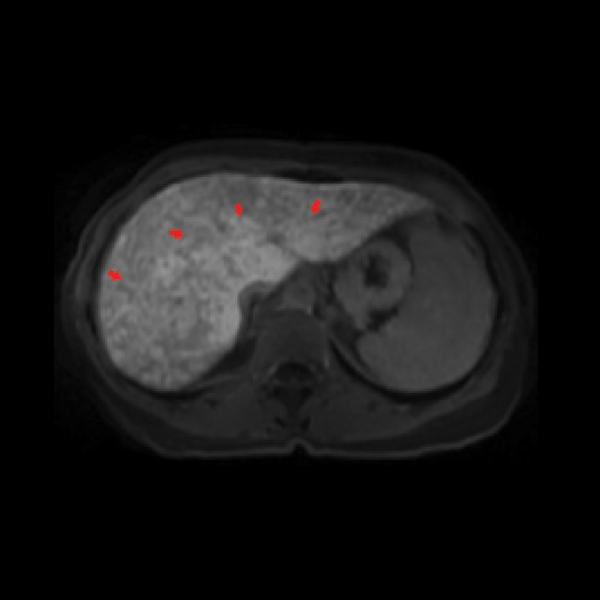
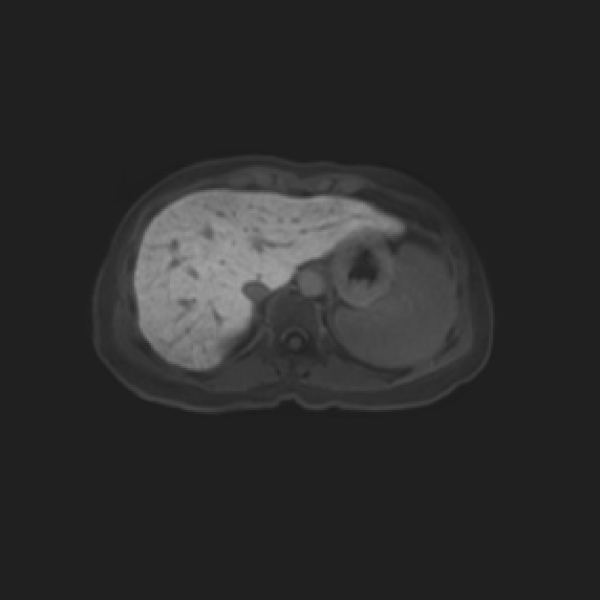
The patient then underwent Magnetic Resonance Imaging (MRI) of the abdomen [Table/Fig-2] with Gadoxetate disodium (Eovist®) which showed a linear, nodular, patchy low signal throughout the liver consistent with sinusoidal obstruction syndrome and nodular regenerative hyperplasia concerning for oxaliplatin toxicity and so it was stopped. Three months later, a follow-up MRI of the abdomen [Table/Fig-3] showed significant improvement in the previously noted diffuse liver disease with improvement in liver enzymes [Table/Fig-4].
Liver MRI showing the linear, nodular low signal throughout the liver (Red Arrows), consistent with sinusoidal obstruction syndrome due to Oxaliplatin therapy.
Liver MRI showing significant improvement in the previously noted diffuse liver disease.
Demonstrates the patient’s liver enzymes trend over the period from starting of the Oxaliplatin therapy until 6 months after it was stopped.
| Initial Values | Oxaliplatin Stopped | After 2 months | After 6 Months |
|---|
| ALP(38-126 U/L) | 134 | 119 | 129 | 126 |
| ALT(11-66 U/L) | 71 | 26 | 25 | 46 |
| AST(14-59 U/L) | 80 | 42 | 34 | 55 |
Discussion
Oxaliplatin-based chemotherapy is most commonly used in the setting of colorectal cancer and its associated metastatic disease [1]. In patients with colorectal hepatic metastasis, oxaliplatin increases the surgical amenability of the formerly unresectable lesions, subsequently increasing the disease-free survival and overall survival rates [2]. However, liver injury, including SOS, has been observed after chemotherapy that utilizes oxaliplatin with the incidence rate of sinusoidal changes reaching up to 75% [3]. SOS has also been described in association with other drugs such as azathioprine, 6-mercaptopurine, 6-thioguanine, busulfan, cyclophosphamide, doxorubicin, etoposide, etc., [4].
Since the first clinical study describing this entity in 2004 [5], oxaliplatin-induced hepatic injury has become a major concern because its pattern mimics metastatic liver lesions in imaging, leading to misdiagnosis and overtreatment. Indeed, there are three reported cases of focal SOS similar to our case and have been treated by surgical resection [6-8]. The exact mechanism of liver injury due to oxaliplatin is not fully understood. However, oxaliplatin is more toxic to sinusoidal endothelial cells than hepatocytes. Other forms of oxaliplatin-related liver damage are centrilobular, perisinusoidal, and venular fibrosis; peliosis; and NRH [9]. NRH is characterized by the diffuse transformation of normal hepatic parenchyma into small, regenerative nodules and represents the most significant degree of injury in SOS. While the pathogenesis of NRH is not clear, it has been suggested that it represents a chronic ischemic injury secondary to disturbance to the blood flow within the liver, which consequently results in portal hypertension [10].
SOS, previously termed veno-occlusive disease, or blue liver syndrome is a distinctive and potentially fatal form of hepatic injury that occurs predominantly after drug exposure. The characteristic histological features of SOS are sinusoidal congestion and dilatation; disruption of the sinusoidal membrane and collagen deposition within the perisinusoidal space, leading to a bluish appearance of the liver [5]. Clinically, oxaliplatin-induced SOS symptoms are nonspecific. Elevated transaminase levels, jaundice, hepatomegaly, splenomegaly with subsequent thrombocytopenia and ascites could occur. Moreover, it may be associated with an increased perioperative morbidity and bleeding risk as well as delayed liver regeneration after liver resection [11]. A diagnosis of SOS can often be made based on clinical presentation and imaging studies. A liver biopsy is diagnostic but not always practical due to chemotherapy-induced thrombocytopenia and neutropenia. Gadolinium-Ethoxybenzyl magnetic resonance imaging (Gd-EOB MRI), which is the most reliable modality in colorectal liver metastasis, shows a defect in the hepatocyte phase in SOS similar to imaging findings of colorectal liver metastasis. Therefore, a qualitative imaging modality such as diffusion-weighted MRI may be superior because the cellular density is higher in cancer than in SOS [12]. Also, the reticular hypointensity in hepatobiliary phase images of Gd-EOB MRI is highly specific for SOS and it can be divided into five levels with levels four and five considered indicating SOS [13]. Additionally, SOS does not show uptake in a Positron Emission Tomography (PET) scan, whereas 90-94% of liver metastases are detected with PET/CT scans [14].
Management of SOS is aimed to avoid further injury caused by oxaliplatin; preventing unnecessary complications such as hypotension, electrolyte and acid-base imbalance, renal and pulmonary failure, infectious complications and maintaining intravascular volume and renal perfusion while limiting third-space fluid accumulation. Glutamine (or glutathione) has been investigated as a potential therapy for oxaliplatin-induced liver injury [15]. Further, the incidence and severity of sinusoidal changes have been shown to be reduced with co-administration of Bevacizumab [16].
Regarding the reversibility of SOS, our case demonstrated a good response after cessation of the oxaliplatin therapy with disappearance of MRI liver changes and normalization of liver enzyme level. However, this is not always the case as the persistence and even the progression of SOS and NRH have been observed in the short and long term [17]. It is certain that the risk of progressive disease is undeniable, especially in patients exposed to higher numbers of chemotherapy cycles.
Conclusion
Oxaliplatin-induced liver injury should be considered in patients presenting with liver nodules who were previously treated with chemotherapy regimen containing oxaliplatin. We recommend that the appropriate imaging should be performed in order to differentiate this entity from metastasis so that unnecessary surgical intervention and overtreatment can be minimized.
[1]. Seo AN, Kim H, Sinusoidal obstruction syndrome after oxaliplatin-based chemotherapyClin Mol Hepatol 2014 20(1):81-84.10.3350/cmh.2014.20.1.8124757663 [Google Scholar] [CrossRef] [PubMed]
[2]. Morris-Stiff G, White AD, Gomez D, Cameron IC, Farid S, Toogood GJ, Nodular regenerative hyperplasia (NRH) complicating oxaliplatin chemotherapy in patients undergoing resection of colorectal liver metastasesEur J Surg Oncol 2014 40(8):1016-20.10.1016/j.ejso.2013.09.01524370284 [Google Scholar] [CrossRef] [PubMed]
[3]. Nguyen-Khac E, Lobry C, Chatelain D, Fuks D, Joly JP, Brevet M, A reappraisal of chemotherapy-induced liver injury in colorectal liver metastases before the era of antiangiogenicsInt J Hepatol 2013 2013:31486810.1155/2013/31486823533786 [Google Scholar] [CrossRef] [PubMed]
[4]. LIVERTOX. Sinusoidal Obstruction Syndrome (Veno-occlusive Disease) [updated June 2, 2017. Available from: https://livertox.nlm.nih.gov/Phenotypes_sinus.html [Google Scholar]
[5]. Rubbia-Brandt L, Audard V, Sartoretti P, Roth AD, Brezault C, Le Charpentier M, Severe hepatic sinusoidal obstruction associated with oxaliplatin-based chemotherapy in patients with metastatic colorectal cancerAnn Oncol 2004 15(3):460-66.10.1093/annonc/mdh09514998849 [Google Scholar] [CrossRef] [PubMed]
[6]. Alexandrino H, Oliveira D, Cipriano MA, Ferreira L, Tralhão JG, Castro E, Sousa F, Oxaliplatin toxicity presenting as a liver nodule - Case reportBMC Cancer 2015 15:24710.1186/s12885-015-1247-425886004 [Google Scholar] [CrossRef] [PubMed]
[7]. Arakawa Y, Shimada M, Utsunomya T, Imura S, Morine Y, Ikemoto T, Oxaliplatin-related sinusoidal obstruction syndrome mimicking metastatic liver tumorsHepatol Res 2013 43(6):685-89.10.1111/j.1872-034X.2012.01114.x23730707 [Google Scholar] [CrossRef] [PubMed]
[8]. Uchino K, Fujisawa M, Watanabe T, Endo Y, Nobuhisa T, Matsumoto Y, Oxaliplatin-induced liver injury mimicking metastatic tumor on images: a case reportJpn J Clin Oncol 2013 43(10):1034-38.10.1093/jjco/hyt11323958518 [Google Scholar] [CrossRef] [PubMed]
[9]. Rubbia-Brandt L, Lauwers GY, Wang H, Majno PE, Tanabe K, Zhu AX, Sinusoidal obstruction syndrome and nodular regenerative hyperplasia are frequent oxaliplatin-associated liver lesions and partially prevented by bevacizumab in patients with hepatic colorectal metastasisHistopathology 2010 56(4):430-39.10.1111/j.1365-2559.2010.03511.x20459550 [Google Scholar] [CrossRef] [PubMed]
[10]. Shimamatsu K, Wanless IR, Role of ischemia in causing apoptosis, atrophy, and nodular hyperplasia in human liverHepatology 1997 26(2):343-50.10.1002/hep.5102602149252144 [Google Scholar] [CrossRef] [PubMed]
[11]. Aloia T, Sebagh M, Plasse M, Karam V, Lévi F, Giacchetti S, Liver histology and surgical outcomes after preoperative chemotherapy with fluorouracil plus oxaliplatin in colorectal cancer liver metastasesJ Clin Oncol 2006 24(31):4983-90.10.1200/JCO.2006.05.815617075116 [Google Scholar] [CrossRef] [PubMed]
[12]. Namimoto T, Yamashita Y, Sumi S, Tang Y, Takahashi M, Focal liver masses: characterization with diffusion-weighted echo-planar MR imagingRadiology 1997 204(3):739-44.10.1148/radiology.204.3.92802529280252 [Google Scholar] [CrossRef] [PubMed]
[13]. Shin NY, Kim MJ, Lim JS, Park MS, Chung YE, Choi JY, Accuracy of gadoxetic acid-enhanced magnetic resonance imaging for the diagnosis of sinusoidal obstruction syndrome in patients with chemotherapy-treated colorectal liver metastasesEuropean Radiology 2012 22(4):864-71.10.1007/s00330-011-2333-x22108766 [Google Scholar] [CrossRef] [PubMed]
[14]. Sacks A, Peller PJ, Surasi DS, Chatburn L, Mercier G, Subramaniam RM, Value of PET/CT in the management of liver metastases, part 1AJR Am J Roentgenol 2011 197(2):W256-59.10.2214/AJR.10.633121785050 [Google Scholar] [CrossRef] [PubMed]
[15]. Kang GH, Moon HS, Lee ES, Kim SH, Sung JK, Lee BS, A case of liver fibrosis with splenomegaly after oxaliplatin-based adjuvant chemotherapy for colon cancerJ Korean Med Sci 2013 28(12):1835-38.10.3346/jkms.2013.28.12.183524339718 [Google Scholar] [CrossRef] [PubMed]
[16]. Hubert C, Sempoux C, Humblet Y, Van den Eynde M, Zech F, Leclercq I, Sinusoidal obstruction syndrome (SOS) related to chemotherapy for colorectal liver metastases: factors predictive of severe SOS lesions and protective effect of bevacizumabHPB(oxford) 2013 15(11):858-64.10.1111/hpb.1204723458554 [Google Scholar] [CrossRef] [PubMed]
[17]. Mentha G, Terraz S, Morel P, Andres A, Giostra E, Roth A, Dangerous halo after neoadjuvant chemotherapy and two-step hepatectomy for colorectal liver metastasesBr J Surg 2009 96(1):95-103.10.1002/bjs.643619109800 [Google Scholar] [CrossRef] [PubMed]