Removal of a Deeply Impacted Ectopic Mandibular Third Molar through a Buccal Corticotomy in Severe Trismus-A Case Report
Ranjeet Bodh1, Saroj Kumari2, Sujata Mohanty3, Rudra Deo Kumar4, Catherine Diana5
1 Senior Resident, Department of Oral and Maxillofacial Surgery, Maulana Azad Institute of Dental Sciences, New Delhi, Delhi, India.
2 Senior Resident, Department of Oral and Maxillofacial Surgery, Maulana Azad Institute of Dental Sciences, New Delhi, Delhi, India.
3 Professor and Head, Department of Oral and Maxillofacial Surgery, Maulana Azad Institute of Dental Sciences, New Delhi, Delhi, India.
4 Postgraduate Student, Department of Oral and Maxillofacial Surgery, Maulana Azad Institute of Dental Sciences, New Delhi, Delhi, India.
5 Postgraduate Student, Department of Oral and Maxillofacial Surgery, Maulana Azad Institute of Dental Sciences, New Delhi, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ranjeet Bodh, Senior Resident, Department of Oral and Maxillofacial Surgery, Maulana Azad Institute of Dental Sciences, New Delhi-110002, Delhi, India.
E-mail: rbjohnmayer85@gmail.com
Management of deeply impacted mandibular third molar in itself is a surgical challenge and when it is associated with restricted mouth opening, it becomes more devious job. Deeply impacted tooth can be approached by buccal corticotomy/osteotomy, lingual split, extraoral approach or sagittal split ramus osteotomy. In patients with restricted mouth opening, options get limited to buccal corticotomy and extraoral approach. Extraoral approach is not a preferred option pertaining to scar formation and potential risk of injury to the marginal mandibular branch of the facial nerve leaving buccal corticotomy as most viable option.
Disimpaction, Impacted tooth, Lingual split
Case Report
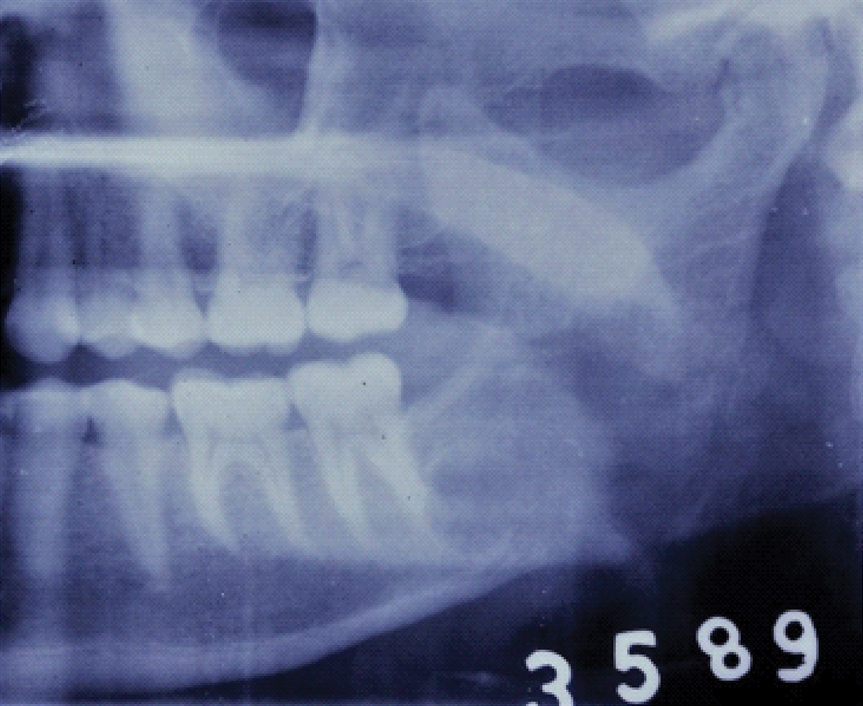
A 25-year-old female patient reported to Department of Oral and Maxillofacial Surgery, Maulana Azad Institute of Dental Sciences, New Delhi, India, with chief complaint of difficulty in mouth opening which was associated with pain, with respect to the left lower back tooth region from past one month. She was a known case of osteomyelitis of skull base admitted under neurosurgery department for management of the same. Patient was already under Intravenous (IV) Levofloxacin from two months for osteomyelitis management. Extra oral examination revealed, grossly symmetrical face, severe trismus with reduced mouth opening and tenderness in the left angle region of mandible. On intra oral examination there was tenderness, erythematous mucogingival tissue in left lower buccal vestibule. Orthopantomogram revealed impacted (Horizontal, Winter’s classification) 38 with dilacerated root and crown abutting the inferior alveolar canal and root apex of 37 [Table/Fig-1,2] [1,2].
Preoperative photograph showing severe trismus.

Preoperative orthopantomogram showing impacted mandibular third molar abutting inferior alveolar canal and root apex of 37.

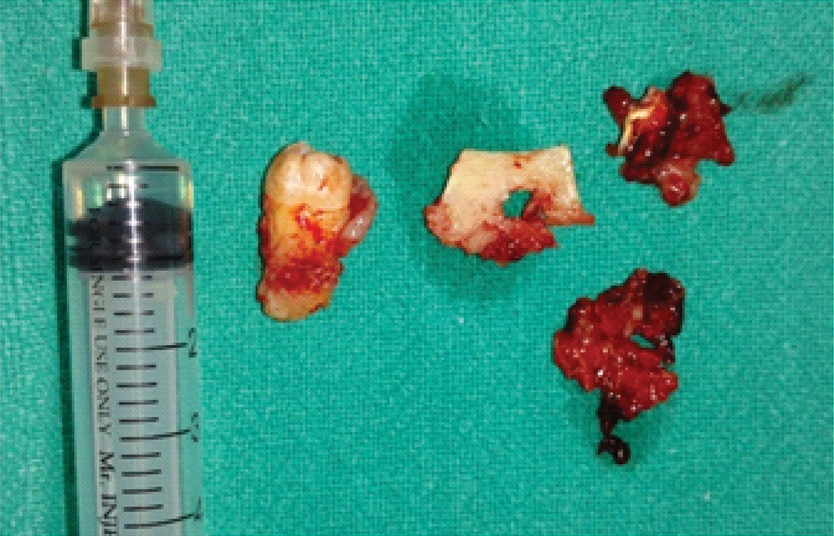
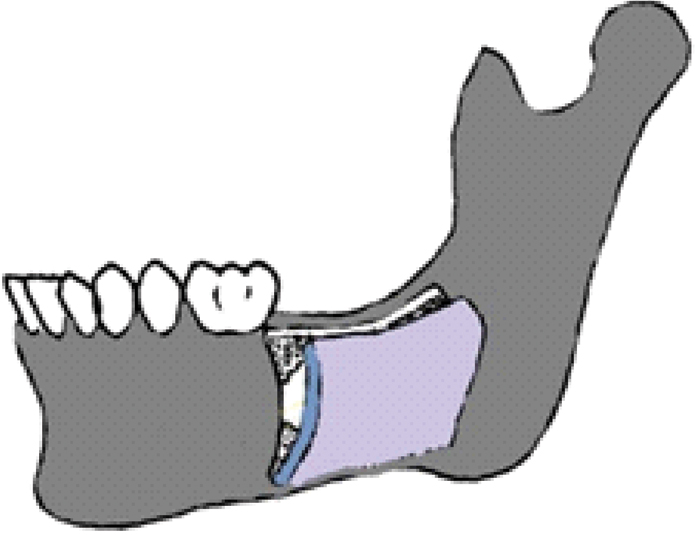
In view of worsening trismus which was unresponsive to above mentioned antibiotics (IV levofloxacin 750 mg), surgical removal of 38 was planned. Haematological investigations (CBC, BT, CT, RBS, Tridot, Serum electrolyte, LFT, KFT) revealed hyponatraemia and low haemoglobin (8.5 gm/dL) making patient unfit for general anaesthesia. Thus, plan of disimpaction via buccal corticotomy approach intraorally was made as conventional intraoral approaches need adequate mouth opening. Neurosurgical clearance and patient’s consent were taken prior to surgery. Phenytoin (500 mg) was given prior to surgery as per neurosurgeon’s advice. The third molar was approached with vestibular incision and mucoperiosteal flap was raised. A rectangular window was made over the impacted tooth using a narrow fissure bur, with the horizontal cut on external oblique ridge and mesial and distal cuts almost reaching the apex of second molar. Corticotomy was completed using a chisel and buccal cortical plate was removed to prevent the possibility of compression and irritation of already inflamed neurovascular bundle. The impacted tooth was removed uneventfully through the created window. Inferior alveolar neurovascular bundle was preserved which could be appreciated on the floor of the created defect [Table/Fig-3,4,5 and 6]. Surgical procedure was completed in 20 minutes. No intraoperative complications were noted. The healing was uneventful postoperatively with significant improvement in mouth opening (20 mm) [Table/Fig-7,8]. Mouth opening of 31 mm was noted on one month follow up. Postoperative paresthesia was reported which completely resolved in one month period.
Surgical access for impacted tooth made through buccal corticotomy.

Neurovascular bundle visible after removal of tooth.

Disimpacted tooth and removed buccal cortical plate.
Buccal corticotomy approach.
Postoperative photograph showing improved mouth opening.

Postoperative orthopantomogram after removal of impacted tooth.
Discussion
The word trismus, which derives from the Greek word “trismos” means grating or grinding of the teeth [3]. In Gould’s medical dictionary, trismus is defined and classified aetiologically as follows: “Spasm of the muscles of mastication, the condition commonly called lock jaw, a titanic condition of the muscles of mastication; or trauma caused by external violence [4].” Limited opening of the jaw is usually due to extra-articular disease with masticatory muscle spasm secondary to stress, trauma (injury to medial pterygoid with needle) or local infection (e.g., pericoronitis around a partially erupted mandibular third molar). Occasionally, it can also be sequelae of intracapsular or pericapsular pathology [3-5]. Trismus secondary to impacted third molar is a very common finding where the main cause is pericoronitis. Here we represent a case of severe trismus with reduced mouth opening due to horizontally impacted third molar abutting the inferior alveolar canal and its surgical management.
Trismus is thought to be a protective reflex that minimises jaw movement to prevent further trauma to already injured tissues [3,6]. Impulses are sent to the trigeminal ganglion when undifferentiated, non-encapsulated nerve endings for pain and temperature sensation are stimulated. The information is related either directly to the motor nucleus of V (reflex arc) or first to the reticular formation or the sensory nucleus of V and then to the motor nucleus of V. Activation of efferent motor neurons from this nucleus resulted in muscle contraction [3,7]. The removal of the stimuli should begin early in the progression of the trismus as it is more effective and easier for the patient. If treatment is delayed, the difficulty in reversing the trismus increases [3-5].
Trismus in partially impacted third molar is the usual cause in pericoronitis, due to spasm of masticatory muscle which resolves with medication, operculectomy or surgical removal [6]. In general, partially or completely unerupted teeth are removed via conventional intraoral approach. On the other hand, deeply impacted or ectopic third molars need either extraoral approach or sagittal split ramus osteotomy [7-10]. In patients with trismus, surgical options get limited to extraoral approach which necessitate general anaesthesia.
Stimulus for severe trismus in this case was the impacted third molar which was progressively compressing the neurovascular bundle. In our particular case, patient was already on broad spectrum antibiotics since two months in view of osteomyelitis excluding medicinal management as a treatment choice. Trismus was refractory to medication which lead to poor nutritional status so the removal of tooth was necessary. Hence, the tooth was approached via buccal corticotomy as conventional intraoral approaches was not possible as they need adequate mouth opening [11]. Extraoral approach was denied as patient was not fit for general anaesthesia due to electrolyte imbalance and low haemoglobin (8.5 gm/dL).
Buccal corticotomy is a well-known technique for surgical exposure of the inferior alveolar nerve in micro-neurosurgical procedures. It provides wide exposure of neurovascular bundle and associated structures [12]. Hence, buccal corticotomy was planned for the present case.
Conclusion
Severe trismus due to inferior alveolar nerve compression is rare but can be possible sequelae in impacted third molar and it should be treated early. Buccal corticotomy approach provides wide exposure with good visibility, which allows easy removal of deeply impacted third molar. It also minimises the possibility of damage to the underlining vital structures (neurovascular bundle). So, this technique can be considered for third molar removal in rare circumstances.
[1]. Almendros-Marqués N, Berini-Aytés L, Gay-Escoda C, Influence of lower third molar position on the incidence of preoperative complicationsOral Surg Oral Med Oral Pathol Oral Radiol Endod 217 102(7):725-42.10.1016/j.tripleo.2006.01.00617138172 [Google Scholar] [CrossRef] [PubMed]
[2]. Winter GB, Principles of exodontia as applied to the impacted mandibular third molar 1927 St LouisAmerican Medical Book Co:241-79. [Google Scholar]
[3]. Margarate R, Leary O, Trismus: Modern Pathophysiological CorrelatesAm J Emerg Med 1990 8:220-27.10.1016/0735-6757(90)90327-V [Google Scholar] [CrossRef]
[4]. Eby J, TrismusThe Journal of the National Dental Association 1920 7(8):787-99.10.14219/jada.archive.1920.0131 [Google Scholar] [CrossRef]
[5]. Scully C, Medical problems in dentistry 2014 7th edEdinburghChurchill Livingstone/Elsevier:177 [Google Scholar]
[6]. Alling C, Catone G, Management of impacted teethJ Oral Maxillofac Surg 1994 51(1):04-07.10.1016/0278-2391(93)90004-W [Google Scholar] [CrossRef]
[7]. Toffanin A, Zupi A, Cicognini A, Sagittal split osteotomy in removal of impacted third molarJ Oral Maxillofac Surg 214 71(5):748-40.10.1053/joms.2003.5012412730848 [Google Scholar] [CrossRef] [PubMed]
[8]. Jones T, Garg T, Monaghan A, Removal of a deeply impacted mandibular third molar through a sagittal split ramus osteotomy approachBr J Oral Maxillofac Surg 214 42(4):475-78.10.1016/j.bjoms.2004.02.02215225962 [Google Scholar] [CrossRef] [PubMed]
[9]. Precious D, Removal of third molars with sagittal split osteotomies: The case forJ Oral Maxillofac Surg 214 72(9):1144-47.10.1016/j.joms.2004.04.01415346368 [Google Scholar] [CrossRef] [PubMed]
[10]. Wang C, Kok S, Hou L, Yang P, Lee J, Cheng S, Ectopic mandibular third molar in the ramus region: report of a case and literature reviewOral Surg Oral Med Oral Pathol Oral Radiol Endod 218 105(2):155-71.10.1016/j.tripleo.2007.04.00917764987 [Google Scholar] [CrossRef] [PubMed]
[11]. Larry J Peterson, Principles of oral and maxillofacial surgery 1992 2nd edJB Lippincott:841 [Google Scholar]
[12]. Miloro M, Surgical access for inferior alveolar nerve repairJ Oral Maxillofac Surg 1995 54(10):1224-25.10.1016/0278-2391(95)90642-8 [Google Scholar] [CrossRef]