Introduction
Non alcoholic fatty liver disease is drawing national and global attention because of its increasing prevalence and its association with dreadful diseases leading to long lasting consequences like chronic liver disease and hepatocellular carcinoma. Urbanisation, unhealthy dietary habits and sedentary lifestyle have contributed to the rising prevalence of NAFLD which is recognised as the most common cause of chronic liver disease. It was earlier considered as a disease of the affluent nations, but studies indicate that it is equally prevalent in developing countries like India [1]. Incidence of this disease is expected to rise further in future.
NAFLD includes a spectrum of liver diseases, with a little fat accumulation in the hepatic cells at one end to complete scarring (liver cirrhosis) of the liver and irreversible liver damage at the other. This disease is asymptomatic and is often detected incidentally. Currently, there is no effective drug therapy for reversal of NAFLD, especially when it has progressed to an advanced stage. Lifestyle modifications focusing on healthy diet and physical activity remain the cornerstones for the management of NAFLD at the moment. However, poor compliance to lifestyle related advice limits the effectiveness of these therapies among the patients.
Personal motivation and willingness to change behaviour can play a major role in the success of NAFLD treatment. Knowledge Attitude Behaviour (KAB) model proposes that after being convinced about the accumulated knowledge, people often initiate a change in their attitude, and this results in gradual behaviour change [2]. Knowledge Attitude Practices (KAP) surveys have become common in the community settings to identify the needs, problems, and possible barriers before developing and implementing an intervention. Well designed KAP questionnaires exist for diseases such as diabetes [3,4], and hypertension [5,6]. However, there is a lack of validated and reliable KAP instruments focusing on NAFLD.
The objective of this article is to review the existing literature on the perception of the general public as well as physicians about NAFLD and to understand the gaps in their knowledge, attitude, practices and behaviour towards this disease. The article also aims to explore the strength of an interdisciplinary approach and the potential role of behaviour counselling in dietary and lifestyle intervention as a solution for improving the treatment outcome in NAFLD patients.
NAFLD: Are We Sitting on a Volcano?
NAFLD, which was earlier considered innocuous, is now quietly becoming a global metabolic threat. The disease is associated with poor quality of life and high economic burden on the patients [7]. Population and hospital based studies from the West report that 10 to 24% of the general population, and 57 to 74% of obese individuals may have NAFLD [8,9]. If NAFLD is left unchecked, it can progress to Non Alcoholic Steatohepatitis (NASH). Of all the NAFLD patients, one-tenth to one-fourth may develop NASH, and 5 to 8% of the latter are estimated to develop liver cirrhosis in subsequent five years [10]. Furthermore, 12.8% of patients with liver cirrhosis are prone to develop Hepatocellular Carcinoma (HCC) within three years [11]. Subsequently, the last option is to go for a liver transplant; however, the demand for transplants is much more than the actual availability of livers for the purpose.
By 2020, NASH is projected to overtake hepatitis C as the leading cause of liver transplants in the United States [12]. NAFLD runs in families but often goes undetected for many years in non drinkers [13]. Being asymptomatic, it is precariously ignored until it has progressed to an advanced stage. Unlike diabetes and blood pressure, where patients are ready to seek help and take treatment, NAFLD patients are unaware of the serious repercussions of the disease and are generally not inclined to consult a physician.
Indian Scenario in the Global NAFLD Pandemic and the Need to Contextualise the Treatment
NAFLD is deeply penetrating itself in the Asian subcontinent with rampant increase in obesity, hypertension, and diabetes mellitus [14]. Findings from few published studies carried out in India reveal that 9 to 35% of the Indian population suffers from NAFLD [15,16]. Considering the large population in the country, the absolute number of patients suffering from this silent liver disease in India equals or exceeds the number in the west, despite the prevalence being somewhat lower [17]. Individuals in the age group of 40 to 50 years, especially men, are most affected by NAFLD [18]. Urbanisation, socioeconomic growth, lack of health awareness, sedentary lifestyle and unhealthy dietary habits are the major factors contributing to its high prevalence in India [19].
It has been observed that the Indian population is predisposed to develop NAFLD at a lower Body Mass Index (BMI) than in the west. A strong genetic susceptibility for developing fatty liver has been indicated as the cause for this inter ethnic difference in the prevalence of NAFLD and NASH among Indian and western population [20]. The pathogenesis and clinicopathological profile of Indian patients with NAFLD is different from that of the patients in the west; additionally, the available guidelines from the west for patients with NAFLD may not be applicable to patients with NAFLD in India [20]. The dietary modifications and lifestyle interventions recommended as first line treatment for NAFLD also need to be adapted in the Indian context. Therefore, it is important to contexualise the treatment of Indian NAFLD patients.
NAFLD: Problems in Perception
Though, studies are available from other parts of the world, no Indian study has been carried out till date to document how seriously Indians perceive the problem of NAFLD.
A case-control study, conducted by Mlynarsky L et al., in 2016, concluded that fatty liver without clinically significant liver disease does not have independent impact on self health perception. The findings indicated that NAFLD diagnosis is not associated with higher healthcare utilisation. Further, the diagnosed patients did not predict any health deterioration over the coming years [21]. Another community based study involving 227 subjects in Singapore found that majority of the subjects had superficial awareness of NAFLD and did not perceive the risk of developing this disease. The authors highlighted the need for enhanced public education and screening to improve the understanding of NAFLD among the general population [22]. Yet another study, carried out on 5000 subjects in USA, showed lack of awareness about NAFLD among a large majority of the respondents who reported that their physicians had never discussed the said disease with them [23]. This study also underscored the urgent need for initiating education campaign for physicians and the general population to increase their awareness about this liver disease.
Since, NAFLD is not yet perceived as a serious disease, its potential risks are often overlooked in vulnerable individuals. Available data underlines the fact that there is a dire need for carrying out research on self-rated health perception among NAFLD patients, particularly in the Indian context.
Are Physicians Tackling the Situation Correctly?
General practitioners are the first point of medical consultation for majority of patients with or ‘at risk’ of NAFLD. Their (particularly non hepatologists’) awareness and attitude are crucial for motivating the patients to adopt healthy lifestyle and sustain it for a long period. There is scant information in the literature about physicians’ awareness about NAFLD diagnosis and management [24]. The available studies [Table/Fig-1] indicate that it is restricted and inadequate [25,26]. A study from the US reports that many doctors do not recognise NAFLD as a clinically relevant diagnosis [27]. The gap in awareness and perception of primary care practitioners can be detrimental in optimising patient care. For example, screening guidelines and position papers for NAFLD exist, but many practitioners are often unaware of these important guidelines [28]. According to a survey carried out in the US, many primary care practitioners do accept NAFLD as a major public health problem, but they have self-reported lack of confidence in their knowledge about this disease. The survey also found that the physicians’ knowledge on prevalence of the disease, identification of associated conditions, and screening of NAFLD was inadequate. Less time, cost of diagnosis and evaluation, lack of confidence in initial assessment, lack of referral to specialists and unclear responsibility for screening were some of the identified barriers to patient care [29].
Studies of Physician Awareness about NAFLD
| Author, Year | Type of study | Subjects | Aim of study | Results and conclusions |
|---|
| Grattagliano I et al., 2008 [25] | Pre and post study design | 56 General practitioners | To assess the impact of an education training program for general practitioners in NAFLD | General practitioners knowledge about NAFLD is barely adequate; thus, targeted training is essential to improve their knowledge and practice. |
| Bergqvist et CJ al., 2013 [26] | Survey | 100 Clinicians (non hepatologists) at two major tertiary hospitals | To assess the awareness about NAFLD and opinions regarding management among non hepatologists at two major tertiary hospitals in Brisbane | Non hepatologists appreciate the seriousness of NAFLD but appear to underestimate its prevalence, especially among their own patients despite known risk factors.More can be done to improve the understanding of this disease among non hepatologists. |
| Wieland AC et al., 2013 [27] | Online survey | 479 Primary care practitioners (PCPs) in Internal Medicine, Family Medicine, Endocrinology, Cardiology, Gynaecology | To investigate the understanding of PCPs with respect to diagnosis and management of NAFLD | Majority do not identify NAFLD as a clinically important diagnosis and do not refer patients to a hepatologist.83% expressed need for education on NAFLD. |
| Said A et al., 2013 [29] | State-wide stratified survey | 250 Primary Care Practitioners | To understand knowledge, attitudes and practices regarding NAFLD and the barriers to providing care for this condition | Majority of participants perceived NAFLD as an important health issue in their practice.A major barrier to managing these patients was self-reported lack of knowledge about NAFLD. |
| Ratziu V et al., 2012 [30] | Survey | 352 Gastroenterologists | To understand the clinical burden, perceived severity, and management patterns of NAFLD. | Most at risk patients are currently missed because of non referral by endocrinologists and no exploration of those with normal aminotransferases. The medical need for the diagnosis and treatment of NAFLD is real in the community of gastroenterologists at large. |
| Iacob S et al., 2016 [31] | Cross-sectional observational study | 102 Gastroenterologists | To assess current diagnostic and treatment patterns of management of NAFLD | Clinical practice patterns among Romanian gastroenterologists for the diagnosis and management of NAFLD frequently diverge from published practice guidelines. |
| Polanco-Briceno S et al., 2016 [32] | Online survey | 302 physicians (152 Primary care physicians, 150 Specialists) | To assess their current practices regarding various liver conditions | More education on the recent practice guidelines for NAFLD and non alcoholic steatohepatitis is needed for the physicians. |
The seriousness of NAFLD as perceived by physicians can play an important role in the follow up and treatment of ‘at-risk’ patients. Despite the known high risk factors in obese and diabetic patients, non hepatologists underestimate the prevalence and severity of NAFLD in their patients [26]. A study, carried out in France, has shown that most ‘at-risk’ patients of NAFLD are currently missed because of non referral by endocrinologists and no exploration of those with normal aminotransferases.
In view of their limited awareness about NAFLD, there is an urgent need to improve the understanding of this disease among the physicians (especially the non hepatologists). This is important for appropriate referral of patients to Hepatology Clinics and the correct treatment of patients who are at risk of developing NAFLD [26]. It is also important to educate the physicians about the recent practice guidelines for NAFLD and NASH [32]. A large majority of physicians have clearly expressed their inclination to learn the skills required for correct screening, diagnosis and management of NAFLD, through targeted medical education programmes [27].
Diet and Lifestyle Counselling for NAFLD Patients
Calorie reduction is regarded as the most important factor in facilitating weight loss in a NAFLD patient regardless of the type of diet a person consumes [33]. Changing the dietary composition even without weight loss can also reduce steatosis and improve metabolic alterations such as insulin resistance and lipid profile [34]. Low calorie diets have proven to show beneficial results in NAFLD patients, but continuous support and regular monitoring is required to maintain adherence to these dietary prescriptions. The Mediterranean Diet (MD) pattern has been recommended as the diet of choice for the treatment of NAFLD by the EASL-EASD-EASO Clinical Practice Guidelines [34]. In view of supporting scientific evidence, restricting fructose, trans fatty acids and saturated fats is recommended in NAFLD patients. For long term weight loss maintenance, a general healthy balanced diet is recommended [35].
Physical activity targets that have been set for NAFLD/NASH patients are in accordance to the targets described in the diabetes prevention trials [36]. It is recommended that NAFLD patients should engage themselves in at least 150 minutes per week of moderate intensity physical activity (e.g., brisk walking) and a minimum of 75 minutes per week of vigorous-intensity physical activity (e.g., jogging), along with muscle strengthening activities twice a week. However, each patient must receive individualised counselling for physical activity based on their age, gender and health status. Even limited physical activity is better than none; therefore, any increase over baseline should be encouraged [36].
Barriers in Compliance to Diet and Lifestyle Related Advice Given to NAFLD Patients
A weight loss goal of 10% of current body weight is recommended for patients with NAFLD [37]. However, long term data indicate that only 15% of participants achieve the goal of 10% body weight reduction and adherence drops after the initial few months. Most of these patients regain the lost weight [38].
There is ample evidence to prove that behavioural intervention targeting diet and physical activity is effective in treating such patients. However, NAFLD patients are unwilling to accept lifestyle changes, especially in terms of physical activity [39]. Compliance to prescription is poor and a major challenge for medical caregivers is to motivate these patients to make long term changes in their lifestyle [34].
The primary reason for reluctance of NAFLD patients to diet and lifestyle related treatment is the inadequate awareness about the progression and possible fatal consequences of the disease. Secondly, patients with NAFLD are advised by clinicians to lose weight without any meaningful and continuous support to make changes in their lifestyle behaviours. Physicians’ negative attitudes toward patients with obesity are well documented [40]. Low levels of emotional rapport in primary care visits with overweight and obese patients may also diminish patients’ adherence to recommendations, and decrease the effectiveness of behaviour change counselling [40]. Frequent unsuccessful weight loss attempts lead to disappointment among the patients. Also, conflicting information from health care professionals, friends, family members, and internet, results in further confusion in the minds of these patients, about the advice to follow [40].
Improving Patient Compliance - Need for an Interdisciplinary Approach
To reduce non compliance to prescription in NAFLD, it is pertinent to have holistic contributions from an interdisciplinary team of physicians, dietitians, clinical psychologists, patients and care givers. “Patient-centred” clinical care [Table/Fig-2] involving a two-way conversation with the patient can bring about more successful treatment outcome [34].
Flow diagram outlining the process for targeting lifestyle behaviour change during NAFLD consultations.
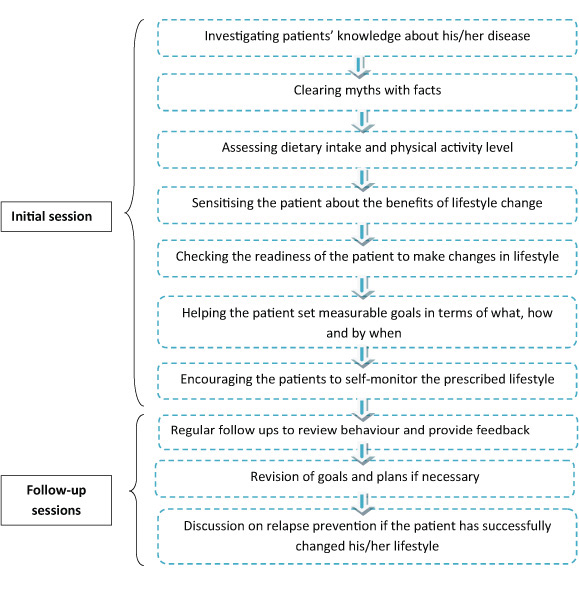
Each member of the multidisciplinary team should have a well defined role to play. The treatment should begin with sensitisation of the patients so that they understand their diagnosis well. It is important that the physician explains this liver disease to the NAFLD patients along with the possible causes, and effective ways to control or reverse its progression. The medical caregiver should try to understand the previous experiences and attempts of the patients for changing their lifestyle and behaviour. Such an approach will help them in addressing the barriers in treatment and improve compliance.
As dietary modification leading to weight loss is the first line of treatment, the dietitian must play a proactive role in the interdisciplinary team to treat NAFLD. His/her role includes helping patients identify their dietary goals and reach therapeutic targets, through effective and individualised weight management plans. Correct knowledge and a serious attitude towards NAFLD from the dietitians may be a key factor in how patients perceive the seriousness of the condition and thereby, affecting the compliance to the prescribed diet.
Integrated multidisciplinary approaches that address psychiatric needs and provide behavioural support for weight loss may help patients with NAFLD implement sustained lifestyle changes [41]. This highlights the role of a clinical psychologist in the team.
The caregivers and family members of a patient diagnosed with NAFLD are expected to have inadequate knowledge and a non serious attitude towards the disease condition, thereby affecting the practices of the patient. Thus, to ensure successful treatment, it is important to keep the patient and his caregivers at a central position.
Potential Role of Cognitive Behaviour Therapy in Achieving Diet and Physical Activity Targets among NAFLD
Cognitive Behaviour Therapy (CBT) is an upcoming promising component which should be added to the interdisciplinary approach to tackle NAFLD. This approach has been extensively used in treatment of obesity and other metabolic diseases. Nevertheless, the effectiveness of CBT in (NAFLD) remains mainly unexplored so far [42].
Besides enabling the patients to achieve their diet and physical activity targets, CBT also assures long term sustainability of change. The behaviour component of lifestyle modification for weight loss includes self-monitoring, goal setting, stimulus control, alternative behaviours, problem solving and cognitive restructuring [Table/Fig-3].
Components of a cognitive behaviour therapy sessions for NAFLD
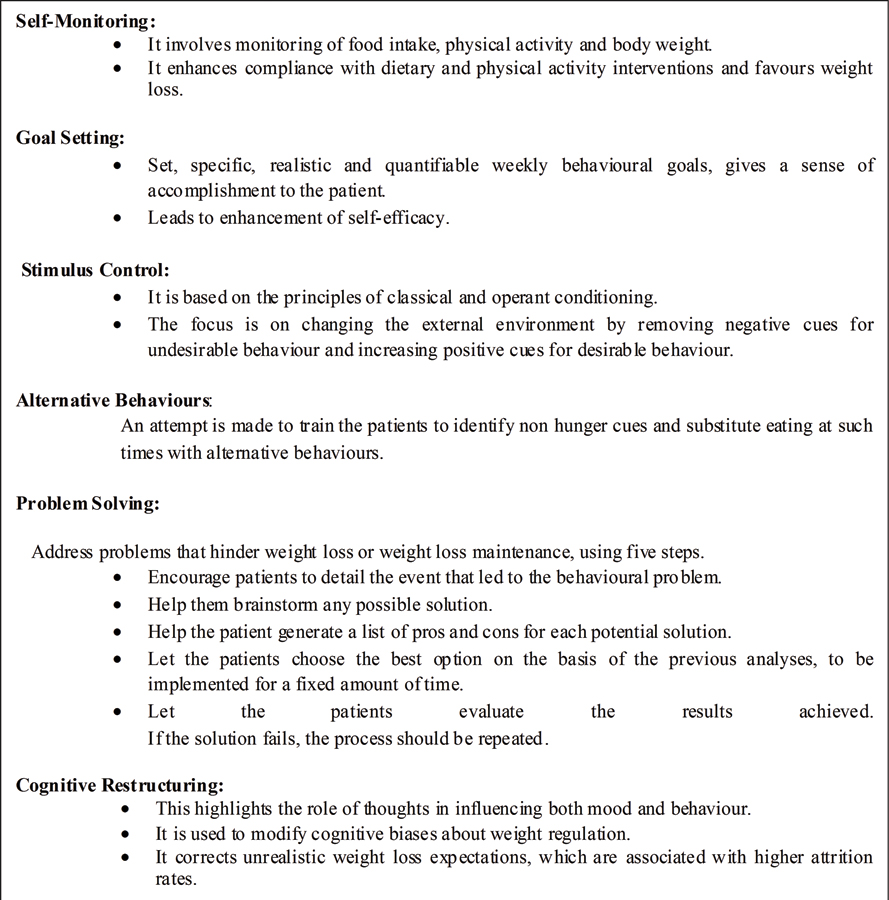
CBT requires a well defined program, the availability of manuals for both patients and therapists, and a team to address both the physical and the psychological needs of patients. The team must include physicians, as well as dietitians, psychologists, trained nurses, experts of physical exercise, working on individual patients or on groups with multiple sessions over several months. The major challenge is the cost, time associated with a team approach and multiple session treatments. Also, the skills and the logistics to carry out a cognitive behaviour approach to diseases are beyond the scope of many hospitals and clinics [43].
General practitioners, hepatologists and dietitians need to undergo training in behaviour therapy. A Canadian study, published in the year 2014 regarding the views and practices of 514 dietitians regarding obesity and weight management, reported that these dietitians wanted to learn more about motivational and behavioural modification counselling techniques, to help bring better and sustainable weight loss results in their clients [44].
The interdisciplinary team needs to communicate with their NAFLD patients more about the broader picture of complications; hepatocellular cancer, increased risk of diabetes, heart attack or stroke, with the message that risk reduction is possible. The physicians/dietitians may use the 5 A’s model (ask, advise, assess, assist, and arrange) while advising NAFLD patients to modify their behaviour, assessing their willingness for doing so, assisting in their behaviour change efforts, and arranging timely and regular follow up for them [45]. CBT, if added along with regular dietary and lifestyle counselling should help improve dietary compliance and also lead to sustained weight loss over a longer period of time [46].
Conclusion
Correct perception about NAFLD and adoption of an interdisciplinary and multifaeted approach for its effective treatment can go a long way in controlling this growing epidemic. CBT is likely to be an effective solution to NAFLD if delivered in an interdisciplinary team setup; although, evidence based tools and training are lacking. Trials exploring the potential effect of CBT as an additive therapy in NAFLD patients call for fervent endeavours.
[1]. Amarapurkar D, Kamani P, Patel N, Gupte P, Kumar P, Agal S, Prevalence of non-alcoholic fatty liver disease: population based studyAnn Hepatol 2007 6(3):161-63.10.1016/S1665-2681(19)31922-2 [Google Scholar] [CrossRef]
[2]. Hiew C, Chin Y, Chan Y, Mohd NM, Development and validation of Knowledge, Attitude and Practice on Healthy Lifestyle Questionnaire (KAP-HLQ) for Malaysian adolescentsJournal of Nutrition and Health Sciences 2015 2(4):01-11.10.15744/2393-9060.2.407 [Google Scholar] [CrossRef]
[3]. Upadhyay DK, Palaian S, Shankar PR, Mishra P, Pokhara N, Knowledge, attitude and practice about diabetes among diabetes patients in Western NepalRawal Med J 2008 33(1):08-11. [Google Scholar]
[4]. Shera AS, Jawad F, Basit A, Diabetes related knowledge, attitude and practices of family physicians in PakistanJ Pak Med Assoc (JPMA) 2002 Available from http://www.jpma.org.pk/PdfDownload/2425.pdf (Accessed on 25th August, 2017) [Google Scholar]
[5]. Akl OA, Khairy AE, Abdel-Aal NM, Deghedi BS, Amer ZF, Knowledge, attitude, practice and performance of family physicians concerning holistic management of hypertensionJ Egypt Public Health Assoc 2006 81(5&6):337-53. [Google Scholar]
[6]. Parmar P, Rathod GB, Rathod S, Goyal R, Aggarwal S, Parikh A, Study of knowledge, attitude and practice of general population of Gandhinagar towards hypertensionInternational Journal of Current Microbiology and Applied Sciences 2014 3(8):680-85. [Google Scholar]
[7]. Golabi P, Otgonsuren M, Cable R, Felix S, Koenig A, Sayiner M, Non-alcoholic fatty liver disease (NAFLD) is associated with impairment of Health Related Quality of Life (HRQOL)Health and Quality of Life Outcomes 2016 14(1):1810.1186/s12955-016-0420-z26860700 [Google Scholar] [CrossRef] [PubMed]
[8]. Sanyal AJ, American Gastroenterological AssociationAGA technical review on nonalcoholic fatty liver diseaseGastroenterology 2002 123:1705-25.10.1053/gast.2002.3657212404245 [Google Scholar] [CrossRef] [PubMed]
[9]. Neuschwander-Tetri BA, Caldwell SH, Nonalcoholic steatohepatitis: summary of an AASLD single topic conferenceHepatology 2003 37:1202-19.10.1053/jhep.2003.5019312717402 [Google Scholar] [CrossRef] [PubMed]
[10]. Milić S, Stimac D, Nonalcoholic fatty liver disease/steatohepatitis: epidemiology, pathogenesis, clinical presentation and treatmentDig Dis 2012 30:158-62.10.1159/00033666922722431 [Google Scholar] [CrossRef] [PubMed]
[11]. White DL, Kanwal F, El-Serag HB, Association between nonalcoholic fatty liver disease and risk for hepatocellular cancer, based on systematic reviewClin Gastroenterol Hepatol 2012 10:1342-59.10.1016/j.cgh.2012.10.00123041539 [Google Scholar] [CrossRef] [PubMed]
[12]. Charlton M, Nonalcoholic fatty liver disease: a review of current understanding and future impactClin Gastroenterol Hepatol 2004 2(12):1048-58.10.1016/S1542-3565(04)00440-9 [Google Scholar] [CrossRef]
[13]. Schwimmer JB, Celedon MA, Lavine JE, Salem R, Campbell N, Schork NJ, Heritability of nonalcoholic fatty liver diseaseGastroenterology 2009 136(5):1585-92.10.1053/j.gastro.2009.01.05019208353 [Google Scholar] [CrossRef] [PubMed]
[14]. Fu CC, Chen MC, Li YM, Liu TT, Wang LY, The risk factors for ultrasound-diagnosed non-alcoholic fatty liver disease among adolescentsAnn Acad Med Singapore 2009 38:15-17. [Google Scholar]
[15]. Mohan V, Farooq S, Deepa M, Ravikumar R, Pitchumoni C, Prevalence of non-alcoholic fatty liver disease in urban south Indians in relation to different grades of glucose intolerance and metabolic syndromeDiabetes Res Clin Pract 2009 84(1):84-91.10.1016/j.diabres.2008.11.03919168251 [Google Scholar] [CrossRef] [PubMed]
[16]. Singh S, Kuftinec GN, Sarkar S, Non-alcoholic fatty liver disease in South Asians: a review of the literatureJ Clin Trans l Hepatol 2017 5(1):76-81.10.14218/JCTH.2016.0004528507930 [Google Scholar] [CrossRef] [PubMed]
[17]. De Silva HJ, Dassanayake AS, Non alcoholic fatty liver disease: confronting the global epidemic requires better awarenessJ Gastroenterol Hepatol 2009 24(11):1705-07.10.1111/j.1440-1746.2009.06026.x20136955 [Google Scholar] [CrossRef] [PubMed]
[18]. Duseja A, Nonalcoholic fatty liver disease in India–a lot done, yet more requiredIndian J Gastroenterol 2010 29(6):217-25.10.1007/s12664-010-0069-121191681 [Google Scholar] [CrossRef] [PubMed]
[19]. Singh SP, Singh A, Misra D, Misra B, Pati GK, Panigrahi MK, Risk factors associated with non-alcoholic fatty liver disease in Indians: a case-control studyJ Clin Exp Hepatol 2015 5(4):295-302.10.1016/j.jceh.2015.09.00126900270 [Google Scholar] [CrossRef] [PubMed]
[20]. Duseja A, Singh SP, Saraswat VA, Acharya SK, Chawla YK, Chowdhury S, Non-alcoholic fatty liver disease and metabolic syndrome-position paper of the Indian National Association for the Study of the Liver, Endocrine Society of India, Indian College of Cardiology and Indian Society of GastroenterologyJournal of Clinical and Experimental Hepatology 2015 5(1):51-68.10.1016/j.jceh.2015.02.00625941433 [Google Scholar] [CrossRef] [PubMed]
[21]. Mlynarsky L, Schlesinger D, Lotan R, Webb M, Halpern Z, Santo E, Non-alcoholic fatty liver disease is not associated with a lower health perceptionWorld Journal of Gastroenterology 2016 22(17):4362-72.10.3748/wjg.v22.i17.436227158205 [Google Scholar] [CrossRef] [PubMed]
[22]. Goh GB, Kwan C, Lim SY, Venkatanarasimha NK, Abu-Bakar R, Krishnamoorthy TL, Perceptions of non-alcoholic fatty liver disease-an Asian community based studyGastroenterol Rep 2015 4(2):131-35.10.1093/gastro/gov04726463276 [Google Scholar] [CrossRef] [PubMed]
[23]. Ghevariya V, Sandar N, Patel K, Ghevariya N, Shah R, Aron J, Knowing what’s out there: awareness of non-alcoholic fatty liver diseaseFront Med 2014 1:4Available from: https://dx.doi.org/10.3389%2Ffmed.2014.00004 (Accessed on 24th June 2017)10.3389/fmed.2014.0000425798442 [Google Scholar] [CrossRef] [PubMed]
[24]. Kallman JB, Arsalla A, Park V, Dhungel S, Bhatia P, Haddad D, Screening for hepatitis B, C and non alcoholic fatty liver disease: a survey of community based physiciansAliment Pharmacol Ther 2009 29(9):1019-24.10.1111/j.1365-2036.2009.03961.x19220207 [Google Scholar] [CrossRef] [PubMed]
[25]. Grattagliano I, D’Ambrosio G, Palmieri VO, Moschetta A, Palasciano G, Portincasa P, Improving nonalcoholic fatty liver disease management by general practitioners: a critical evaluation and impact of an educational training programJ Gastrointestin Liver Dis 2008 17(4):389-94. [Google Scholar]
[26]. Bergqvist CJ, Skoien R, Horsfall L, Clouston AD, Jonsson JR, Powell EE, Awareness and opinions of non alcoholic fatty liver disease by hospital specialistsIntern Med J 2013 43(3):247-53.10.1111/j.1445-5994.2012.02848.x22646061 [Google Scholar] [CrossRef] [PubMed]
[27]. Wieland AC, Quallick M, Truesdale A, Mettler P, Bambha KM, Identifying practice gaps to optimize medical care for patients with nonalcoholic fatty liver diseaseDig Dis Sci 2013 58(10):2809-16.10.1007/s10620-013-2740-823843097 [Google Scholar] [CrossRef] [PubMed]
[28]. Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Why don’t physicians follow clinical practice guidelines? :A framework for improvementJ Am Med Assoc 1999 282(15):1458-65.10.1001/jama.282.15.145810535437 [Google Scholar] [CrossRef] [PubMed]
[29]. Said A, Gagovic V, Malecki K, Givens ML, Nieto FJ, Primary care practitioners survey of non-alcoholic fatty liver diseaseAnn Hepatol 2013 12(5):758-65.10.1016/S1665-2681(19)31317-1 [Google Scholar] [CrossRef]
[30]. Ratziu V, Cadranel JF, Serfaty L, Denis J, Renou C, Delassalle P, A survey of patterns of practice and perception of NAFLD in a large sample of practicing gastroenterologists in FranceJ Hepatol 2012 57(2):376-83.10.1016/j.jhep.2012.03.01922521354 [Google Scholar] [CrossRef] [PubMed]
[31]. Iacob S, Ester C, Lita M, Ratziu V, Gheorghe L, Real-life perception and practice patterns of NAFLD/NASH in Romania: results of a survey completed by 102 board-certified gastroenterologistsJ Gastrointestin Liver Dis 2016 25(2):183-89.10.15403/jgld.2014.1121.252.naf [Google Scholar] [CrossRef]
[32]. Polanco-Briceno S, Glass D, Stuntz M, Caze A, Awareness of nonalcoholic steatohepatitis and associated practice patterns of primary care physicians and specialistsBMC Res Notes 2016 9(1):15710.1186/s13104-016-1946-126969270 [Google Scholar] [CrossRef] [PubMed]
[33]. Hallsworth K, Avery L, Trenell MI, Targeting lifestyle behavior change in adults with NAFLD during a 20-min consultation: summary of the dietary and exercise literatureCurr Gastroenterol Rep 2016 18(3):1110.1007/s11894-016-0485-126908279 [Google Scholar] [CrossRef] [PubMed]
[34]. ZelberSagi S, Salomone F, Mlynarsky L, The Mediterranean dietary pattern as the diet of choice for NAFLD; evidence and plausible mechanismsLiver Int 2017 37(7):936-49.10.1111/liv.1343528371239 [Google Scholar] [CrossRef] [PubMed]
[35]. Ratziu V, Bellentani S, Cortez-Pinto H, Day C, Marchesini G, A position statement on NAFLD/NASH based on the EASL 2009 special conferenceJ Hepatol 2010 53(2):372-84.10.1016/j.jhep.2010.04.00820494470 [Google Scholar] [CrossRef] [PubMed]
[36]. Orchard TJ, Temprosa M, Goldberg R, Haffner S, Ratner R, Marcovina S, The effect of metformin and intensive lifestyle intervention on the metabolic syndrome: the Diabetes Prevention Program randomized trialAnn Intern Med 2005 142(8):611-19.10.7326/0003-4819-142-8-200504190-0000915838067 [Google Scholar] [CrossRef] [PubMed]
[37]. Dyson JK, Anstee QM, McPherson S, Republished: Non-alcoholic fatty liver disease: a practical approach to treatmentPostgrad Med J 2015 91(1072):92-101.10.1136/postgradmedj-2013-100404rep25655252 [Google Scholar] [CrossRef] [PubMed]
[38]. Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, Comparison of weight-loss diets with different compositions of fat, protein, and carbohydratesNew Engl J Med 2009 360(9):859-73.10.1056/NEJMoa080474819246357 [Google Scholar] [CrossRef] [PubMed]
[39]. Centis E, Moscatiello S, Bugianesi E, Bellentani S, Fracanzani AL, Calugi S, Stage of change and motivation to healthier lifestyle in non-alcoholic fatty liver diseaseJ Hepatol 2013 58(4):771-77.10.1016/j.jhep.2012.11.03123201248 [Google Scholar] [CrossRef] [PubMed]
[40]. Gudzune KA, Beach MC, Roter DL, Cooper LA, Physicians build less rapport with obese patientsObesity 2013 21(10):2146-52.10.1002/oby.2038423512862 [Google Scholar] [CrossRef] [PubMed]
[41]. Stewart KE, Haller DL, Sargeant C, Levenson JL, Puri P, Sanyal AJ, Readiness for behaviour change in non alcoholic fatty liver disease: implications for multidisciplinary care modelsLiver Int 2015 35(3):936-43.10.1111/liv.1248324521540 [Google Scholar] [CrossRef] [PubMed]
[42]. Moscatiello S, Luzio R, Bugianesi E, Suppini A, Hickman IJ, Domizio S, Cognitive behavioral treatment of nonalcoholic fatty liver disease: a propensity score adjusted observational studyObesity 2011 19(4):763-70.10.1038/oby.2010.25420966900 [Google Scholar] [CrossRef] [PubMed]
[43]. Marchesini G, Suppini A, Forlani G, NAFLD treatment: Cognitive-behavioral therapy has entered the arenaJ Hepatol 2005 43(6):926-28.10.1016/j.jhep.2005.09.00516246450 [Google Scholar] [CrossRef] [PubMed]
[44]. Barr SI, Yarker KV, Levy-Milne R, Chapman GE, Canadian dietitians’ views and practices regarding obesity and weight managementJ Hum Nutr Diet 2004 17(6):503-12.10.1111/j.1365-277X.2004.00562.x15546427 [Google Scholar] [CrossRef] [PubMed]
[45]. Vallis M, Piccinini-Vallis H, Sharma AM, Freedhoff Y, Modified 5 As: minimal intervention for obesity counseling in primary careCan Fam Physician 2013 59(1):27-31. [Google Scholar]
[46]. Bellentani S, Dalle Grave R, Suppini A, Marchesini G, Behavior therapy for nonalcoholic fatty liver disease: the need for a multidisciplinary approachHepatology 2008 47(2):746-54.10.1002/hep.2200918098321 [Google Scholar] [CrossRef] [PubMed]