A Rare Association of Aqueductal Stenosis with Subependymal Heterotopia
Pooja Gupta1, Kamlesh Kumar Singh2, Satish Mendonca3
1 Assistant Professor, Department of Radiodiagnosis and Imaging, Armed Forces Medical College, Pune, Maharashtra, India.
2 Assistant Professor, Department of Pathology and Laboratory Science, Armed Forces Medical College, Pune, Maharashtra, India.
3 Professor Medicine, Department of Nephrology, Army Base Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pooja Gupta, Assistant Professor, Department of Radiodiagnosis and Imaging, Armed Forces Medical College, Pune-411040, Maharashtra, India.
E-mail: pooja1306@gmail.com
Aqueductal stenosis is one of the known causes of hydrocephalus and the most common cause of congenital hydrocephalus. Gray matter heterotopias are malformations of cortical development where the migration of neurons along specialized glial cells from near the ventricle to the cortex is interrupted, causing "normal neurons in abnormal locations". In this case report we have a case of a two-year-old girl who presented with obstructive hydrocephalus due to a stenosis in the aqueduct associated with nodular grey matter heterotopias along the walls of occipital and temporal horns of both lateral ventricles. We hereby describe the characteristic radiological features along with a review of the relevant literature.
Aqueduct of sylvius, Cortex, Hydrocephalus, Magnetic resonance imaging
Case Report
The patient was a two-year-old girl, born to non consanguineous parents, presented with history of delayed motor milestones. There was no history of increased sleepiness, episodic vomiting, reduced activity, poor feeding, failure to thrive or seizures. On examination the head circumference was mildly increased. The rest of the neurological examination was within normal limits. The child was born at full term, cried after birth and had no obvious birth defects. Antenatal history of the mother was uneventful and she underwent one fetal ultrasound scan at 19 weeks of gestation which was normal. No further scans were done during the period of gestation. In view of history of delayed milestones, the child was subjected to Magnetic Resonance Imaging (MRI) of the brain which showed dilatation of both the lateral ventricles with absence of septum pellucidum [Table/Fig-1]. The third ventricle was also dilated with ballooning of its walls [Table/Fig-2]. The corpus callosum was displaced superiorly and thinned out. There was narrowing noted in the aqueduct [Table/Fig-3]. The fourth ventricle was normal in size. There was presence of nodular heterotopic grey matter in the walls of occipital and temporal horns of both lateral ventricles [Table/Fig-4]. The cerebral hemispheres revealed normal morphology and signal characteristics. Following the diagnosis the child was taken up for surgery and a ventriculo-peritoneal shunting was done to decompress the hydrocephalus. A postoperative repeat MRI of the brain showed significant decrease in hydrocephalus. Presently almost a year after the surgery the child is asymptomatic and is on follow up in Paediatric Outpatient Department.
MRI Brain Axial T2W1 image showing dilatation of both lateral.

MRI brain axial T2W1 image showing dilatation of third ventricle (red arrow).

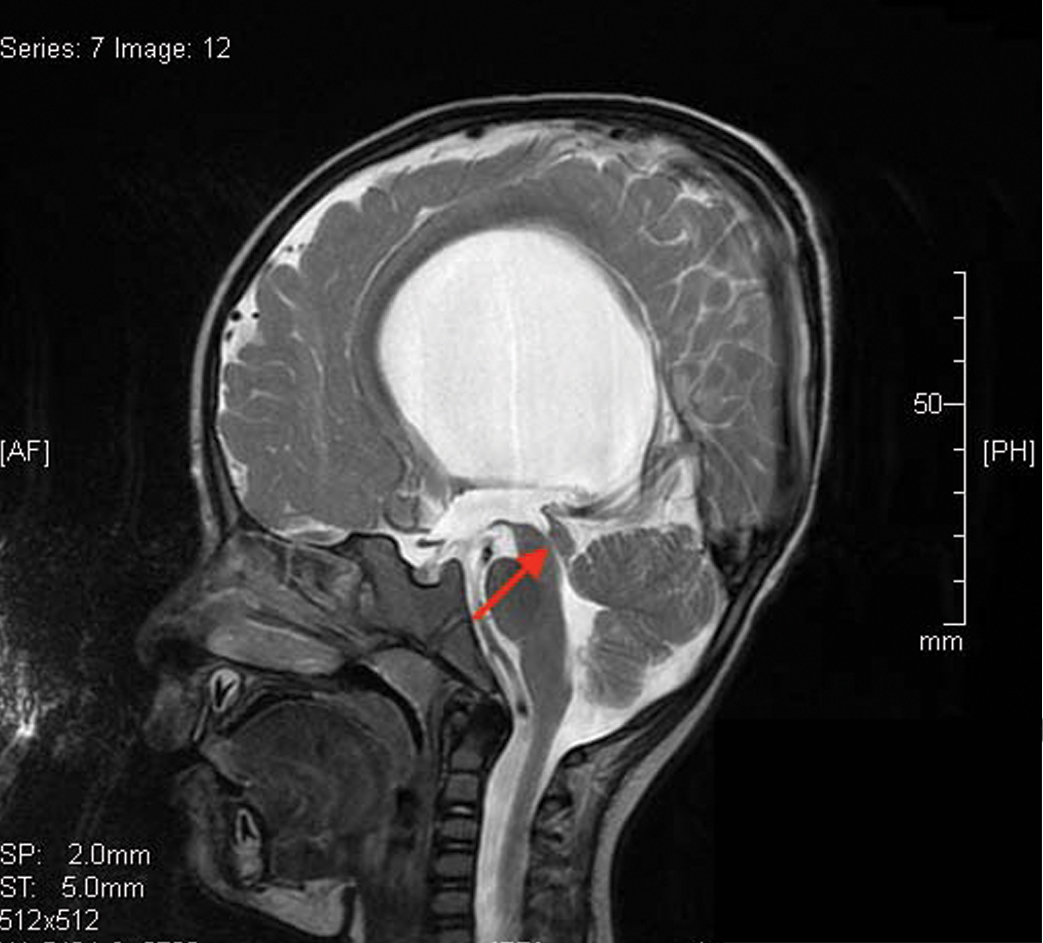
MRI brain midsagittal T2W1 image showing narrowing of the aqueduct (red arrow) with the corpus callosum displaced superiorly and thinned out.
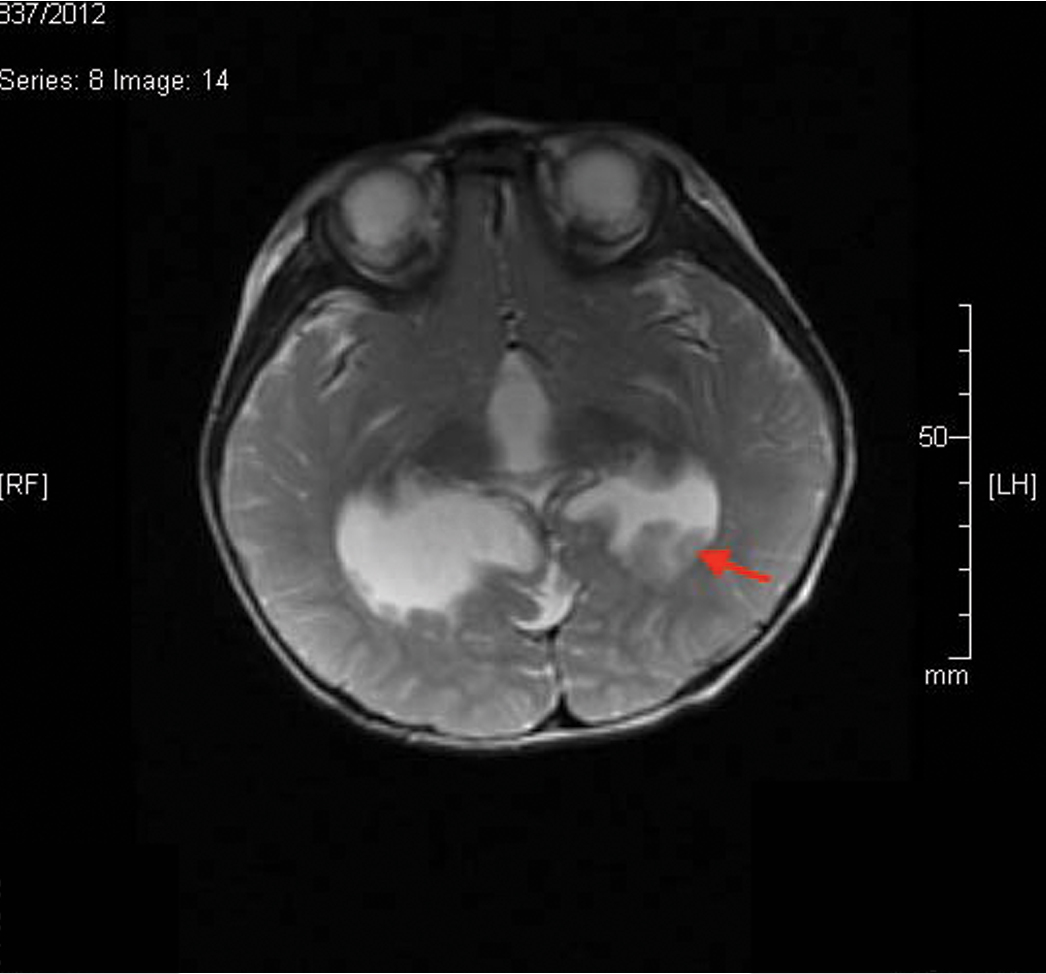
MRI brain axial T2W1 image showing presence of nodular heterotopic grey matter in the walls of occipital horns of both lateral ventricles (red arrow).
Discussion
Congenital hydrocephalus is one of the most common anomalies of the central nervous system. This condition usually develops by the twentieth week of gestation, and the defect can occur either alone or in association with other abnormalities of the neural axis. There are two types of hydrocephalus; communicating hydrocephalus in which there is a defect in the reabsorption of Cerebrospinal Fluid (CSF) or non- communicating hydrocephalus in which there is a block in the normal flow of CSF pathway. Aqueductal stenosis is the most common cause of congenital obstructive hydrocephalus [1]. Aqueductal stenosis results from narrowing of the aqueduct of sylvius, an opening that connects the third and fourth ventricles in the brain. It is located between the pons and the cerebellum. Hydrocephalus is the first complication of aqueductal stenosis which is defined as an enlargement of head due to obstruction to bulk flow of CSF. This causes enlargement of the ventricles with pressure on the surrounding brain tissue causing enlargement of head and shrinking of the brain [2]. In infants, hydrocephalus presents with symptoms of enlargement of head, irritability, poor feeding and slow attainment of milestones. In children there is presence of headache, vomiting, diplopia, lethargy, gait disturbances, deterioration in level of consciousness leading to coma and death in severe cases [3]. Imaging with Computed Tomography (CT) and MRI will show dilated lateral and third ventricles with marked upward bowing of corpus callosum as was also seen in our case. The normal aqueductal CSF flow void in MRI will not be seen, indicating obstruction to CSF flow through the aqueduct [4].
Grey matter heterotopias are clusters of neurons which are arrested during their migration from the periventricular region to the cortex. They appear as nodules or bands, and may be subpial, subcortical or subependymal in location [5].
Periventricular heterotopia represents a heterogeneous group of migrational disorders, characterized by grey matter nodules that are located ectopically along the lateral ventricular walls. When in a subependymal location, the nodules may either be discrete or in clusters or bands adjacent to the lateral ventricles, often bilaterally and symmetrically. It has been seen that subependymal heterotopia is the commonest form of grey matter heterotopia, at least in the adult population, based on imaging alone. Symptomatic patients with subependymal heterotopia typically present with partial epilepsy during the second decade of life; development and neurologic examinations up to that point are typically normal. Subependymal heterotopia is well diagnosed by neuroimaging [6,7]. It is very well delineated on MRI as compared to CT. On CT, irregularities along the lateral walls of the lateral ventricles may be the only clue to the diagnosis of subependymal heterotopias. MRI shows the extent, morphology and location of subependymal heterotopias. The nodules of heterotopia are isointense to grey matter on all sequences and like normal grey matter do not show post contrast enhancement. Differential diagnosis of subependymal heterotopias includes subependymal tubers of tuberous sclerosis and subependymal giant cell astrocytoma. However, the subependymal tubers of tuberous sclerosis are calcified (except in childhood), have higher T2W1 signal intensity than grey matter and other stigmata of tuberous sclerosis are usually present. Subependymal giant cell astrocytomas are located at or near the foramen of Monro, enhance brightly with contrast and are usually seen in association with tuberous sclerosis [8].
In our case, MRI brain showed nodules which were isointense to grey matter in the occipital and temporal horns of both the lateral ventricles.
Treatment of aqueductal stenosis is aimed at relieving the hydrocephalus by inserting a ventriculo-peritoneal shunt or performing an endoscopic third ventriculostomy or an endoscopic aqueductoplasty and stent placement. Management of heterotopias is aimed at controlling the clinical manifestations associated with them, commonly seizures.
Although, aqueductal stenosis and periventricular heterotopias are not very rare entities by themselves, however the association of these two entities is rare and there are not many cases of their association in literature. Pepe E et al., reported a case of an Italian boy, born to normal and non consanguineous parents with presence of aqueductal stenosis and subependymal glial heterotopias. The child also had bilateral macrostomia without other evident facial anomalies. Antenatal ultrasound examination of the mother was performed every month considering the mothers age (40-year-old). It was normal till 36 weeks when the scan showed dilatation of the third ventricle and of the lateral ventricles. Prenatal MRI confirmed mild triventricular dilataion and revealed glial heterotopic nodules [9]. Sheen VL et al., in their study mentioned three different cases of periventricular heterotopia with a genetic basis for the heterotopia along with presence of different kinds of hydrocephalus [10]. Manganaro L et al., reported two cases of subependymal heterotopias associated with ventriculomegaly and cerebellar abnormalities diagnosed by fetal MRI in two cases at 20 and 23 weeks gestation respectively [11]. Bargallo N et al., reported a case of bilateral nodular heterotopia associated with mega cisterna magna diagnosed by ultrasound and MRI in a 26-year-old primigravida woman at 29 weeks’ gestation [12]. Srour M et al., reviewed 31 patients with pathology or imaging confirmed nodular heterotopias and studied their associated systemic and cerebral malformations. Nine of these patients had associated ventriculomegaly which was more common in unilateral focal nodular heterotopias than in bilateral heterotopias [13]. No cases of this unusual association have however been reported in India.
In most of these studies heterotopias were not detected on routine antenatal scans and were diagnosed only on diagnostic MRI performed in symptomatic patients. However, hydrocephalus could be detected on antenatal ultrasounds specifically done during later period of gestation. In our case, the ultrasonography was done at 19 weeks of gestation and did not reveal either hydrocephalus or heterotopias.
Conclusion
The co-existence of aqueductal stenosis with periventricular heterotopias is rare, though few cases showing association between heterotopias and hydrocephalus have been reported in literature. In our case a two-year-old girl presented with developmental delay and was detected to have both the abnormalities on neuroimaging. In our report, we want to emphasize the importance of increased awareness amongst clinicians of this rare association so that further imaging can be done early in gestation once hydrocephalus is seen in antenatal anomaly scans. Further, we want to highlight the significance of more stringent imaging follow up after 20 weeks gestation, if future siblings are being planned in such families.
[1]. Garton HJ, Piatt JH Jr, HydrocephalusPaediatr Clin North Am 2004 51(2):305-25.10.1016/j.pcl.2003.12.00215062673 [Google Scholar] [CrossRef] [PubMed]
[2]. Kahle KT, Kulkarni AV, Limbrick DD Jr, Warf BC, "Hydrocephalus in children."Lancet 2016 387(10020):788-99.10.1016/S0140-6736(15)60694-8 [Google Scholar] [CrossRef]
[3]. Venkataramana NK, Hydrocephalus Indian scenario-A reviewJ Paediatr Neurosci 2011 6(Suppl 1):S11-S22.10.4103/1817-1745.8570422069421 [Google Scholar] [CrossRef] [PubMed]
[4]. Ucar M, Guryildirim M, Tokgoz N, Evaluation of aqueductal patency in patients with hydrocephalus: three-dimensional high-sampling-efficiency technique (space) versus two-dimensional turbo spin echo at 3 teslaKorean J Radiol 2014 15(6):827-35.10.3348/kjr.2014.15.6.82725469096 [Google Scholar] [CrossRef] [PubMed]
[5]. Barkovich AJ, Gressens P, Evrard P, Formation, maturation, and disorders of brain neocortexAJNR Am J Neuroradiol 1992 13(2):423-46. [Google Scholar]
[6]. Donkol RH, Moghazy KM, Abolenin A, Assessment of gray matter heterotopia by magnetic resonance imagingWorld J Radiol 2012 4(3):90-96.10.4329/wjr.v4.i3.9022468189 [Google Scholar] [CrossRef] [PubMed]
[7]. Zisch R, Artmann W, MR in the diagnosis of heterotopicgrey matterNeuroradiology 1991 33:527-28.10.1007/BF005880471780057 [Google Scholar] [CrossRef] [PubMed]
[8]. Umeoka S, Koyama T, Miki Y, Akai M, Tsutsui K, Togashi K, Pictorial review of tuberous sclerosis in various organsRadiographics 2008 28(7):e3210.1148/rg.e3218772274 [Google Scholar] [CrossRef] [PubMed]
[9]. Pepe E, Petricig P, Peretta P, Cinalli G, Bilateral Macrostomia Associated With Aqueductal Stenosis and Glial HeterotopiasCleft Palate–Craniofacial Journal 2007 44(5):558-61.10.1597/06-096.117760484 [Google Scholar] [CrossRef] [PubMed]
[10]. Sheen VL, Basel-Vanagaite L, Goodman JR, Etiological heterogeneity of familial periventricular heterotopias and hydrocephalusBrain & Development 2004 26(5):326-34.10.1016/j.braindev.2003.09.00415165674 [Google Scholar] [CrossRef] [PubMed]
[11]. Manganaro L, Saldari M, Bernardo S, Aliberti C, Silvestri E, Bilateral subependymal heterotopia, ventriculomegaly and cerebellar asymmetry: Fetal MRI findings of a rare association of brain anomaliesJournal of Radiology Case Reports 2013 7(11):38-45.10.3941/jrcr.v7i11.145724421929 [Google Scholar] [CrossRef] [PubMed]
[12]. Bargallo N, Puerto B, De Juan C, Martinez-Crespo JM, Lourdes Olondo M, Hereditary subependymal heterotopia associated with mega cisterna magna: antenatal diagnosis with magnetic resonance imagingUltrasound Obstet Gynecol 2002 20(1):86-89.10.1046/j.1469-0705.2002.00741.x12100426 [Google Scholar] [CrossRef] [PubMed]
[13]. Srour M, Rioux MF, Varga C, Lortie A, Major P, Robitaille Y, The clinical spectrum of nodular heterotopias in children: Report of 31 patientsEpilepsia 2011 52(4):728-37.10.1111/j.1528-1167.2010.02975.x21320118 [Google Scholar] [CrossRef] [PubMed]