Dizziness: Smell the Smoke!
Sharwari Bhutada1, Santosh Venketraman Kondekar2, Surbhi Rathi3, Rajesh Kunchelikar4, Tejaswini Munde5
1 Paediatric Medical Officer, Department of Paediatrics, Topiwala National Medical College, Mumbai, Maharashtra, India.
2 Associate Professor, Department of Paediatrics, Topiwala National Medical College, Mumbai, Maharashtra, India.
3 Professor, Department of Paediatrics, Topiwala National Medical College, Mumbai, Maharashtra, India.
4 Resident, Department of Paediatrics, Topiwala National Medical College, Mumbai, Maharashtra, India.
5 Resident, Department of Paediatrics, Topiwala National Medical College, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Santosh Venketraman Kondekar, Associate Professor, Department of Paediatrics, College Building First Floor, BYL Nair Hospital, Mumbai Central, Mumbai-400008, Maharashtra, India.
E-mail: drkondekar@gmail.com
Dizziness in a child is often mistaken for giddiness, vertigo or syncope and at times it is considered equivalent to malingering or foolishness. We hereby report a case of a child whose dizziness stayed neglected and unevaluated for three years. This case is an eye opener for physicians to not take the symptom lightly. A detailed assessment and prompt evaluation can seriously unmask the underlying morbidity like Moyamoya Disease (MMD).
Giddiness, Moyamoya disease, Puff of smoke, Stroke, Vertigo
Case Report
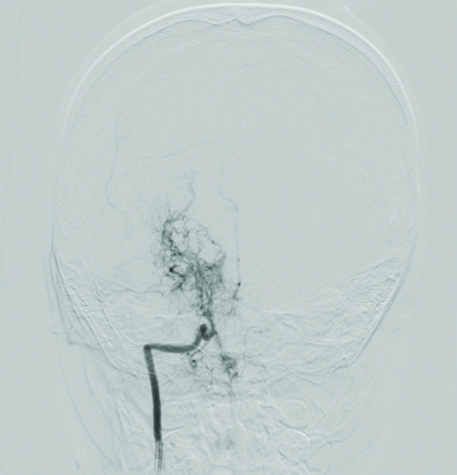
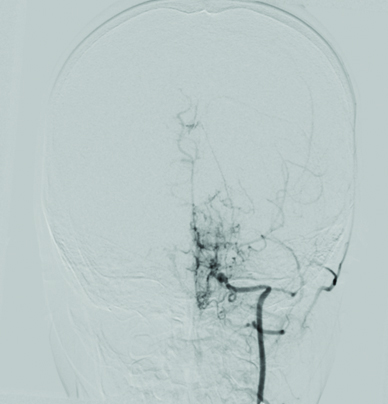
A 6-year-old left handed girl born out of a non consanguineous marriage from an educated family was brought with complaints of six episodes dizziness in last three years. Each time, child used to complain about some different feeling lasting few minutes and then she used to be near normal. This feeling was described by the parents as dizziness or giddiness at times and no evaluation was made. These episodes were not related to school, study, stress, exertion or position and only once she had to skip school for same. During these episodes she was fully conscious and obeying commands and performing day to day activities but preferred to lie down. In her last episode, a prompt reference to otologist was made in view of vertigo and was started on Cinnarizine 1 mg/kg body weight once a day for a week. In the current episode her dizziness was associated with mild headache, to confuse as migraine. She had normal milestones and had no family history for similar events or seizures. No history of any convulsion, fever, vomiting, involuntary movement, trauma or fall. Patient has a past history of febrile convulsion at two years of age. On examination, child had normal blood pressure and other vital parameters. On central nervous system examination, cranial nerves and fundus were normal except that her speech sounded monotonous and slurred. Further, on neurological examination, her right hand grip was noted weak and she could not raise her right hand above her head. Power was 2/5 at shoulder extension. Rest of the power, tone, reflexes and systemic examination was normal. Blood counts, blood glucose and electrolytes were normal. Suspecting an old infarct involving left prefrontal cortex, a CT brain was advised. CT brain plain showed bilateral patchy infarcts across Middle Cerebral Artery (MCA) territory. Digital Subtraction Angiography (DSA), confirmed narrowing at roots of internal carotid artery and its branches along with multiple collaterals bilaterally across the cerebral circulation, sparing the ophthalmic artery resembling a “puff of smoke” appearance [Table/Fig-1,2]. This confirmed the diagnosis of MMD. She recovered from the dizzy episode over two days, but grip deficit and speech slurring persisted for a month. She was started on aspirin 75 mg/kg body weight per day for six weeks and neurosurgeons have planned a corrective shunt.
Digital subtraction angiography right internal carotid artery anteroposterior view, showing puff of smoke appearance;
Digital subtraction angiography left internal carotid artery anteroposterior view showing puff of smoke appearance.
Discussion
Dizziness, giddiness and syncope are often used interchangeably. Dizziness is commonly associated with vertigo, hypoglycaemia, hypotension and labyrinthitis [1]. Stroke and disorders of cerebrovascular system are a known cause of dizziness [2]. These conditions are often overlooked being rare and easily misinterpretable by parent, child or doctor. Also, as children often verbally mimic non-specific symptom of a parent; and also as toddlers have less understanding for a particular subjective symptoms; it does get wrongly described. Unless associated with other symptom or sign, a detailed evaluation is usually not planned unless the symptoms recur.
Strokes in children often present with frank deficits of power or cranial nerves than as dizziness alone [2]. Dizziness/giddiness is a common symptom associated with cerebrovascular accidents, transient ischaemic attacks in adult. This is another reason that a cerebrovascular accident is not easily suspected in a child who has no obvious restriction of activity or deficit in power.
Moyamoya disease is known for asymptomatic multiple non-catastrophic strokes with or without seizures in different time span, primarily due to simultaneous development of collateral circulation of capillaries over years [3]. There has been no case reported of MMD presenting as persistent/recurrent dizziness. Intermittent hemiplegia is a more common presentation of MMD [4]. Transient Ischaemic Attacks (TIA) is another known presentation of MMD [5].
Moyamoya, which means “wavering puff of smoke”, reflects to the image of collateral capillary communications as seen on DSA. Its incidence ranges between 0.54 per 100,000 patients globally [6,7]. It forms about one-fifth of the known cerebral arteriopathies in paediatric stroke up to most common cerebrovascular disease in children in East Asia [8].
In children, unilateral involvement occurs about 18% and progress to bilateral involvement within two years [9,10]. Aetiology of the disease is still not known but genetic causes are highly considered. Paediatric age group commonly presents as TIA, strokes along with headache, involuntary choreiform movements, seizures and other motor disturbances [11]. Rarely, a child presents with repeated episodes of dizziness/giddiness and altered speech as in our case. It is difficult to diagnose early in younger children (TIA versus infarction) [12].
Early diagnosis and treatment is necessary during childhood as the disease can lead to progressive deterioration in cognition and disability [13]. Currently, there is no definitive medical treatment to treat or stabilise the course. Direct Superficial Temporal Artery (STA) to MCA bypass is the surgical treatment of choice. Indirect surgeries such as Encephalo-Duroarterio-Synangiosis (EDAS) and Encephalo-Myo-Synangiosis (EMS) appear promising.
Conclusion
Dizziness as a symptom carries vague meaning. Even though it is a non-specific symptom, it is a remote presenting sign for serious conditions. A careful examination and prompt investigation helped unmask the underlying cerebrovascular disease. It’s important to keep the high-index of suspicion about a Cerebrovascular Accident (CVA) (puff of smoke–“Moyamoya”) in a child complaining of non-specific symptoms (smell of the smoke).
[1]. Wipperman J, Dizziness and vertigoPrim Care 2014 41(1):115-31.10.1016/j.pop.2013.10.00424439886 [Google Scholar] [CrossRef] [PubMed]
[2]. Amlie-Lefond C, Bernard TJ, Sébire G, Friedman NR, Heyer GL, Lerner NB, Predictors of cerebral arteriopathies in children with arterial ischemic stroke: Results of the international pediatric stroke studyCirculation 2009 119(10):1417-23.10.1161/CIRCULATIONAHA.108.80630719255344 [Google Scholar] [CrossRef] [PubMed]
[3]. Suzuki J, Kodama N, Moyamoya disease–a reviewStroke 1983 14(1):104-09.10.1161/01.STR.14.1.1046823678 [Google Scholar] [CrossRef] [PubMed]
[4]. Bidaki R, Zarepur E, Intermittent hemiplegia in a boy with primary moyamoya disease: A case report from IranIranian J Chil Neurol 2017 11(2):65 [Google Scholar]
[5]. Zhao M, Zhang D, Wang S, Zhang Y, Wang R, Zhao J, Transient ischemic attack in pediatric patients with moyamoya disease: Clinical features, natural history, and predictors of strokePediatric Neurology 2017 75:48-54.10.1016/j.pediatrneurol.2017.06.02028778481 [Google Scholar] [CrossRef] [PubMed]
[6]. Kim SK, Wang KC, Kim DG, Paek SH, Chung HT, Han MH, Clinical feature and outcome of pediatric cerebrovascular disease: a neurosurgical seriesChilds Nerv Syst 2000 16:421-28.10.1007/PL0000728610958551 [Google Scholar] [CrossRef] [PubMed]
[7]. Uchino K, Johnston SC, Becker KJ, Tirschwell DL, Moyamoya disease in Washington state and CaliforniaNeurology 2005 65(6):956-58.10.1212/01.wnl.0000176066.33797.8216186547 [Google Scholar] [CrossRef] [PubMed]
[8]. Kuriyama S, Kusaka Y, Fujimura M, Wakai K, Tamakoshi A, Hashimoto S, Prevalence and clinic-epidemiological features of moyamoya disease in Japan: Findings from a nationwide epidemiological surveyStroke 2008 39(1):42-47.10.1161/STROKEAHA.107.49071418048855 [Google Scholar] [CrossRef] [PubMed]
[9]. Kelly ME, Bell-Stephens TE, Marks MP, Do HM, Steinberg GK, Progression of unilateral moyamoya disease: A clinical seriesCerebrovasc Dis 2006 22(2-3):109-15.10.1159/00009323816685122 [Google Scholar] [CrossRef] [PubMed]
[10]. Kawano T, Fukui M, Hashimoto N, Yonekawa Y, Follow-up study of patients with unilateral Moyamoya diseaseNeurol Med Chir (Tokyo) 1994 34(11):744-47.10.2176/nmc.34.7447533268 [Google Scholar] [CrossRef] [PubMed]
[11]. Gosalakkal JA, Moyamoya disease: A reviewNeurology India 2002 50(1):6-10. [Google Scholar]
[12]. Jea A, Smith ER, Robertson R, Scott RM, Moyamoya syndrome associated with down syndrome outcome after surgical revascularizationPediatrics 2005 116(5):e694-701.10.1542/peds.2005-056816263984 [Google Scholar] [CrossRef] [PubMed]
[13]. Khan N, Schuknecht B, Boltshauser E, Capone A, Buck A, Imhof HG, Moyamoya disease and moyamoya syndrome: Experience in Europe; choice of revascularisation proceduresActa Neurochir (Wien) 2003 145(12):1061-71.10.1007/s00701-003-0148-514663563 [Google Scholar] [CrossRef] [PubMed]