Breastmilk is the most complete and ideal food for infants and all efforts should be made to promote successful breastfeeding. Insufficient mother’s milk intake can lead to increased incidence of neonatal jaundice, inadequate weight gain, hypernatraemic dehydration and occasionally causes serious ill-effects on neonate’s health. Hypernatraemic dehydration secondary to faulty breastfeeding practices is a completely preventable complication and its rising trend emphasizes the importance of intense counselling of lactating mothers to reduce the incidence. Increasing awareness in health personnel will go a long way in reducing this preventable complication of inadequate breastfeeding to newborns.
Poor mother’s milk intake/inadequate feeding is one of the frequent cause of exaggerated physiological jaundice, some of these neonates may have weight loss and hypernatraemia in addition to hyperbilirubinaemia [1,2]. Reduced feeding or lactation failure could be due to maternal or neonatal factors. These include mothers with postpartum stress, mastitis, engorged breasts, sore or retracted nipple and tend to cause impaired lactogenesis. Similarly, neonates can have poor suckling as a result of prematurity, hypoglycaemia, infection, facial anomalies, maternal drugs etc. These causes often lead to reduced intake of breast milk by the babies and ultimately may lead to dehydration. High-levels of sodium in mother’s milk can be indicative of lactation failure and neonates of such mothers are at risk of the above complications [3]. The aim of our study was to know what proportion of neonates admitted with unconjugated non-haemolytic hyperbilirubinaemia exhibit inadequate weight gain and/or hypernatraemia, to study association between serum sodium and mother’s milk sodium levels and also to study the feeding patterns or feeding issues in them.
Materials and Methods
This research was conducted as a prospective observational study over a period of one year (June 2014 to May 2015) at Neonatal Intensive Care Unit (NICU)/Postnatal Care (PNC) ward of our tertiary care hospital. Before commencing the study, we had taken the Institutional Ethics Committee’s approval. An informed written consent was taken from every mother whose neonate fulfilled the inclusion criteria.
Inclusion and Exclusion Criteria
We enrolled 60 full term neonates who had >2500 gm birth weight, >48 hours old, admitted for indirect hyperbilirubinaemia with bilirubin levels more than 12 mg/dL (above physiological range and requiring phototherapy as per NICE guidelines) [4,5]. Any baby with hemolysis as a cause of jaundice [suggested by reticulocyte count > normal range (depending on day of life)], prolonged jaundice or with conjugated jaundice was excluded from the study. Babies who were severely ill or who had received special medical treatment prior to hyperbilirubinaemia presentation/had any known predisposing medical condition (sepsis/haematoma/polycythaemia/NICU admission for any other reason) for hyperbilirubinaemia were also excluded.
Sample Size
Calculation of sample size was based on Medcalc V.11.3.3.0 software, by taking a similar study done by Tarcan A et al., as a reference study and the minimum sample size in this study was determined as 46 (r-0.4, p-0.05) [2]. However, to adjust for any dropouts, we took a sample size of 60. [Total sample size=N=[(Zα+Zβ)/C]2+3=46. Where, The standard normal deviate for α =Zα=1.960, The standard normal deviate for β=Zβ=0.842, C=0.5* ln[(1+r)/(1-r)] = 0.424].
Study Procedure
A thorough clinical evaluation of all the neonates was done by the authors independently with a detailed history related to jaundice, birth details, weight at admission and birth, significant prenatal/postnatal issues, feeding problems and a complete physical examination. Subsequently daily weight, hydration status, frequency of urine output and jaundice were noted in prestructured proforma. Weight check was done for naked neonates using a digital scale with an error of 5 gm. Maternal breast examination was also done to assess feeding related issues in the mother, for example, mothers with cracked nipple/flat nipple/mastitis/engorged breast/low milk output etc. Besides this, to evaluate for correct breastfeeding techniques with respect to position/latch/infant suck, infant-mother dyads were observed.
Serum Bilirubin levels (total and direct) were estimated for all these neonates at admission, the levels were repeated after eight to tweleve hours depending upon neonate’s response to phototherapy. Blood investigations were also done at admission to rule out common causes of indirect hyperbilirubinaemia i.e., blood cell counts, haemoglobin, blood grouping, reticulocyte index, Direct Coomb’s Test (DCT), Glucose-6-Phosphate Dehydrogenase (G6PD), blood culture, serum electrolytes, Blood Urea Nitrogen (BUN) and creatinine. These also helped to exclude babies with haemolytic causes, sepsis, prolonged jaundice or babies predisposed with any known risk factor [5]. In addition, the mother’s breast milk sodium levels were assessed. The babies were monitored till clinical and biochemical improvement. Serum sodium levels were repeated after six to eight hours in patients with hypernatraemia and later if required. These neonates were then categorised into three groups: a) Group A-Neonates with <10% weight loss or regained birth weight by day 10 (39 neonates) b) Group B-Neonates with >10% weight loss or did not regain birth weight by day 10 and serum sodium <146 mEq/L (14 neonates) and c) Group C-Neonates with >10% weight loss or did not regain birth weight by day 10 and serum sodium ≥146 mEq/L (seven neonates).
Definitions
Inadequate weight gain was defined in babies who had >10% weight loss or had not regained birth weight by tenth postnatal day or did not gain 15-20 gm/day after the 10th day of life [6-8]. Hypernatraemia was defined as serum Na levels ≥ 146 mEq/L. Mother’s breast milk sodium levels of >20 mEq/L after 3rd day of postpartum period, were considered to be higher than normal [2,3].
Statistical Analysis
All data was analysed using SPSS package, version 11.5. Quantitated data was calculated with the help of mean, standard deviation, and median. Categorical data was analysed using Pearson’s chi-square test. A p-value <0.05 was considered statistically significant. Scatter plots were made to assess the relation between percentage weight loss and day of life, weight loss and mother’s milk sodium levels and to look for mother’s milk sodium levels in relation to their baby’s serum sodium levels. Pearson correlation coefficient was used to analyse correlation between these quantifiable parameters e.g., serum sodium and breast milk sodium.
Results
Our demographic data of 60 enrolled babies, revealed male predominance (37) (61.6%) and majority 46 (76.6%) of the neonates weighed between 2500 to 3000 gm. As many as, 55 neonates (91.6%) presented to us between third to seventh day of life with hyperbilirubinaemia [Table/Fig-1]. There were 39 hyperbilirubinaemic babies with weight loss less than 10% (Group A) and 21(33%) neonates had significant weight loss of >10%. Of these 21 neonates, 14 (66.6%) had normal serum sodium (Group B) and seven (33.3%) had hypernatraemia (Na≥146 meq/L) (Group C). The correlation between weight loss and hypernatraemia was found to be highly significant (p-value: 0.004). Of the total nine (15%) neonates with hypernatraemia, seven had weight loss >10% (Group C) and two neonates did not have any significant weight loss (Group A). One neonate had severe hypernatraemia (Na >150 mEq/L) and eight had values between 146-149 mEq/L. Incidence of combined weight loss and hypernatraemia (Group C) among all studied hyperbilirubinaemic neonates was 12%. We did not find any direct correlation between the bilirubin level and weight loss or serum sodium concentration.
Comparison of clinical and biochemical parameters in three groups of neonates.
| Healthy Term Neonates (n=60) | Group-A (n=39)Weight loss <10% | Group-B (n=14)Weight loss >10% | Group C (n=7)Weight loss >10% with Serum Na >146 mEq/L |
|---|
| Birth weight (gm) | 2929±3972845 (2500–4100) | 2777±2362693 (2521–3346) | 2711±1612635 (2500–2960) |
| Postnatal age at presentation (days) | 4.4±2.33.75 (2–15) | 3.6±0.63.5 (2.9-5.2) | 3.5±2.23 (2.5–14) |
| Weight at admission (gm) | 2742±3602742 (2310–3780) | 2468±2342400 (2200–2940) | 2363±1372345 (2200–2500) |
| % Weight loss at admission | 6.1±2.26.3 (1–10) | 10.9±3.411.1 (10.1–15.3) | 12.7±2.212.4 (10.3–16) |
| Mode of feeding (breast milk/cow’s/mixed feeding) | 33/2/4 | 13/0/1 | 4/1/2 |
| Indirect bilirubin (mg/dL) | 18.7±1.018.8 (15.1–22) | 18.7±0.618.8 (17.5–19.8) | 18.5±0.618.2 (18–19.8) |
| Serum Na (mEq/L) | 139±3.1139 (135–147) | 140±2.9139 (134-144) | 148±1.9149 (146–151) |
| Breast milk Na (mEq/L) | 17.4±9.413 (6–49) | 14.1±8.911 (2–38) | 28.8±2216 (7–59) |
Values are given as mean±standard deviation median (minimum-maximum). Na-sodium ions
We found 18 (30%) mothers to have high sodium levels in their milk and amongst these mother-infant dyads, 16% of the neonates had significant weight loss as well as serum hypernatraemia. While amongst mothers with normal milk sodium levels, 7% of babies had significant weight loss and hypernatraemia [Table/Fig-2]. This association between weight loss, hypernatraemia and mother’s milk sodium levels was also found to be statistically significant (p-value: 0.017). Neonates exhibiting >10% weight loss had no statistical difference related to the parity of the mother (30% were primiparous and 43% of multiparous mothers).
Association between weight loss/hypernatraemia and breast milk sodium levels.
| Breast milk sodium | % Weight loss | Serum sodium | Total |
|---|
| Normal | Hypernatraemia |
|---|
| Normal (42) | Up to 10% | 25 (59.5%) | 01(2.3%) | 26 (62%) |
| Above 10% | 12 (28.5%) | 04 (9.5%) | 16 (38%) |
| Total | 37 (88.1%) | 05 (11.9%) | 42 (100%) |
| Pearson chi-square | Value-4.226 | Df-1 | p-value=0.040 |
| High (18) | Up to 10% | 12 (66.6%) | 01 (5.5%) | 13 (72%) |
| Above 10% | 02 (11.1%) | 03 (16.6%) | 05 (28%) |
| Total | 14 (77.8%) | 04 (22.2%) | 18 (100%) |
| Pearson chi-square | Value (5.716) | Df-1 | p-value=0.017 |
Feeding pattern in our neonates revealed that as many as 50 (83%) neonates were on exclusive breastfeeding and 17% (10) were either mixed fed or were fed with cow’s milk. No significant correlation between weight loss, hypernatraemia and mode of feeding was detected. We found 39 (65%) mothers to have feeding issues, like 29 (48%) had complained of perceived low milk output, six (10%) mothers were giving foremilk only, four (6.6%) mothers had nipple related issues like cracked nipple/flat nipple leading to inadequate mother’s milk intake by their neonates. Amongst the mothers with feeding issues, 77% had high levels of sodium in their milk. Also our analysis revealed that all the hypernatraemic babies belonged to mothers with breastfeeding related issues.
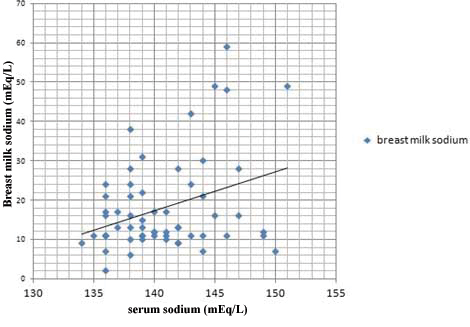
On statistical analysis, the scatter plot [Table/Fig-3] depicts a positive correlation, between neonate’s serum sodium levels and mother’s milk sodium levels. The value of R was 0.6329 and R2, the coefficient of determination, was 0.4006.
The scatter diagram shows a positive correlation, between neonate’s serum sodium levels and mother’s milk sodium levels.
Discussion
Inadequate breastfeeding in the first week of life is one of the major factors responsible for exaggeration of physiologic jaundice and leads to development of breastfeeding jaundice. Some of these babies besides presenting with jaundice clinically may have exaggerated weight loss and hypernatraemia also.
In our study, nearly 61% neonates were males and 92% neonates presented within first week of life. Most presentations of jaundice being in first week is reported by many other authors [2,9]. It is known that less caloric/fluid intake in the first few days of life delays intestinal movements and increases enterohepatic circulation, finally leading to increased levels of indirect bilirubin in the blood. Poor feeding has a major role in hospital readmissions also for healthy term icteric infants. Thus, early establishment of adequate lactation is essential in preventing hospitalisation of such infants in the first few days of life.
In the present study, 33% of hyperbilirubinaemic newborns exhibited severe weight loss (>10%). Boskabadi H et al., showed about one-third of neonates with idiopathic hyperbilirubinaemia had weight loss of more than 7%. Another study by Tarcan A et al., also indicates the similar prevalence [1,2]. Such high incidence of potential complications of inadequate breastfeeding is posing a greater demand on the current physicians to educate mothers for proper breastfeeding techniques. Recent policy statement from American Academy of Paediatrics insists that weight loss of more than 7% from birth weight during the first five days of life indicate possible breastfeeding problems and require urgent evaluation [10].
A significant correlation between weight loss and hypernatraemia was observed, of the nine neonates with hypernatraemia (Na >146 mEq/L), seven (11.6%) had severe weight loss of >10% in addition (p=0.004). Several other studies have reported a linear and direct relation between high serum sodium and weight loss in neonates [11,2]. Oddie SJ et al., in his population based study reported a significant association between serum sodium levels and percentage weight loss at presentation, with sodium as a dependent variable and a greater weight loss linked to higher sodium levels in term neonates [12].
The combined incidence of weight loss and hypernatraemia (Group C) among all studied hyperbilirubinaemic neonates was 12% in our study. In a study by Basiratina M et al., the prevalence of ‘Breastfeeding Associated Hypernatraemia (BFAH)’ among hospitalised hyperbilirubinaemic neonates was 7.4% which was similar to the results of other studies also [13,14]. These observations support early measurement of sodium levels in neonates presenting with jaundice and significant weight loss, as neonates with hypernatraemic dehydration are known to have better conservation of extravascular volume, thus being less symptomatic during the initial phase.
In our study, there was no direct correlation between the bilirubin level and either weight loss or peak serum sodium concentration. This was also observed by several other authors [15,16]. However, on the contrary, Boskabadi H et al., reported that neonates with idiopathic severe hyperbilirubinaemia had three times more severe weight loss when compared with those of weight loss <7% [1]. This could be due to causal relationship of jaundice and hypernatraemic dehydration with poor feeding, both the complications despite being independent variables tend to present together in babies receiving lesser calories and hydration.
The relationship between weight loss and parity of mother is not very clear. Various studies done previously on association of these parameters, have shown that hypernatraemic infants were significantly more likely to be born to primiparous mothers than those born to multiparous [17,18]. In contrast, in our study, the weight loss pattern in babies was similar in multiparous or primiparous mothers and there was no statistical association of weight loss with parity (43% vs. 30% respectively), perhaps because of small sample size of our study population. Basiratnia M et al., have also shown no difference in the rate of significant weight loss with parity of mother [13]. Nevertheless, lack of education and irregular clinical follow ups have remained the major causes for such inadequate feeding practices since long time. It is highly recommended that early postpartum follow up of all mother infant dyads should be done and the education on breastfeeding for all seems to be extremely important irrespective of the parity of the mothers.
On studying the feeding patterns in our neonates, we noted that majority of neonates were given exclusive breastfeeding and about 17% were either mixed fed or were on cow’s milk. We found no correlation between weight loss, hypernatraemia and mode of feeding. In a study by Zuppa AA et al., 903 healthy term neonates were investigated in two feeding models of partial and full rooming-in and no statistical difference was observed on the incidence of weight loss or jaundice with respect to mode of feeding [15]. Similar results were also noted by few other authors in their study [2,16]. Whereas, Basiratina M et al., and Chen CF et al., noted more significant weight loss being associated with breastfed neonates when compared with mixed feeding [13,19]. This was in contrast to the study done by Davanzo R et al., who found that in infants, the weight loss in the formula fed group was higher than in the breastfed group (7.5% vs 6.3%). According to their study, formula feeding was a probable risk factor for greater early neonatal weight loss [6]. To evaluate the true impact of mixed or formula feeding on the neonatal health, further research is warranted.
Early breastfeeding problems that a mother encounters ranges from lack in confidence in her breastfeeding abilities, lack of support from family members, previous unpleasant breastfeeding experiences and breast and nipple problems. In our study, 29 (48%) out of 60 mothers, had complained of perceived low milk output, six (10%) mothers were giving foremilk only, four (6.6%) mothers had nipple related issues like cracked nipple/ flat nipple. In a study by Boskabadi H et al., almost half of mothers of neonates with hypernatraemic dehydration had positioning/latching difficulties, inverted nipple (17%), cracked nipple (17%) or mastitis (9%) [18]. In Jain S and Basu S report, nearly 62% mothers had complaints of inadequate lactation due to perceived low milk output or breast problems [20]. There is no alternative solution to combat such high incidence of distress among these mothers other than educating and counselling them.
Studies suggests that high breast milk sodium level is often documented in mothers of neonates with weight loss and hypernatraemia. Poor milk drainage from the breast potentiates high sodium content in mother’s milk [21]. Research also indicates that high levels of sodium in breast milk are closely associated with lactation failure [22]. Our data was consistent with that of other investigators who have noted a significantly higher incidence of weight loss in neonates with mother’s milk hypernatraemia as compared to those with normal mother’s milk sodium [23,24].
Limitation
The small sample size of our study limits the ability in assessing the true burden of inadequate feeding related complications in newborns and makes it difficult to generalise the results to a larger population. Another limitation was that accurate estimation of mother’s milk intake and evaluation of pregnancy and childbirth related problems were not documented.
Conclusion
Our study reveals that due to inadequate breastfeeding, some neonates may have weight loss and hypernatraemia in addition to presenting with hyperbilirubinaemia. High mother’s milk sodium levels indicated a high possibility of lactation failure in them. Occurrence of significant weight loss, hypernatraemia and hyperbilirubinaemia in neonates due to inadequate breastfeeding suggests the widespread need for better physician/nursing/parents training in breastfeeding management, adequate follow up monitoring and breastfeeding education.
Values are given as mean±standard deviation median (minimum-maximum). Na-sodium ions