Histopathological Changes in Skin after Electric Current Injury: An Autopsy Study
Didar Singh Walia1, Raminder Kaur2, Jagdish Gargi3, Daljit Singh4, Akash Deep Aggarwal5
1 Assistant Professor, Department of Forensic Medicine, Government Medical College, Patiala, Punjab, India.
2 Senior Resident, Department of Otorhinolaryngology, Government Medical College, Patiala, Punjab, India.
3 Ex-Professor and Head, Department of Forensic Medicine, Government Medical College, Amritsar, Punjab, India.
4 Ex-Professor and Head, Department of Clinical Pathology, Government Medical College, Amritsar, Punjab, India.
5 Associate Professor, Department of Forensic Medicine, Government Medical College, Patiala, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Akash Deep Aggarwal, 14-Desi Mehmandari, Patiala-147001, Punjab, India.
E-mail: toakashdeep@gmail.com
Introduction
With the proliferation of electrical equipment and devices, there is a rise in deaths due to electrocution injuries. There may be allegations of electric burns either by way of accident or torture. Many a times no specific findings may be present to support such a claim. Electric contact mark is pathognomic of electrocution.
Aim
To decide whether the electric current mark was antemortem or postmortem in nature or no conclusion regarding the same can be drawn even after histopathological examination.
Materials and Methods
The present study was conducted on 40 dead bodies brought to the mortuary of a Tertiary Care Institution, Government Medical College, Amritsar, Punjab, India, with history of death due to electric shock over a period of two years. Another 20 corpses, who had not died due to electric current injury, but were given the same after death, were taken as control. All the 40 cases were thoroughly examined for medicolegal purposes at the time of conducting postmortem examination and findings were recorded as per proforma attached. Skin was examined for the wound of entry and exit (if any) of electric current injury. Skin biopsies, from the electric current sites of the deceased, were taken from the edge of the wound and subjected to histopathological examination.
Results
About 85% cases had visible electric current injury. Involvement of clothes was seen in 15% cases. Microscopic findings included bulla (22.5%), flattened papillae (47.5%), erosions (12.5%), charring (45%), nuclear changes (2.5%), vacuolisation (12.5%) and necrosis (62.5%). In the 20 control cases studied, charring of the skin was present in the epidermis/dermis and no other change was observed.
Conclusion
Histopathological changes can be used as supportive evidence in giving cause of death in such cases.
Blister, Burns, Dermis, Electrocution, Epidermis, Histopathology
Introduction
Deaths due to electrocution are not too uncommon in comparison with the widespread use of electricity. The skin is a relatively thin layer of tissue but highly resistant to the passage of electric current; resistance is not homogeneous, and at certain points insulation is poor. The occurrence of injuries caused by contact with electrical conductors depends upon kind of current, amount of current, path of current and duration of current [1,2]. In electric current injury, external lesions include contact burns, spark burns or flash burns. The internal appearance of lesions is those of anoxia [3]. Ecchymosis, lacerations and contusions may be present at the point of entry and exit of the current; and the hair may be singed [4].
The end result of passage of an electric current through the human body is unpredictable in individual case; many factors are known to influence the nature and severity of electrical injuries. Body tissues vary considerably in their resistance to flow of current, with conductivity roughly proportional to water content. Bone and skin offer relatively high resistance while blood, muscle and nerve are good conductors. The resistance of normal skin can be lowered by moisture which can convert a mild injury to a fatal shock. Grounding can lower the intensity of current passing through the body. The accident involving passage of current between a point of contact on the leg and the ground is less likely to be injurious than one between the head and the foot, in which heart lies between the two poles of circuit [5].
Since electrical injuries may leave minimal or no visible scars, there is a need for the study of histopathological changes, useful to support the allegations of electrical torture [6]. Calcification at the site of electric current injury has also been reported, though its origins are debatable [7]. Although, the current mark is a proof that electric current passed through the body, only the detection of vital reaction will decide whether the exposure to the electric current occurred before or after death [8].
The electric current injuries are fairly resistant to postmortem decomposition and can be demonstrable for a considerable period of time on a buried corpse [9]. Deaths caused by lightning stroke are also common. The pathological changes in this form of death are essentially similar to deaths caused by contact with electrical conductors [10].
This study was undertaken to decide whether the electric current injury mark was antemortem or postmortem in nature or no conclusion regarding the same can be drawn even after histopathological examination.
Materials and Methods
The cross-sectional analytical study was conducted on 40 dead bodies brought to the mortuary of a tertiary care institution, with history of death due to electric shock over a period of two years from April 2007 to March 2009. Another 20 corpses, who had not died due to electric current injury, but were given the same after death, were taken as control. The electric current (220 V) was applied to control cases at different sites.
All the 40 cases were thoroughly examined for medicolegal purposes at the time of conducting postmortem examination and findings were recorded as per proforma attached. Skin was examined for the wound of entry and exit (if any) of electric current injury. Skin biopsies, from the electric current injury sites of the deceased, were taken from the edge of the wound and subjected to histopathological examination. Histopathological examination was carried out as described by Culling CFA et al., using haematoxylin and eosin staining [11].
Results
Over a period of two years, 1748 cases were brought to the mortuary, of which, 40 cases were brought by the police with the alleged cause of death to be electric shock. Incidence of electric shock was 2.2% of total autopsies. Male (n=37) to female (n=3) ratio was 12.5:1, with most of the victims (62.5%) aged 20-40 years. Death was reported within 30 minutes of electrocution in 92.5% of the cases [Table/Fig-1].
Electric current injury changes observed in the present study.
| Changes | Depth/change | N=40 | Percentage (%) |
|---|
| Involvement of clothes | Absent | 34 | 85.0 |
| Present | 6 | 15.0 |
| Gross changes | No visible electric current | 6 | 15.0 |
| Epidermis | 3 | 7.5 |
| Epidermis and dermis | 28 | 70.0 |
| Deeper tissues also involved | 3 | 7.5 |
| Blister formation | - | - |
| Metallisation | - | - |
| Inflammatory response | - | - |
| Microscopic changes in epidermis | Bulla formation | 9 | 22.5 |
| Papillae flattened | 19 | 47.5 |
| Epidermis charred/burnt | 18 | 45.0 |
| Vesicular nucleus | 1 | 2.5 |
| Eroded | 5 | 12.5 |
| No significant change | 3 | 7.5 |
| Microscopic changes in dermis | Necrotic changes | 25 | 62.5 |
| Charring | 3 | 7.5 |
| Bulla formation | 2 | 5.0 |
| Vacuolated appearances | 5 | 12.5 |
| Calcification/metallisation | - | - |
| Adnexal structures intact | 9 | 22.5 |
| Papillae flattened | 3 | 7.5 |
| Intact dermal glands | 2 | 5.0 |
| Inflammatory change | - | - |
| No significant change | 4 | 10 |
Epidermis and dermis were involved in 28 (70%) of the cases while blister formation, metallisation or inflammatory response of the tissues was not present in any of the cases. In 34 (85%) of the cases, clothing of the deceased was not involved. Of these 6 out of 40 cases, clothing of 5 (12.5%) persons was involved due to flash burns, while in 1 (2.5%) case clothing was involved due to lightening. Exit wound of electric current injury was not present in any of the victims of electric current injury cases in present study.
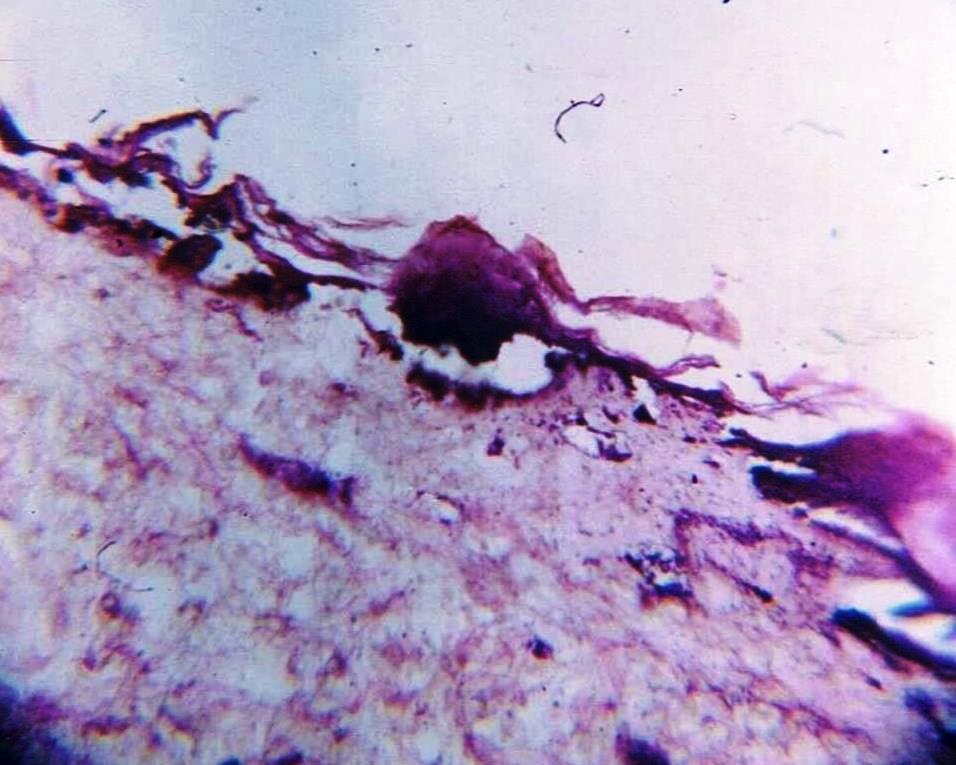
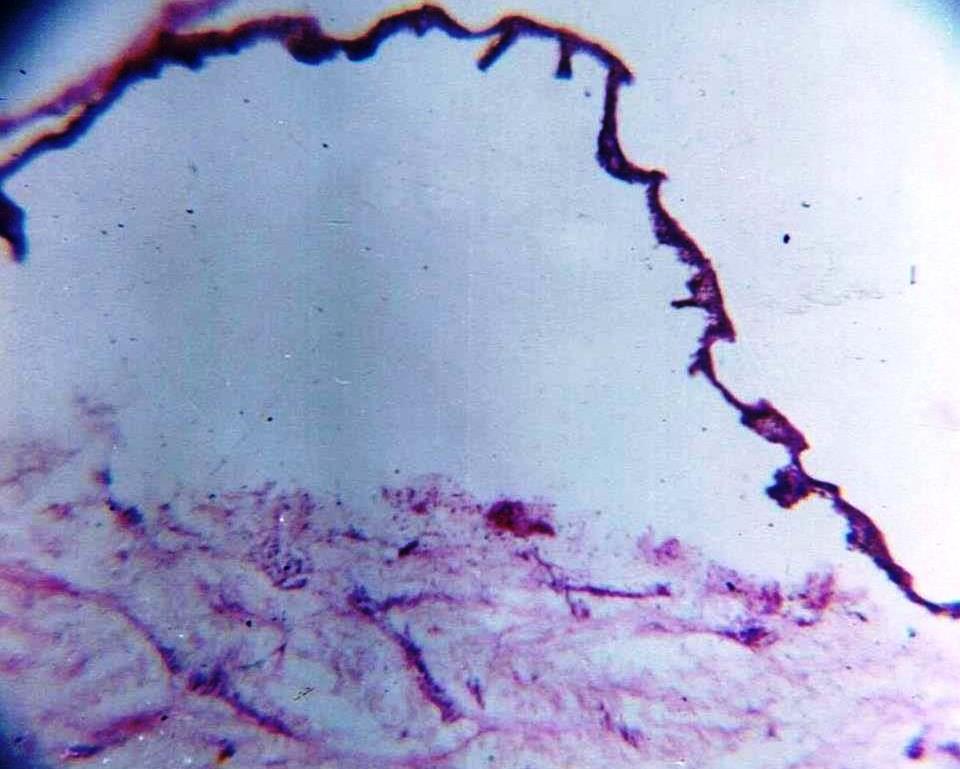
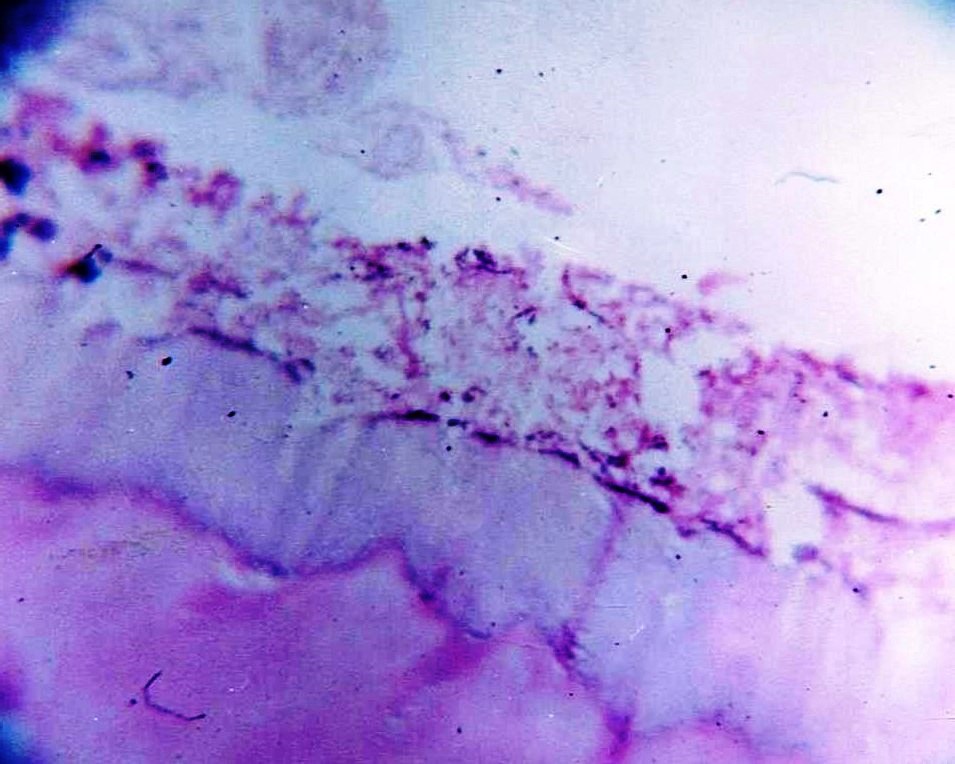
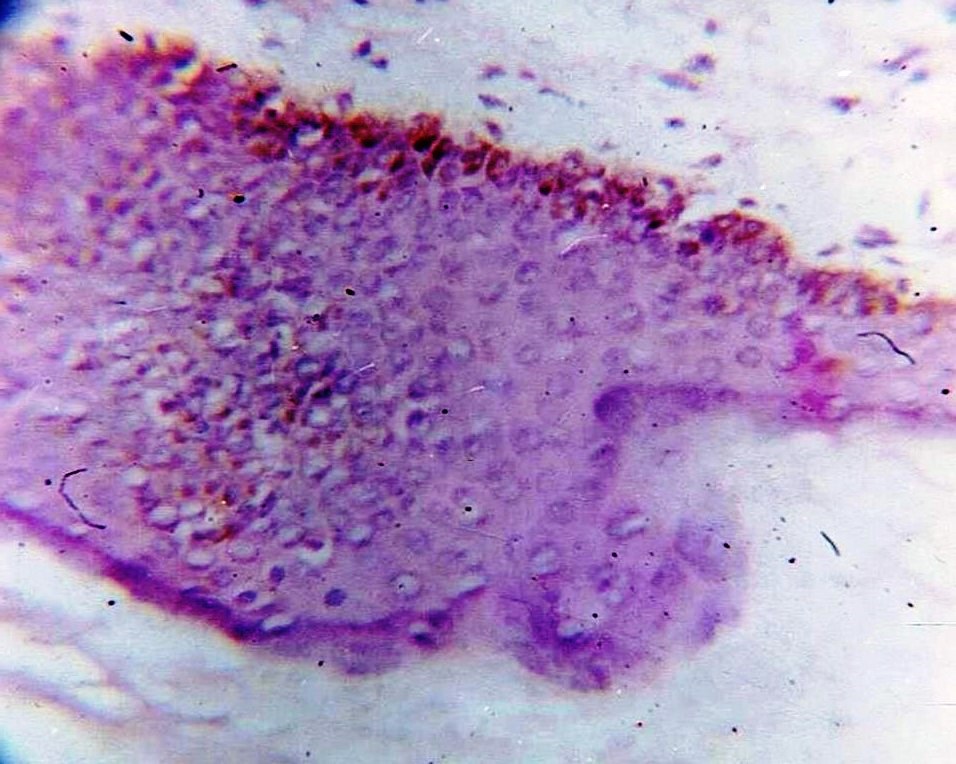
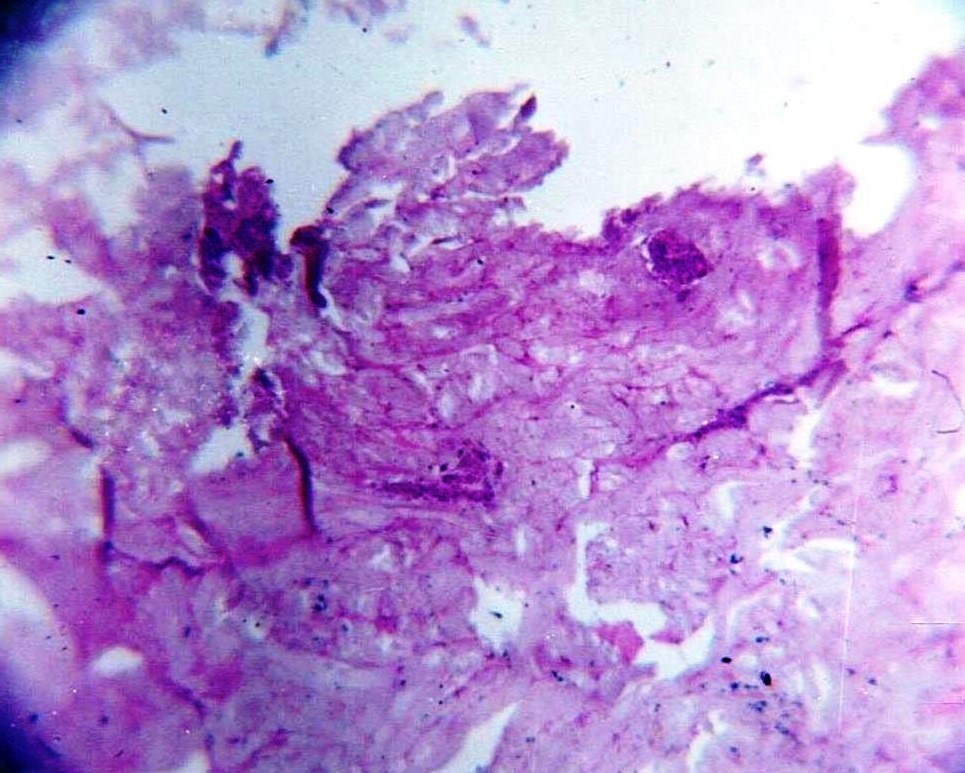
Epidermis was found burnt/charred [Table/Fig-2] in 18 (45%) of cases and bulla formation [Table/Fig-3] was present in 9 (22.5%) of the cases under study. Epidermal papillae were flattened [Table/Fig-4] in 19 cases (47.5%). Vesicular nuclei [Table/Fig-5] were seen in 2.5% cases. No significant change in epidermal cells of skin was seen in 3 (7.5%) of the cases.
Microphotograph showing charring of the epidermis with necrosis in the underlying dermis (100X).
Microphotograph showing bulla formation (100X).
Microphotograph showing flattening of papillae (400X).
Microphotograph showing vesicular nuclei in the epidermis (400X).
In 25 (62.5%) cases, necrotic changes [Table/Fig-6] were observed, adnexal structures were intact in 9 (22.5%) cases. Vacuolated appearance in dermis was seen in 5 (12.5%) cases. Charring and flattening of papillae were observed in 3 (7.5%) cases each in the study. Bulla formation in dermis was seen in 2 (5%) cases.
Microphotograph showing marked necrosis in the dermis (100X).
In none of the cases under study, inflammatory change or metallisation/calcification was noted. In the 20 control cases studied, charring of the skin was present in the epidermis/dermis and no further change in the epidermis/dermis were present in any of the control cases.
Discussion
In the present study, attempt has been made to know the histopathological changes in the skin as a result of electric current injury. Electric burn injury marks often appear as painless, depressed, yellow-grey, punctate areas with central necrosis. Isolated thermal burns may also be seen when clothing ignites. Superficial electric current injury may appear to be linear, punctate, feathering, or thermal burns. In high-voltage electric current injuries, muscle necrosis can extend to sites distant from the observed skin injury, and compartment syndromes occur as a result of vascular ischaemia and muscle oedema, further resulting in delayed thrombosis and haemorrhage [12].
We found 15% cases to have burnt clothing, but no such similar study could be found except generalised statements that clothing or shoes may be burnt in high voltage electrocution cases. In our study, visible electric current injury mark was seen in 85% cases; similarly most studies report visible marks in 62.5-100% cases [13-19]; however, one study reported visible burns in only 5.71-47.25% cases [20].
This is correct as per “Gross changes” in [Table/Fig-1] Laceration and deeper tissue involvement was noted in 7.5% cases. One study reported lacerations in 9.4% cases [15]. Blister formation, metallisation or inflammatory change was not present grossly in any of the cases studied. Various studies have described blistering in 9.4-21.98% cases [15,20]. Metallisation has been reported in one study in 2.2% cases [20]. Some authors have described erythema in 34.4% [15] cases; petechiae in 11.5% [14] and 48.3% [17] cases; and hyperkeratosis in 1.6% [15] and 45.4% [16] cases [Table/Fig-2].
On microscopic examination of the affected part of the skin, bulla formation, flattened papillae, vesicular nucleus and burnt epidermis were seen; the changes typical of electric current trauma. While doing microscopic examination of the dermal layer of the affected skin, necrotic changes, bulla formation, vacuolated appearance, intact adnexal structures and flattened dermal papillae were present. Calcification/metallisation or inflammatory change was not present in any of the cases studied, which can be due to the fact that time gap between electrical trauma and death of the victim was less than the usual time taken for these processes to develop microscopically, as reported by Danielsen L et al., [6]. In our study, perhaps no one survived for sufficient time whereby we could not observe the findings similar to them.
Bulla formation was seen in 22.5% cases in epidermis and 5% cases in dermis; whereas, another study described micro-blistering in 81.8% cases [16]. We found flattening of papillae in 47.5% cases in epidermis and 7.5% cases in dermis; however, no similar findings have been reported in other studies. Charring of epidermis was seen in 45% cases and dermis in 7.5% cases; whereas, other studies have reported charring in 46.9% cases [15]. We noted vesicular nuclei in 2.5% cases; whereas, other studies reported pyknotic nuclei in 54.5% cases [16], and nuclear streaming in 2.86-9.89% [20] to 33.3% [13] and 90.9-100% [16,18,19] cases. Epidermal erosion was observed in 12.5% cases and dermal separation in 77.5% cases; whereas, other studies reported dermo-epidermal separation in 33.3% [13], 73.3-83.3% [19], 90.9% [16], 100% [18] cases. Necrotic changes were seen in 62.5% cases; whereas, other studies reported necrosis in 6.3% [15], 46.7% [19], 60% [13], 66.6% [18], 90.9% [16] cases. Vacuolisation was seen in 12.5% cases; whereas, others reported it in 2.86-7.69% [20], 40% [13], 90.6% [15] cases [Table/Fig-7].
Electric current injury changes observed in other studies.
| Author | Duration | Cases | Place | Findings |
|---|
| Rathod MR et al., [13] | 1 year | 8 | Gujarat, India | Electric burns 62.5%, Petechial haemorrhage and necrosis 60.0%, Vacuolisation 40.0%, Intra-epidermal separation 33.3%, Epidermal nuclear elongation 33.3% |
| Wick R et al., [14] | 30 years | 96 | Adelaide, Australia | Electric burns 83.3%, Petechiae 11.5% |
| Al-Hadithi RHM et al., [15] | 1 year | 64 | Baghdad, Iraq | Electric burns 87.5%, Erythema 34.4%, Charring 46.9%, Blistering 9.4%, Laceration 9.4%, Coagulative necrosis 6.3%, Vacuolisation 90.6%, Hyperkeratosis 1.6% |
| Guntheti BK et., [16] | 1 year | 11 | Andhra Pradesh, India | Electric burns 90.9%, Streaming of nuclei 90.9%, Dermo-epidermal separation 90.9%, Degeneration of collagen in dermis with coagulative necrosis 90.9%, Pyknoses of nuclei 54.5%, Hyperkeratosis 45.4%, Micro blister formation 81.8%, Degeneration of collagen in Keratin layer 36.4%, Metallisation 81.8% |
| Shaha KK and Joe AE [17] | 5 years | 118 | Tamil Nadu, India | Electric burns 93.23%, Petechiae 48.30% |
| Viswakanth B and Shruthi P [18] | 1 year | 6 | Karnataka, India | Electric burns 100%, Sub-epidermal separation 100%, Nuclear streaming 100%, Epidermal coagulation necrosis 66.66% |
| Uzün I et al., [19] | Random | 30 | Istanbul, Turkey | Electric burns 100%, Intraepidermal separation 73.3%, Subepidermal separation 83.3%, Coagulation necrosis 46.7%, Nuclear elongation 100% |
| Blumenthal R [20] | 4 years | 126 | Gauteng, South Africa | Low voltage | Electric burns 47.25%, Blistering 21.98%, Vacuolisation 7.69%, Metallisation 2.20%, Streaming 9.89%, Eosinophilia 2.20% |
| High voltage | Electric burns 5.71%, Blistering 11.43%, Vacuolisation 2.86%, Streaming 2.86% |
| Present study | 2 years | 40 | Punjab, India | Electric burns 85%, Bulla formation 22.5%, Flattened papillae 47.5%, Vacuolisation 12.5%, Necrosis 62.5% |
Limitation
The major limitation of the study appears to be the small number of electric current injury cases, though all cases over the two year study period were included. Further studies are recommended for studying the findings in clinical cases admitted with electrocution and extending the study over more number of cases.
Conclusion
Majority of the fatalities occur within first half an hour of electric current injury. Grossly, the electric current injury indicated no blister formation, metallisation or any inflammatory response of the body. Microscopically too, no calcification or metallisation or inflammatory change was observed. Histopathological study in cases of electrocution could help the forensic pathologist in their diagnosis especially in cases with less typical findings or obscure circumstances; although, the microscopic features are not very specific. Electric contact mark is pathognomic of electrocution. Dermo-epidermal separation is a common histopathological finding. Histopathological changes can be used as supportive evidence in giving cause of death in such cases.
[1]. Moritz AR, Studies of thermal injury: III. The pathology and pathogenesis of cutaneous burns: an experimental studyAm J Pathol 1947 23(6):915-41. [Google Scholar]
[2]. Moritz AR, Physical agents in the causation of injury and diseaseIn: Pathology 1957 3rd edSt. LouisMosby:135-38. [Google Scholar]
[3]. Hughes JPW, Electric shock and associated accidentsBr Med J 1956 1(4971):852-55.10.1136/bmj.1.4971.85213304359 [Google Scholar] [CrossRef] [PubMed]
[4]. Franklin CA, Injuries from Burns, Scalds, Lightening and ElectricityIn: Modi’s Medical Jurisprudence and Toxicology 1988 21st edBombayN M Tripathi Pvt Ltd:231-49. [Google Scholar]
[5]. Dimick AR, Electrical injuriesIn: Harrison’s Principles of Internal Medicine 1994 13th edNew YorkMcGraw Hill:2480-82. [Google Scholar]
[6]. Danielsen L, Karlsmark T, Thomsen HK, Diagnosis of skin lesions following electrical tortureRomanian J Leg Med 1997 5:15-20. [Google Scholar]
[7]. Öztop F, Lök V, Baykal T, Tunca M, Signs of electrical torture on the skinAnkara: Human Rights Foundation of Turkey 1994 :97-104.(Treatment and rehabilitation centers report) [Google Scholar]
[8]. Prokop O, Lehrbuch der gerichtlichen MedizinTextbook of Judicial Medicine 1960 BerlinVolk & Gesundheit Publishers:611[In German] [Google Scholar]
[9]. Sammicheli M, Luchini D, Scaglione M, Salemmi O, Case report of an occupational electrocution fatality: histopathological, medicolegal, work safety and insurance implicationsPrev Res 2017 6(2):12-15.10.11138/PER/2017.6.2.012 [Google Scholar] [CrossRef]
[10]. Spencer HA, Lightning, lightning-stroke, and its treatment 1932 LondonBailliere, Tindall and Cox:91 [Google Scholar]
[11]. Culling CFA, Allison RT, Barr WT, Cellular pathology technique 1985 4th edLondonButterworths:64210.1016/B978-0-407-72903-2.50031-9 [Google Scholar] [CrossRef]
[12]. Price TG, Cooper MA, Electrical and Lightning Injuries. In: Marx JA, Hockberger RS, Walls RM, Biros MH, Ling LJ, Danzl DF, et al., editorsRosen’s Emergency Medicine – Concepts and Clinical Practice 2014 8th edPhiladelphiaSaunders:1906-14. [Google Scholar]
[13]. Rathod MR, Goswami H, Jankar D, A study of histopathological changes in burn deaths at civil hospital Ahmedabad, GujaratInt J Res Med 2014 3(1):42-45. [Google Scholar]
[14]. Wick R, Gilbert JD, Simpson E, Byard RW, Fatal electrocution in adults: a 30-year studyMed Sci Law 2006 46(2):166-72.10.1258/rsmmsl.46.2.16616683472 [Google Scholar] [CrossRef] [PubMed]
[15]. Al-Hadithi RHM, Al-Khateeb NGH, Abdullah MAJ, Forensic histopathological approach to electrocutionJ Fac Med Baghdad 2008 50(3):358-64. [Google Scholar]
[16]. Guntheti BK, Singh UP, Khaja S, Diagnosis of electric injuries: Histopathological examinationJ Indian Acad Forensic Med 2014 36(2):137-41. [Google Scholar]
[17]. Shaha KK, Joe AE, Electrocution-related mortality: a retrospective review of 118 deaths in Coimbatore, India, between January 2002 and December 2006Med Sci Law 2010 50(2):72-74.10.1258/msl.2010.01000820593598 [Google Scholar] [CrossRef] [PubMed]
[18]. Viswakanth B, Shruthi P, Low voltage electrocution deaths and histopathological findings: one-year prospective autopsy studyJ Curr Forensic Sci Res 2015 1:01-05. [Google Scholar]
[19]. Uzün I, Akyildiz E, Inanici MA, Histopathological differentiation of skin lesions caused by electrocution, flame burns and abrasionForensic Sci Int 2008 178(2-3):157-61.10.1016/j.forsciint.2008.03.01218472235 [Google Scholar] [CrossRef] [PubMed]
[20]. Blumenthal R, A retrospective descriptive study of electrocution deaths in Gauteng, South Africa: 2001-2004Burns J Int Soc Burn Inj 2009 35(6):888-94.10.1016/j.burns.2009.01.00919442447 [Google Scholar] [CrossRef] [PubMed]