Recurrent Primary Angiosarcoma of Breast–A Rare Entity
Namrata Rao1, Siddiq M Ahmed2
1 Assistant Professor, Department of Pathology, Melaka Manipal Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
2 Professor, Department of Pathology, Bangalore Medical College and Research Institute, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Namrata Rao, Flat No 14/6, B-Type Flats, KMC Quarters, Manipal-576104, Karnataka, India.
E-mail: doctornamrata2411@gmail.com
Angiosarcoma of the breast is a rare tumour with a reported incidence of only 0.04% of all breast malignancies. A 34-year-old lady presented with a lump in her right breast. In view of haemorrhage and few stromal fragments on Fine Needle Aspiration Cytology (FNAC), a diagnosis of phylloides was given. Simple mastectomy was done which showed a tumour with areas of haemorrhage. On microscopy anastomosing irregular vascular channels filled with RBC’s were noted. Sheets of tumour cells with high mitotic activity was observed at places. There were areas of haemorrhage and ischaemic necrosis. A diagnosis of angiosarcoma was made which was confirmed by immunohistochemistry (CD 34 and factor VIII). Eight months later she presented with a recurrent lump in her right chest wall following which lumpectomy was done. Microscopy showed similar features as in the earlier mastectomy specimen. On reviewing the fine needle aspiration slides we realised that the endothelial fragments were mistaken for stromal fragments.
The importance of this case report lies in the fact that primary breast angiosarcoma is a rare tumour which can develop without radiation exposure/history of previous breast surgery. The presence of spindle cells on fine needle aspiration slides necessitates careful examination and evaluation to rule out malignancy. It is important that the cytopathologist is aware of this possibility, to enable an early diagnosis.
Malignancy, Spindle cell, Stromal fragments
Case Report
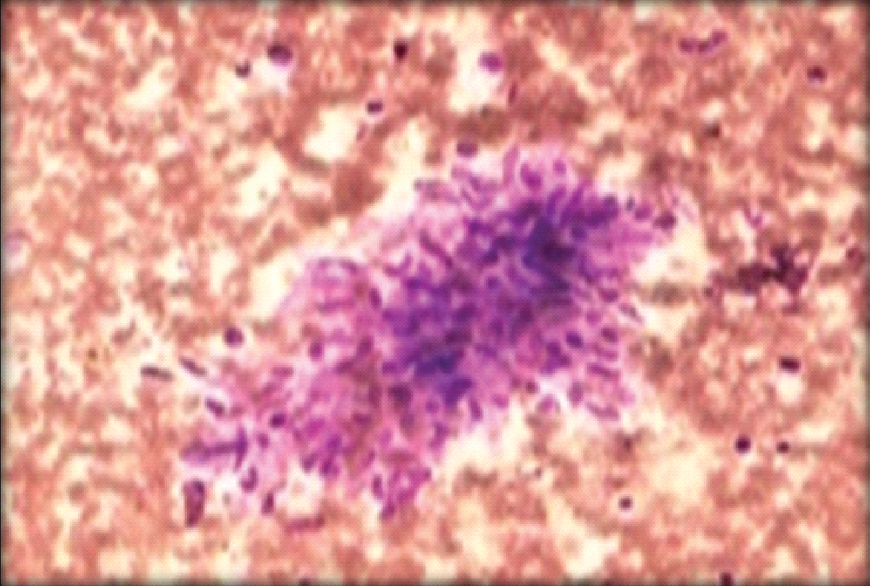
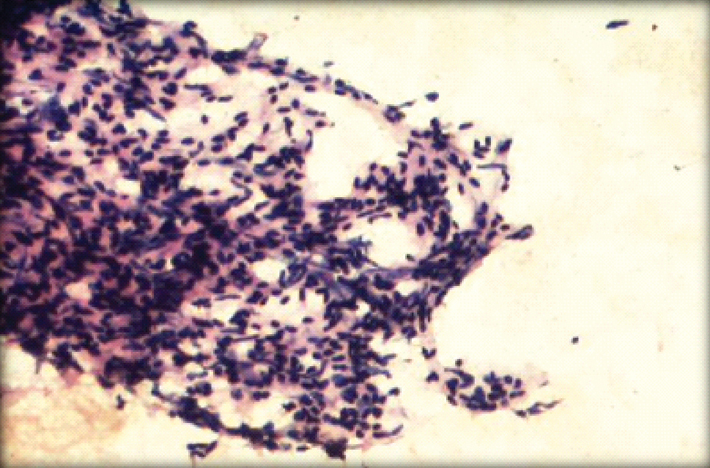
A 34-year-old woman presented with lump and pain in her right breast since two months. There was no family history of breast malignancy. On examination, the lump measured (10x8) cm, consistency was soft to firm. The patient was sent for FNAC. Aspiration done several times yielded only haemorrhagic material and showed few stromal fragments with spindle cells [Table/Fig-1]. Diagnosis of phylloides was given and the patient was operated.
Stromal fragments on fine needle aspiration cytology (Leishman stain, 10X).
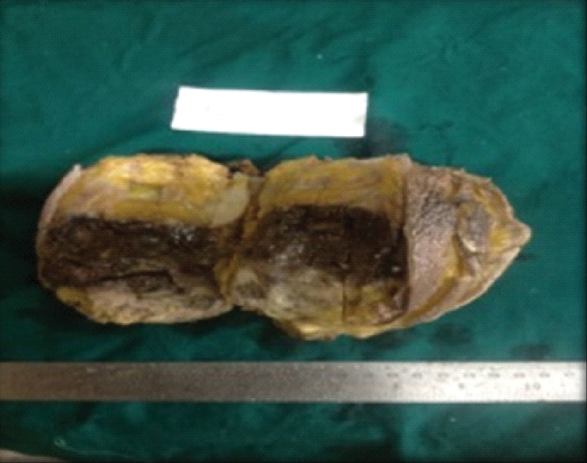
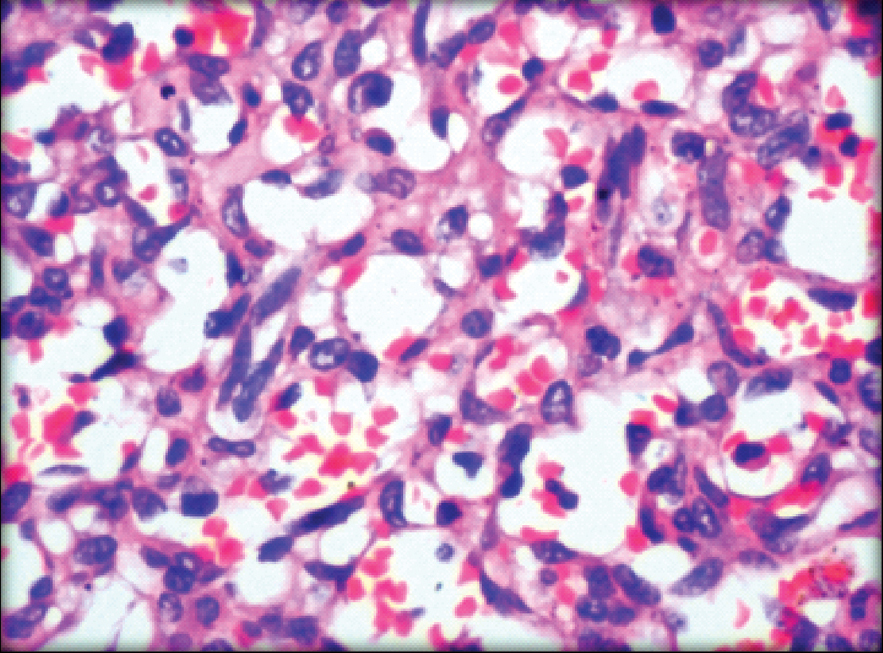
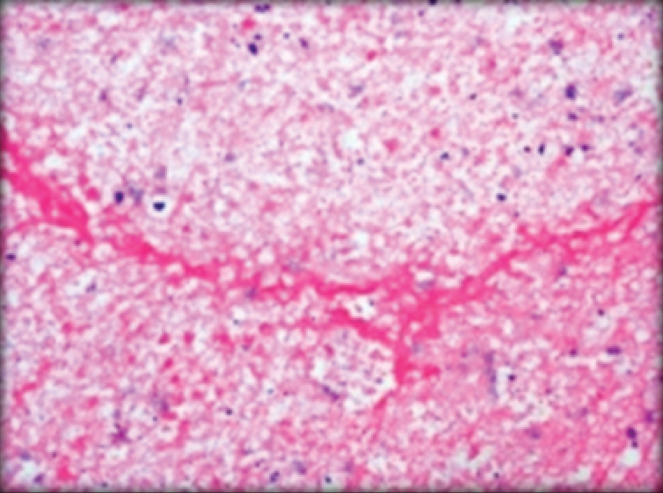
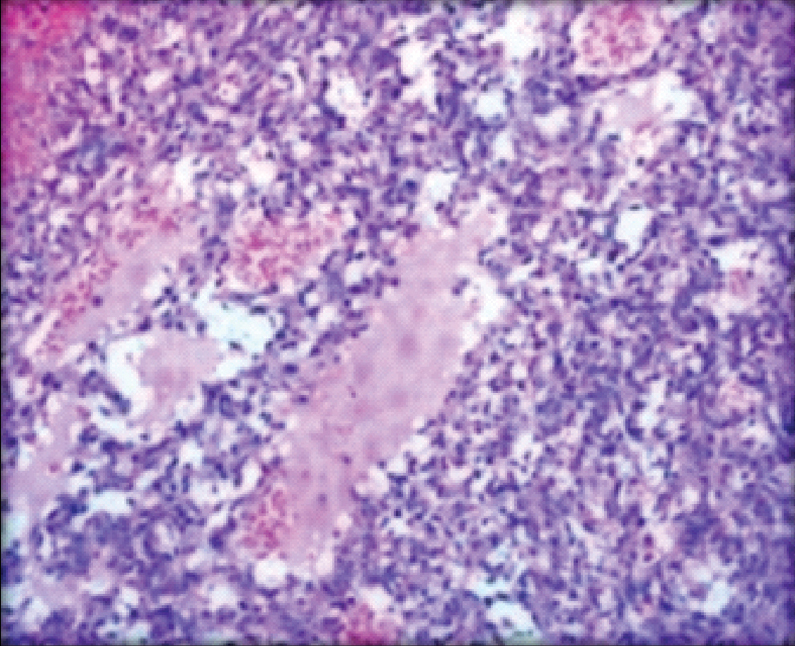
We received a simple mastectomy specimen which measured (13.0x8.0x5.0) cm. Cut surface showed a well circumscribed tumour with areas of haemorrhage measuring (7.5x7.0x5.0) cm. The tumour was 1.5 cm away from the deep resected margin [Table/Fig-2]. On microscopy, sections from the tumour showed anastomosing irregular vascular channels that were dissecting the stroma and were filled with RBC’s. The spaces were lined by epithelioid cells. The cells showed neo lumina formation [Table/Fig-3]. Sheets of tumour cells with high mitotic activity were observed at places. Areas of haemorrhage and ischaemic necrosis were noted [Table/Fig-4]. The nipple areola and deep resected margin were free of tumour. A diagnosis of angiosarcoma was given which was confirmed by Immunohistochemistry (IHC) (CD 34 and factor VIII) [Table/Fig-5].
Gross specimen showing tumour.
Anastomosing irregular vascular channels with neo lumina formation (H&E, 20X).
Areas of necrosis and haemorrhage (H&E, 10X).
CD34 staining (IHC, 10X).
Eight months later she again presented with a recurrent lump in her right chest wall following which, excision of the lump was done. The patient was not sent for FNAC. The lumpectomy specimen measured (10.0x8.0x4.0) cm. Cut surface was haemorrhagic. On microscopy, the features were similar to that seen in the earlier mastectomy specimen [Table/Fig-6]. Patient was referred to the regional oncology centre for further management.
Anastomosing vascular channels (H&E, 10X).
Discussion
Breast sarcomas arise from the stroma of the mammary gland [1]. Angiosarcoma of the breast is a rare tumour, the incidence of which is only 0.04% of all breast malignancies [2]. It is said that upto 70% of angiosarcoma cases relapse, most commonly as local recurrence [3]. It arises from the endothelial lining of the blood vessels [4]. Primary angiosarcomas are rare as compared to secondary ones. Primary angiosarcomas are diagnosed when the patients never had breast cancer while secondary angiosarcomas occur after radical mastectomy or lumpectomy and radiation. Both primary and secondary angiosarcomas have similar morphology. Primary tumours commonly occur during the third and fourth decades of life, as in our case whereas secondary ones occur in women over 40, five to ten years after radiotherapy for breast cancer. Most of these lesions develop in patients after breast conservation treatment within the prior irradiation field [5]. There is a long latent period (median 59–90 months) between radiotherapy and the diagnosis of angiosarcoma [6]. Both primary and secondary breast angiosarcomas carry a worse prognosis as compared to breast carcinoma [7].
Primary breast angiosarcoma is a rare tumour which has around 170 cases documented in literature [8]. Radiographic assistance in reaching the diagnosis is limited. Skin thickening or an ill-defined superficial mass may be seen on mammography, but the findings are often non-specific. Nearly, 33% of patients with angiosarcomas of breast have negative findings on mammography [9]. Preoperative diagnosis by aspiration cytology and biopsy was found to be difficult by some authors [10,11]. In our case too, the presence of stromal fragments led to a diagnosis of Phylloides. On reviewing the FNAC slides, we realised that the endothelial fragments were mistaken for stromal fragments [Table/Fig-7]. Recognition of cytologic vasoformative features and integration of these features with immunocytochemical evidence of endothelial differentiation can establish the correct FNAC diagnosis of angiosarcoma.
Endothelial fragments on fine needle aspiration cytology (H&E, 10X).
Breast angiosarcoma usually present as a rapidly growing palpable mass, without pain [12,13]. In our case, the patient presented with lump rapidly growing over a short period of two months. Grossly the tumour is soft, spongy and haemorrhagic. Microscopically three grades of angiosarcoma are described-Anastomosing vascular channels are seen in tumours of low-grade. Intermediate-grade tumours have more solid areas with increased mitosis. High-grade lesions (as in our case) are predominantly solid sarcomatous with necrotic, infarcted and haemorrhagic areas. Diagnostic areas are characterised by interanastomosing vascular channels lined by atypical endothelial cells. The endothelial cells show reactivity for several markers, including CD31, CD34 and von Willebrand factor (factor VIII).
Angiosarcoma carries a poor prognosis, most of the patients develop metastasis via the blood stream [14]. This type of breast cancer is aggressive, has a high rate of recurrence and the prognosis depends on the stage at the time of diagnosis. The estimated disease-free survival five years after initial treatment is 76% for patients with Grade-1 tumours and 15% for patients with grade-3 tumours [15].
Conclusion
Primary Angiosarcomas of the breast are rare heterogenous group of vascular malignancies typified by frequent local/metastatic recurrence. The importance of this case report lies in the fact that primary breast angiosarcoma is a rare tumour which can develop without radiation exposure/history of previous breast surgery. The presence of spindle cells on FNAC slides indicates high potentiality towards malignancy. It is important that the cytopathologist is aware of this possibility, to enable an early diagnosis.
[1]. Yang G, Li J, Jin H, Ding H, Is mammary not otherwise specified-type sarcoma with CD10 expression a distinct entity? A rare case report with immunohistochemical and ultrastructural studyDiag Pathol 2013 8(1):1410.1186/1746-1596-8-1423356903 [Google Scholar] [CrossRef] [PubMed]
[2]. Kardum-Skelin I, Jelic-Puskaric B, Pazur M, Vidic-Paulisic I, Jakic-Razumovik J, Separovic V, A case report of breast angiosarcomaColl Antropol 2010 34(2):645-48. [Google Scholar]
[3]. Bennani A, Chbani L, Lamchahab M, Wahbi M, Alaoui FF, Badioui I, Primary angiosarcoma of the breast: A case reportDiagnostic Pathology 2013 8:6610.1186/1746-1596-8-6623607567 [Google Scholar] [CrossRef] [PubMed]
[4]. Bohn OL, de León EA-P, Lezama O, Rios-Luna NP, Sánchez-Sosa S, Llombart-Bosch A, Pulmonary artery sarcoma with angiosarcoma phenotype mimicking pleomorphic malignant fibrous histiocytoma: a case reportDiag Pathol 2012 7:15410.1186/1746-1596-7-15423134683 [Google Scholar] [CrossRef] [PubMed]
[5]. Vorburger SA, Xing Y, Hunt KK, Lakin GE, Benjamin RS, Feig BW, Angiosarcoma of the breastCancer 2005 104:2682-88.10.1002/cncr.2153116288486 [Google Scholar] [CrossRef] [PubMed]
[6]. Sener SF, Miloss Feldman JL, Martz CH, Winchester DJ, Dieterich M, The spectrum of vascular lesions in the mammary skin, including angiosarcoma, after breast conservation treatment for breast cancerJ Am Coll Surg 2001 193(1):22-28.10.1016/S1072-7515(01)00863-8 [Google Scholar] [CrossRef]
[7]. Babarović E, Zamolo G, Mustać E, Strčić M, High grade angiosarcoma arising in fibroadenomaDiag Pathol 2011 6:12510.1186/1746-1596-6-12522185665 [Google Scholar] [CrossRef] [PubMed]
[8]. Osama Abu-Salem MD, Angiosarcoma of the breast: A case reportJRMS18(1):71-75. [Google Scholar]
[9]. Iberman L, Dershaw DD, Kaufman R, Rosen PP, Angiosarcoma of breastRadiol 1992 183:64910.1148/radiology.183.3.15849131584913 [Google Scholar] [CrossRef] [PubMed]
[10]. Farrokh D, Hashemi J, Zandi B, Angiosarcoma of the breastIran J Radiol 2006 3:81 [Google Scholar]
[11]. Pohar-Marinsek Z, Lamovec J, Angiosarcoma in FNAC smears: diagnostic accuracy, morphology, immunocytochemistry and differential diagnosesCytopathology 2010 21(5):311-19.10.1111/j.1365-2303.2009.00726.x20105214 [Google Scholar] [CrossRef] [PubMed]
[12]. Johnson CM, Garguilo GA, Angiosarcoma of the breast: a case report and literature reviewCurrent Surgery 2002 59(5):490-94.10.1016/S0149-7944(02)00629-3 [Google Scholar] [CrossRef]
[13]. Georgiannos S, Sheaff M, Angiosarcoma of the breast: a 30 year perspective with an optimistic outlookBritish Journal of Plastic Surgery 2003 56(2):129-34.10.1016/S0007-1226(03)00025-0 [Google Scholar] [CrossRef]
[14]. Rosai J, Rosai and Ackerman’s surgical pathology. 10th ed. Chapter 20: Breast 2011 Mosby Elsevier:1725-26. [Google Scholar]
[15]. Glazebrook KN, Magut MJ, Reynolds C, Angiosarcoma of the breastAm J Roentgenol 2008 190:533-38.10.2214/AJR.07.290918212243 [Google Scholar] [CrossRef] [PubMed]