Introduction
Acute Coronary Syndrome (ACS) includes a spectrum of disorders ranging from unstable angina to myocardial infarction. Since, ACS is an important cause of mortality in the world, early diagnosis of the disease is very important. Ischaemia Modified Albumin (IMA) is an ischaemia biomarker that has been approved by the US Food and Drug administration and has clinical application. Although, many studies have been done on IMA as a biomarker in ACS patients, role of IMA for differentiating patients with unstable angina, Non ST-Segment Elevation Myocardial Infarction (NSTEMI) and ST-Segment Elevation Myocardial Infarction (STEMI) requires further study.
Aim
To assess the diagnostic role of IMA in ACS patients and evaluate correlation between IMA and necrotic biomarkers such as cardiac Troponin I (cTnI) and Creatine kinase-myoglobin binding (CKmb) in ACS patients.
Materials and Methods
The study included 75 subjects with ACS, who were divided into three groups of 25 patients each: Unstable angina, NSTEMI and Myocardial Infarction (MI) and 25 healthy people as control. They were enrolled into the study from the Fatemeh Zahra Heart Center, Sari, Iran, between November 2015 and October 2016. IMA was measured by the Cobalt-Albumin Binding (CAB) assay, cTnI was measured by rapid immunoassay and CKmb was estimated utilising colorometric enzyme method by commercial kits. The correlation between IMA and necrotic biomarkers was determined using a Pearson correlation analysis. Receiver Operator Characteristic (ROC) curve was used to assess role of IMA in diagnosis of ACS.
Results
IMA levels in unstable angina patients were significantly higher than NSTEMI and MI (p<0.001). While there was no significant difference in IMA levels between NSTEMI and MI (p=0.675). Bivariate correlation analyses were performed to assess for any relationship between IMA levels and two common cardiac biomarkers (p>0.5, r=0.25). The area under the ROC curve of IMA for ACS patients was 0.783. The sensitivity, specificity, Positive Predictive Value (PPV) and Negative Predictive Value (NPV) of IMA was 74.7%, 72%, 88.9% and 48.6% respectively.
Conclusion
IMA is a useful biomarker in diagnosis of ACS especially unstable angina patients and there is no significant correlation between IMA and necrotic biomarkers (cTnI and CKmb) in ACS patients.
Creatine kinase myoglobin binding, Cardiac troponin I, Cobalt-albumin binding assay
Introduction
According to the heart disease and stroke statistics-2016 Update, One of every seven deaths occurred in the United States in 2013 due to Coronary Heart Disease (CHD). The prevalence of new and regressive coronary attack is estimated 6,60,000 and 3,05,000 Americans yearly [1].
ACS which can be considered as a subset of CHD, is a term that refers to a set of clinical symptoms indicative of myocardial ischaemia and encompasses a spectrum of conditions which include unstable angina, NSTEMI and STEMI [2-4].
Most cases of ACS are due to rupture of an atherosclerotic plaque in a coronary artery and lead to formation of a thrombus [5]. In majority of patients with ACS including unstable angina and NSTEMI, thrombus causes partial and intermittent obstruction. On contrary complete occlusion of the coronary artery is the main cause of STEMI [6].
Unstable angina and NSTEMI have similar clinical presentations and pathophysiologic origins and also differ in severity and necrotic biomarker releasing changes [3]. This means that NSTEMI is severe enough to cause myocardial damage and release CKmb and cTnI [3,7].
Clinical presentation, electrocardiogram and biochemical markers are important components for the diagnosis of ACS. Most conventional biomarkers such as CKmb, and cTnI are indicative of cell necrosis [8]. Finding a biomarker that increases before necrosis can be highly effective in early diagnosis of ACS [9].
IMA which is a form of human serum albumin was introduced as a potential biomarker of myocardial ischaemia by US Food and Drug administration [10]. In the ischaemic condition, the N-terminal sequence of human albumin (NH2-Asp-Ala-His-Lys) undergoes transient modifications by free radicals, these modifications lead to a reduced metal binding capacity for cobalt in comparison to non ischaemic normal controls, hence concentration of IMA increases [11-14].
The present study was aimed to determine the correlation between IMA with CKmb and cTnI in ACS patients and compare usefulness of this biomarker for the diagnosis of unstable angina, NSTEMI and MI subjects.
Materials and Methods
The present non interventional case control study was conducted at the Department of Clinical Biochemistry in collaboration with Department of Cardiology in Mazandaran University of Medical Sciences, Sari, Iran. Ethical approval to carry out this study was given by the Research Ethics Committee of Mazandaran University of Medical Science, Iran.
Patient Selection
A total of 75 ACS patients with age group of 30 to 80 years including 41 male and 34 female, were taken up for the study. ACS patients were diagnosed by cardiologists on the basis of history, physical examination, chest pain duration, ECG changes and cardiac biomarkers (CKmb and cTnI).
The ACS patients were divided into three groups including unstable angina (25 subjects), NSTEMI (25 subjects) and STEMI (25 subjects), by physicians according to American College of Cardiology/American Heart Association (ACC/AHA) guideline for the management of patients with ACS [15]. Twenty five subjects as control group with age and sex matched individuals, normal ECGs and without any malignant or cardiac disease were also enrolled in the study. Patients and control groups gave the informed consent before the study.
Exclusion Criteria
Patients with renal, hepatic and infectious disease, diabetes mellitus, stroke and cirrhosis were excluded from the study.
Sampling
On admission, 5 mL blood was collected from the patients using standard aseptic techniques. The samples were centrifuged and serum was separated for measuring IMA, cTnI and CKmb. The cTnI was measured by rapid immunoassay (Immunochromatography) method using a kit from Nano-check TM AMI cardiac test. A cTnI>0.5 ng/mL was considered as positive value. CKmb was measured by a colorimetric enzyme assay (Pars Azmoon Kit) on a Hitachi autoanalyser. Remaining part of the sample was kept at -70°C for assay of IMA.
Laboratory Measurements
Ischaemia modified albumin was measured by the CAB assay [16]. Briefly, 3 μL CoCl2 and 40 μL sample were added to 131.8 μL KH2PO4 as a buffer solution. After 10 minutes incubation at room temperature, 5.2 μL Dithiotritol (DTT) was added. Finally, 20 μL 9% NaCl was added. The absorbance was measured at 470 nm and reported by Absorbance Unit (ABSU) parameter.
Statistical Analysis
The statistical analysis was executed using SPSS version 19.0. Student’s t-test was applied for comparison of means of ACS and control groups and one-way ANOVA test was performed between three groups of ACS. The correlations among IMA and cardiac biomarkers were evaluated in ACS patients using a Pearson correlation analysis. ROC curve analysis was performed and the optimal cut off for the IMA was selected. The sensitivity and specificity of IMA were assessed by ROC curve. All the data was expressed as mean±standard deviation and a two-tailed p-value <0.05 was considered to be statistically significant.
Results
Baseline demographic and clinical characteristics of study population are shown in [Table/Fig-1].
Clinical characteristics of the study groups.
| Variable | ACS (n=75) | Control (n=25) | p-value |
|---|
| UA (n=25) | NSTEMI (n=25) | MI (n=25) |
|---|
| Age (years) | 63.32±13.41 | 64.36±14.53 | 58.24±14.74 | 61.92±10.41 | - |
| Gender (M/F) | F:11 M:14 | F:15 M:10 | F:8 M:17 | F:12 M:13 | - |
| cTnL (ng/mL) | 0.652±0.404 | 21.87±15.9 | 40.85±24.80 | 0.257±0.093 | p<0.001*p<0.001**p=0.01*** |
| CKmb (U/L) | 20.64±2.71 | 34.96±27.69 | 114.36±114.66 | 20.24±4.03 | p<0.05*p<0.001**p<0.001*** |
| IMA (ABSU) | 0.874±0.111 | 0.609±0.119 | 0.575±0.086 | 0.535±0.037 | p<0.001*p<0.001**p=0.675***p<0.05**** |
Data were presented as mean±standard deviation, p-value significant at 0.05 level
ACS: Acute coronary syndrome; UA: Unstable angina; NSTEMI: Non ST-segment elevation myocardial infarction; MI: ST-segment elevation myocardial infarction; IMA: Ischaemia modified albumin; cTnI: Cardiac troponin I; CKmb: Creatin kinase myoglobin binding.
*Unstable angina vs. NSTEMI; **Unstable angina vs. MI; ***NTEMI vs MI; **** ACS vs. Control
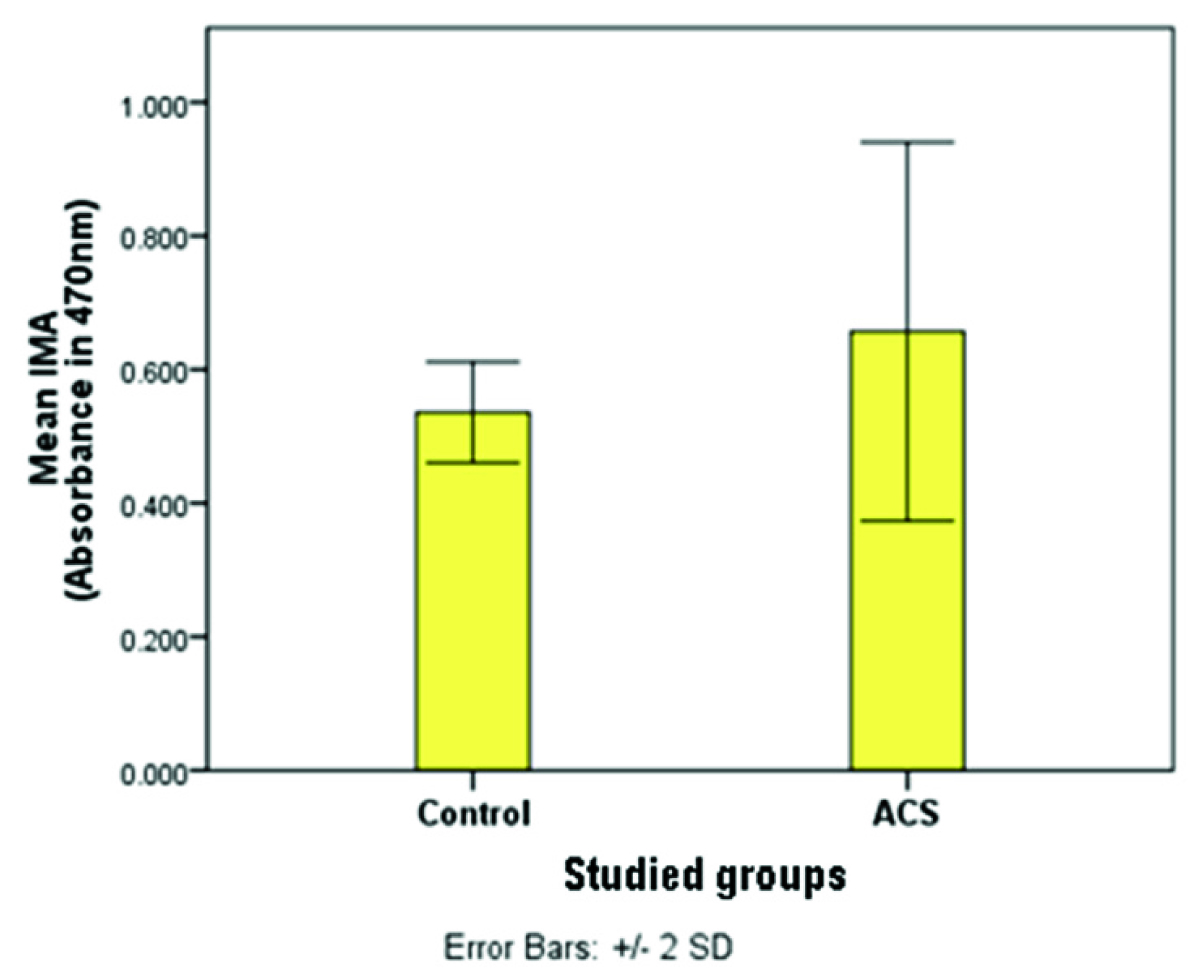
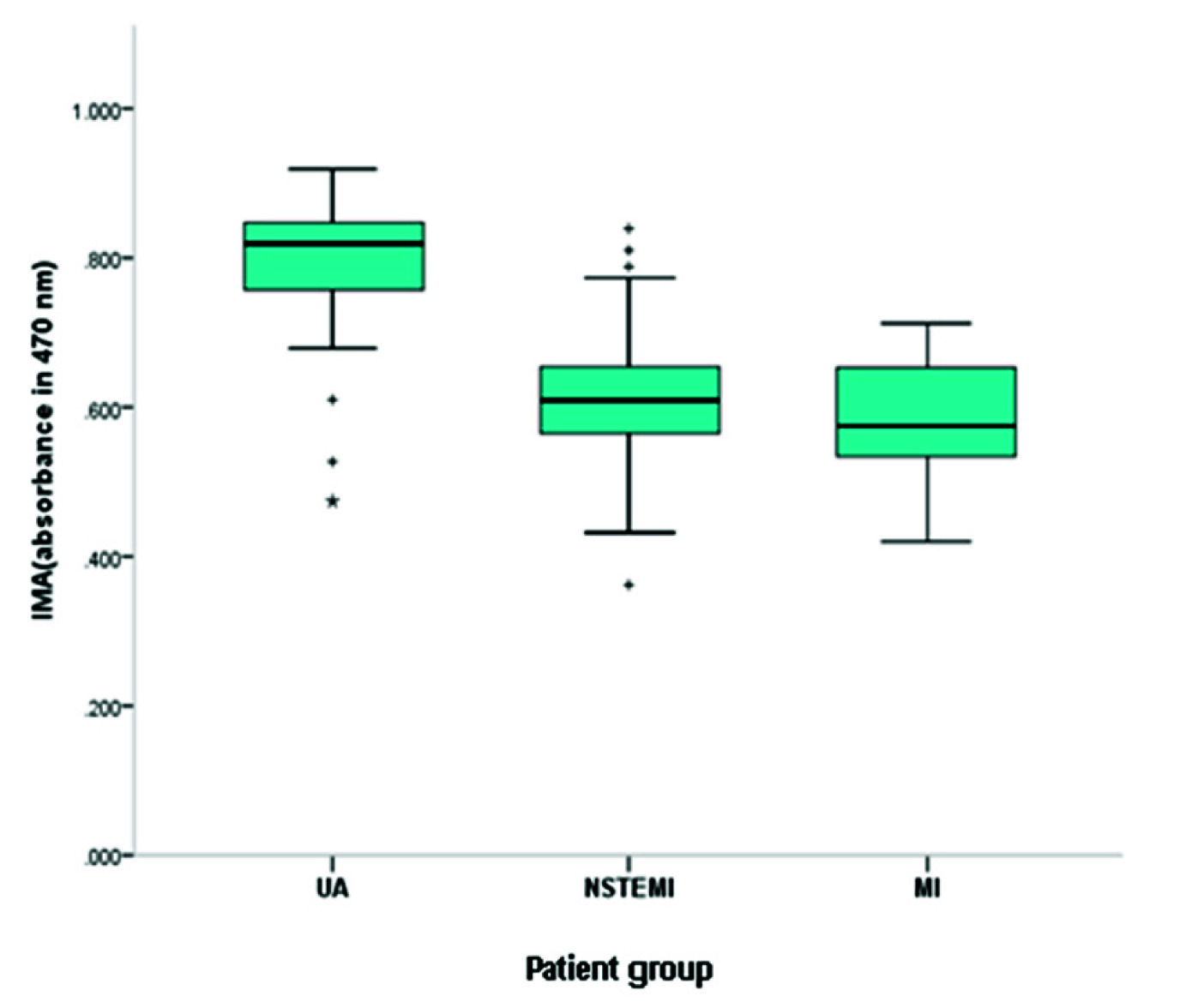
As shown in [Table/Fig-1], cTnI levels (p<0.001) and CKmb levels (p<0.001) were elevated in ACS group compared to control group. IMA levels in ACS patients were significantly higher than controls (p<0.001) [Table/Fig-2]. Furthermore, IMA levels were significantly higher in patients with unstable angina compared with NSTEMI and MI (p<0.001) but there was no significant difference between NSTEMI and MI (p=0.675) [Table/Fig-3].
IMA levels in ACS patients and control group (p-value <0.05).
IMA levels in ACS group.
(p-value UA<0.001), (p-value NSTEMI and MI=0.675)
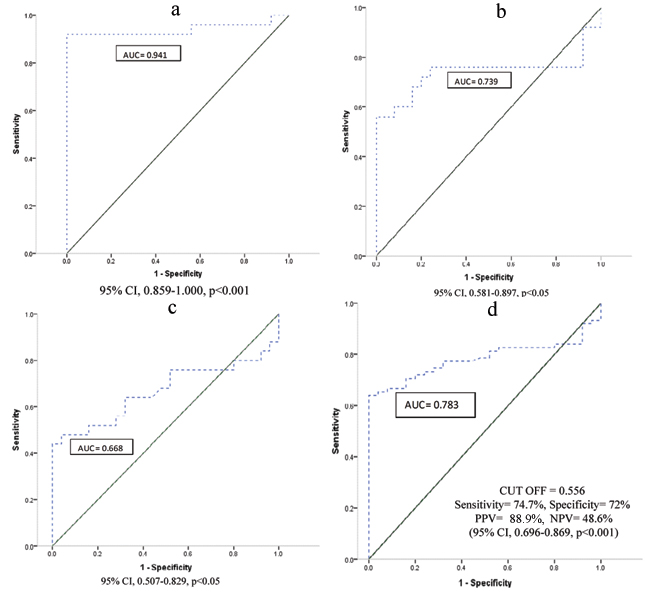
Bivariate correlation analyses were performed to assess for any relationship between IMA levels and two common cardiac biomarkers, cTnI and CKmb in ACS group. There was no positive or negative correlation between the levels of IMA and common cardiac biomarkers in unstable angina, NSTEMI and MI groups (p>0.05). The area under ROC curve for diagnostic ACS based on IMA levels was 0.783 (95% CI, 0.696-0.869, p<0.001). Separate entity wise ROC curve analysis for UA, NSTEMI and MI is also presented in [Table/Fig-4]. IMA levels >0.556 ABSU yielded a sensitivity of 74.7% and a specificity of 72%, a PPV of 88.9% and a NPV of 48.6% for the diagnosis of ACS.
Receiver operator characteristic curves: a) ROC of IMA in unstable angina group; b) ROC of IMA in NSTEMI; c) ROC of IMA in MI; d) ROC of IMA in ACS.
Discussion
In the present study we assessed IMA using CAB assay© proposed by Lee E et al., to investigate role of IMA in diagnosis of unstable angina, NSTEMI and MI patients and hypothesised that measuring the level of IMA in combination with necrotic biomarkers (cTnI and CKmb) can improve the efficiency of ACS diagnosis, especially diagnosis of unstable angina [16]. Many studies have been done on the role of IMA in diagnosis of ACS [9,11,13,17-20] and in most of them, IMA were measured using Albumin Cobalt Binding test (ACB test©) described by Bar-Or D et al., [21].
Using of buffering system, low sample volume and resistance to pH changes are some advantages of CAB assay compared to ACB test [22].
In this study, we reported that IMA levels in the ACS patients were significantly higher than control group. This finding was similar to the results of other studies [11,17,18,20]. Moreover, our results showed that IMA levels were significantly higher in individuals with unstable angina compared to the other two groups of patients (p<0.05), whereas there was no significant difference in IMA levels between MI patients and NSTEMI. In support of our results, Kountana E et al., showed IMA levels as a useful tool for excluding unstable angina [23]. One study also represented IMA as a potential biomarker in diagnosis of unstable angina [24]. They hypothesised that lesser albumin will be exposed to free radicals in myocardial necrosis compared to non necrotic damage, so less IMA will be made. Furthermore, myocardial necrosis causes limiting IMA access to circulation. However, other studies showed IMA as a poor discriminator between MI and unstable angina [20,25].
In a recent study on the role of IMA in CAD, IMA came out to be as a strong predictor of CAD in patients with unstable angina pectoris [26].
According to the results of the present study and mentioned studies above, IMA can be a good biomarker in early diagnosis of ACS in emergency room. Our study showed that there was an elevated level of CKmb and cTnI besides IMA levels in NSTEMI and MI patients, while IMA was a significant biomarker in unstable angina patients. So, we suggested elevated level of IMA without increased level of cardiac biomarker such as CKmb and cTnI may be a useful biomarker in diagnosis of unstable angina. Since, bivariate correlation analysis of IMA with cTnI and CKmb showed no significant correlation in unstable angina, NSTEMI and MI patients so, more studies are needed. The correlation results are in agreement with those reported by Ertekin B et al., and Chek J et al., and Bonorino NF et al., [18,27,28].
Based on the results of ROC curve analysis for IMA, the sensitivity and specificity was found to be 74.7% and 72% respectively. A study demonstrated a sensitivity of 76% and a specificity of 74% for IMA assay in CAD patients, which were quite close to our results [26]. Although, many studies suggested high specificity for IMA in ACS [11,18,29]. There are many studies that expressed increased level of IMA in non cardiac ischaemia conditions like type 2 diabetes mellitus, Liver disease, thyroid disorders and pregnancy [30-33]. Thus, IMA may not be a specific marker for cardiac ischaemia and this observation may be due to non usage of IMA as much as cTnI and CKmb in emergency room.
In a study done by Reddy CB et al., on 89 subjects, IMA levels were higher in patients with unstable angina compared to NSTEMI [20]. However, firstly, they indicated that positive IMA levels alone cannot differentiate between unstable angina and MI and secondly it wasn’t possible to distinguish between AMI and unstable angina (area under ROC curve 0.66).
Our results are in agreement with first part, IMA levels should be investigated besides another cardiac marker to differentiate between unstable angina and MI. However, contrary to second part, in the present study the AUC for IMA concentration in unstable angina and MI was 0.941 and 0.668, respectively. The results of the present study supported that IMA plays an important role in diagnosis of ACS and besides another cardiac markers (CKmb and cTnI), IMA can be a differential biomarker between unstable angina and MI.
Limitation
Limited number of participants were enrolled in the study, albumin-adjusted IMA levels were not calculated, increased level of IMA in such non ischaemic condition and using a colorimetric assay (CAB assay) as an indirect measurement method were considered as limitations of the present study.
Conclusion
The results of the present study confirms the valuable role of IMA in diagnosis of ACS especially unstable angina patients. On the other hand, our results suggest that increased level of IMA without elevated levels of necrotic biomarkers such as cTnI and CKmb can be a useful biomarker in diagnosis of unstable angina, although further studies are required to assess IMA in unstable angina patients.
Data were presented as mean±standard deviation, p-value significant at 0.05 level
ACS: Acute coronary syndrome; UA: Unstable angina; NSTEMI: Non ST-segment elevation myocardial infarction; MI: ST-segment elevation myocardial infarction; IMA: Ischaemia modified albumin; cTnI: Cardiac troponin I; CKmb: Creatin kinase myoglobin binding.
*Unstable angina vs. NSTEMI; **Unstable angina vs. MI; ***NTEMI vs MI; **** ACS vs. Control
[1]. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Executive summary: Heart Disease and Stroke Statistics-2016 update: A report from the American Heart AssociationCirculation 2016 133(4):447-54.10.1161/CIR.000000000000036626811276 [Google Scholar] [CrossRef] [PubMed]
[2]. Tan YC, Sinclair H, Ghoorah K, Teoh X, Mehran R, Kunadian V, Gender differences in outcomes in patients with acute coronary syndrome in the current era: A reviewEuropean Heart Journal: Acute Cardiovascular Care 2016 5(7):51-60.10.1177/204887261561088626450783 [Google Scholar] [CrossRef] [PubMed]
[3]. Kumar A, Cannon CP, Acute coronary syndromes: diagnosis and management, part IMayo Clin Proc 2009 84(10):917-38.10.4065/84.10.91719797781 [Google Scholar] [CrossRef] [PubMed]
[4]. Worrall A, Fletcher G, Acute coronary syndromes—assessment and interventionsManagement 2017 8:12-17. [Google Scholar]
[5]. Fuster V, Stein B, Ambrose JA, Badimon L, Badimon JJ, Chesebro JH, Atherosclerotic plaque rupture and thrombosis. Evolving conceptsCirculation 1990 82(3 Suppl):II47-59. [Google Scholar]
[6]. Moe KT, Wong P, Current trends in diagnostic biomarkers of acute coronary syndromeAnn Acad Med Singapore 2010 39(3):210-15. [Google Scholar]
[7]. Braunwald E, Unstable angina and non–ST elevation myocardial infarctionAmerican Journal of Respiratory and Critical Care Medicine 2012 185(9):924-32.10.1164/rccm.201109-1745CI22205565 [Google Scholar] [CrossRef] [PubMed]
[8]. Christenson RH, Duh SH, Sanhai WR, Wu AH, Holtman V, Painter P, Characteristics of an albumin cobalt binding test for assessment of acute coronary syndrome patients: a multicenter studyClin Chem 2001 47(3):464-70. [Google Scholar]
[9]. Vijaya D, Gayathri B, Role of ischemia modified albumin in the early diagnosis of acute myocardial infarctionInnovative Journal of Medical and Health Science 2014 4(1):353-58. [Google Scholar]
[10]. Peacock F, Morris DL, Anwaruddin S, Christenson RH, Collinson PO, Goodacre SW, Meta-analysis of ischemia-modified albumin to rule out acute coronary syndromes in the emergency departmentAmerican Heart Journal 2006 152(2):253-62.10.1016/j.ahj.2005.12.02416875905 [Google Scholar] [CrossRef] [PubMed]
[11]. Patil SM, Banker MP, Padalkar RK, Pathak AP, Bhagat SS, Ghone RA, The clinical assessment of ischaemia modified albumin and troponin I in the early diagnosis of the acute coronary syndromeJ Clin and Diagn Res 2013 7(5):804-08.10.7860/JCDR/2013/5288.294423814715 [Google Scholar] [CrossRef] [PubMed]
[12]. Apple FS, Clinical and analytical review of ischemia: modified albumin measured by the albumin cobalt binding testAdv Clin Chem 2005 39:01-10.10.1016/S0065-2423(04)39001-3 [Google Scholar] [CrossRef]
[13]. Chowdhury N, De A, Bhattacharya R, Chakraborty I, Ischemia modified albumin in myocardial infarction and its correlation with selected acute phase reactantsNigerian Journal of Cardiology 2015 12(2):65-70.10.4103/0189-7969.152028 [Google Scholar] [CrossRef]
[14]. Albarello K, dos Santos GA, Bochi GV, Sangoi MB, Almeida TC, da Silva JE, Ischemia modified albumin and carbonyl protein as potential biomarkers of protein oxidation in hemodialysisClin Biochem 2012 45(6):450-54.10.1016/j.clinbiochem.2012.01.03122342921 [Google Scholar] [CrossRef] [PubMed]
[15]. Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Ganiats TG, Holmes DR, 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromesCirculation 2014 130:e344-e426.10.1161/CIR.0000000000000134 [Google Scholar] [CrossRef]
[16]. Lee E, Eom JE, Jeon KH, Kim TH, Kim E, Jhon GJ, Evaluation of albumin structural modifications through cobalt-albumin binding (CAB) assayJournal of Pharmaceutical and Biomedical Analysis 2014 91:17-23.10.1016/j.jpba.2013.12.00324434278 [Google Scholar] [CrossRef] [PubMed]
[17]. Gurumurthy P, Borra SK, Yeruva RK, Victor D, Babu S, Cherian KM, Estimation of ischemia modified albumin (IMA) levels in patients with acute coronary syndromeIndian Journal of Clin Biochem 2014 29(3):367-71.10.1007/s12291-013-0367-324966488 [Google Scholar] [CrossRef] [PubMed]
[18]. Ertekin B, Kocak S, Dundar ZD, Girisgin S, Cander B, Gul M, Diagnostic value of ischemia-modified albumin in acute coronary syndrome and acute ischaemic strokePak J Med Sci 2013 29(4):1003-07.10.12669/pjms.294.317624353676 [Google Scholar] [CrossRef] [PubMed]
[19]. Hazini A, Cemek M, Alpdagtas S, Önül A, Senel Ü, Kocaman T, Investigation of ischemia modified albumin, oxidant and antioxidant markers in acute myocardial infarction. Postepy w Kardiologii InterwencyjnejAdvances in Interventional Cardiology 2015 11(4):298-303.10.5114/pwki.2015.5560026677379 [Google Scholar] [CrossRef] [PubMed]
[20]. Reddy CB, Cyriac C, Desle HB, Role of “Ischemia Modified Albumin” (IMA) in acute coronary syndromesIndian Heart Journal 2014 66(6):656-62.10.1016/j.ihj.2014.12.00525634401 [Google Scholar] [CrossRef] [PubMed]
[21]. Bar–Or D, Lau E, Winkler JV, A novel assay for cobalt-albumin binding and its potential as a marker for myocardial ischemia-a preliminary reportJournal of Emergency Medicine 2000 19(4):311-15.10.1016/S0736-4679(00)00255-9 [Google Scholar] [CrossRef]
[22]. Reddy VS, Hemadri V, Pasupuleti P, Perugu B, Lee E, Eoma JE, Cobalt-albumin binding (CAB) assay: An advantageous and flaw free testing of albumin-cobalt bindingJournal of Pharmaceutical and Biomedical Analysis 2014 99:79-82.10.1016/j.jpba.2014.06.01625086492 [Google Scholar] [CrossRef] [PubMed]
[23]. Kountana E, Tziomalos K, Semertzidis P, Dogrammatzi F, Slavakis A, Douma S, Comparison of the diagnostic accuracy of ischemia-modified albumin and echocardiography in patients with acute chest painExp Clin Cardio 2013 18(2):98-100. [Google Scholar]
[24]. Sinha MK, Roy D, Gaze DC, Collinson PO, Kaski JC, Role of “Ischemia modified albumin”, a new biochemical marker of myocardial ischaemia, in the early diagnosis of acute coronary syndromesEmergency Medicine Journal 2004 21(1):29-34.10.1136/emj.2003.00600714734370 [Google Scholar] [CrossRef] [PubMed]
[25]. Bhagavan NV, Lai EM, Rios PA, Yang J, Ortega-Lopez AM, Shinoda H, Evaluation of human serum albumin cobalt binding assay for the assessment of myocardial ischemia and myocardial infarctionClin Chem 2003 49(4):581-85.10.1373/49.4.58112651810 [Google Scholar] [CrossRef] [PubMed]
[26]. Toklu O, Akgol E, Yesil M, Ustuner F, Abusoglu S, Predictive value of ischemia modified albumin in determining the severity of coronary artery diseaseJ Ann Eu Med 2017 5(1):22-26.10.4328/AEMED.100 [Google Scholar] [CrossRef]
[27]. Chek J, Dusek J, Stasek J, Vojacek J, Bis J, Ulrychova M, Role of ischemia-modified albumin in estimating the extent and scope of cardiac ischemia in patients with ST elevation myocardial infarctionHeart and Vessels 2011 26(6):622-27.10.1007/s00380-010-0114-021267579 [Google Scholar] [CrossRef] [PubMed]
[28]. Bonorino NF, Lunardelli A, Oliveira JR, Use of ischemia modified albumin for the diagnosis of myocardial infarctionJornal Brasileiro de Patologia e Medicina Laboratorial 2015 51(6):383-88.10.5935/1676-2444.20150060 [Google Scholar] [CrossRef]
[29]. Mehta MD, Marwah SA, Ghosh S, Shah HN, Trivedi AP, Haridas N, A synergistic role of ischemia modified albumin and high-sensitivity troponin T in the early diagnosis of acute coronary syndromeJournal of Family Medicine and Primary Care 2015 4(4):570-75.10.4103/2249-4863.17429526985418 [Google Scholar] [CrossRef] [PubMed]
[30]. Kumar PA, Subramanian K, The role of ischemia modified albumin as a biomarker in patients with chronic liver diseaseJ Clin Diagn Res 2016 10(3):BC09-BC12.10.7860/JCDR/2016/17168.739927134856 [Google Scholar] [CrossRef] [PubMed]
[31]. Chawla R, Loomba R, Guru D, Loomba V, Ischemia Modified Albumin (IMA)-a marker of glycaemic control and vascular complications in type 2 diabetes mellitusJ Clin Diagn Res 2016 10(3):BC13-BC16.10.7860/JCDR/2016/15282.743227134857 [Google Scholar] [CrossRef] [PubMed]
[32]. Bahinipati J, Mohapatra PC, Ischemia modified albumin as a marker of oxidative stress in normal pregnancyJ Clin Diagn Res 2016 10(9):BC15-BC17.10.7860/JCDR/2016/21609.845427790423 [Google Scholar] [CrossRef] [PubMed]
[33]. Reddy VS, Bukke S, Mahato K, Kumar V, Reddy NV, Munikumar M, Vodelu B, A meta-analysis of the association of serum ischaemia-modified albumin levels with human hypothyroidism and hyperthyroidismBioscience Reports 2017 37(1):BSR2016026810.1042/BSR2016026827920278 [Google Scholar] [CrossRef] [PubMed]