Culprit or Companion-Foetal Right Ventricular Diverticulum: Role of M-mode Echocardiography in Distinguishing it from Ventricular Aneurysm
Ashwal Adamane Jayaram1, Krishnanand Nayak2, Abdul Razak3, R Padmakumar4, Umesh Pai5
1 Associate Professor, Department of Cardiology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
2 Assistant Professor, Department of Cardiovascular Technology, School of Allied Health Science (SOAHS), Manipal Academy of Higher Education, Manipal, Karnataka, India.
3 Assistant Professor, Department of Cardiology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
4 Professor, Department of Cardiology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
5 Assistant Professor, Department of Cardiovascular Technology, School of Allied Health Science (SOAHS), Manipal Academy of Higher Education, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ashwal Adamane Jayaram, Associate Professor, Department of Cardiology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal-576104, Karnataka, India.
E-mail: dr.ashwal@gmail.com
Congenital ventricular diverticula and aneurysms are very rare. Prenatal diagnosis of such cases is reported only by few authors. Differentiating these two entities by echocardiography alone is very difficult. We present a case of prenatally diagnosed right ventricular diverticulum at 33 weeks of gestation. She was 37-year-old and primigravida with no past medical history. She underwent a routine prenatal scanning and was suspected to have a foetal cardiac abnormality and referred to us. It was diagnosed as foetal right ventricular diverticulum with the help of Motion-mode (M-mode) echocardiogram and was advised follow up after delivery. One of the differential diagnosis is ventricular aneurysm. Unfortunately, she had a miscarriage at 36 weeks due to unknown cause.
Congenital ventricular diverticula, M-mode echocardiogram, Prenatal foetal echocardiogram
Case Report
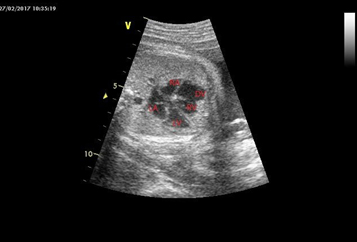
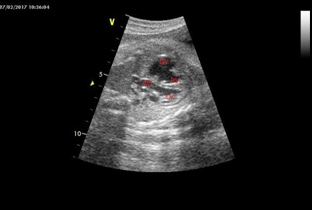
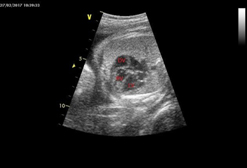
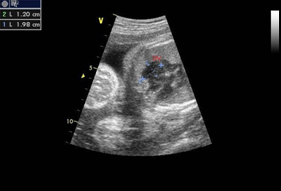
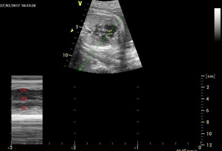
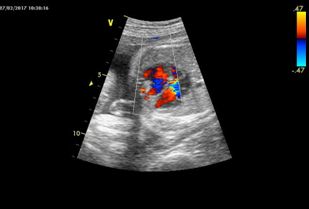
We present a 37-year-old, primigravida with unremarkable medical and family histories. An abnormal foetal heart chamber was identified in the 32nd weeks of pregnancy when the patient underwent a routine prenatal ultrasound at a local hospital by a radiologist. She was referred to our hospital in the 33rd weeks of pregnancy. Four chambers foetal echocardiogram revealed a Right Ventricular (RV) abnormal chamber [Table/Fig-1,3] of size measuring 1.2 cm × 1.98 cm communicating freely with RV [Table/Fig-4]. The four chamber view showed normal contractility of the diverticulum synchronous with rest of the myocardium by M-mode assessment [Table/Fig-5] and [Video-1]. Even though the connection to the ventricle was broad, colour Doppler echocardiogram detected blood flow into and out of the abnormal heart chamber [Table/Fig-6] and [Video-2]. The heart was otherwise normal. However, she had a miscarriage at 36 weeks due to unknown cause. There was no evidence of pericardial effusion, congenital heart disease, dysrhythmia, or extra cardiac anomalies. Thus, the diagnosis of right ventricular diverticula was made.
4 chamber view of the foetal heart showing right atrium (RA), right ventricle (RV), left atrium (LA), left ventricle (LV) and the diverticulum (DV) with a wide mouth connecting it with the right ventricle.
3 chamber view of the foetal heart showing right ventricle (RV), left ventricle (LV), aorta (AO) and the diverticulum (DV) with a wide neck connecting it with the right ventricle.
4 chamber view of the foetal heart showing right ventricle (RV), left ventricle (LV) and the diverticulum (DV).
Foetal echocardiogram showing a right ventricular diverticulum (DV) of approximately size 1.2 ×1.98 cm connected with the right ventricle (RV).
M mode of the foetal heart showing synchronous contraction of the diverticulum (DV), right ventricle (RV) and left ventricle (LV).
Colour Doppler ultrasound showing blood flow in and out of the abnormal heart chamber.
Discussion
Ventricular diverticula are very rare. Since 1940s, less than 200 cases of ventricular aneurysms or diverticula have been reported in the literature and only 20 of these are involving the right ventricle [1]. Pathogenesis of congenital cardiac diverticula and aneurysms is poorly understood. The focal weakening of the ventricular wall because of an interruption during embryogenesis or infection/localised ischaemia of the ventricular wall is proposed as mechanisms responsible for the development of diverticula and aneurysm [2]. In this report, we present a case of a right ventricular diverticulum diagnosed prenatally by M-mode ultrasonography and colour Doppler echocardiography.
Cardiac diverticula are localised outpouchings from the free ventricular wall. The prognosis is good in isolated cases. Complications include rupture, arrhythmia, thrombus formation, heart failure, and rarely infective endocarditis. The 10 years survival rate of patients with ventricular diverticula is around 80% year and the four years survival rate is around 30% [3].
When an abnormal heart chamber is continuous with the ventricle, differential diagnoses are an aneurysm and diverticula. Peters C et al., [4] proposed that diverticula wall is thick and aneurysm wall is thin. McAuliffe FM et al., [5] and Koshiishi T et al., [6]. distinguished aneurysm and diverticula by the size of the orifice connecting the ventricles. Diverticula appear saccular with a narrow base and aneurysms have a broad base. Cavalle-Garrido T et al., [7] and Del RM et al., [8] added the abnormal heart chamber contractibility to the above criteria. Ventricular diverticula have normal contraction synchronous with the ventricle as they are composed of all the three cardiac layers, and ventricular aneurysms are akinetic or dyskinetic with paradoxical contraction. Katsura D et al., [9] proposed colour Doppler ultrasound can detect blood flow from the diverticulum to the heart ventricle for diastole of the heart and from the heart to the diverticulum for systole.
M-mode imaging shows the movement and change of a point over time as the ultrasound beam’s brightness varies on the same line continuously. Thus, it helps fully in diagnosis as ventricular diverticulum has normal contraction and the ventricular aneurysm is akinetic or dyskinetic. As in our case, Katsura D et al., [9] also diagnosed abnormal heart chamber prenatally as a ventricular diverticulum by showing normal contraction on M-mode ultrasound and later by postnatal computed tomography. Demir F et al., [10] and Martinez Olorón P et al., [11] also believe M-mode ultrasound helps in distinguishing between a ventricular aneurysm and diverticulum. However, Ohlow MA et al., [12] reported that 10% of ventricular diverticula were akinetic and 8% of ventricular aneurysms had normal contractility and other criteria’s like the thickness of the wall, size of the orifice and blood flow on colour Doppler should be used in the diagnosis.
Importantly, right ventricular diverticula are usually not associated with abnormalities like aneuploidy, extra cardiac malformations, or foetal growth restriction. We suggest that foetuses with suspected right ventricular diverticula should undergo serial sonography and echocardiography. Vaginal delivery at term is usually preferred. After delivery, echocardiography is recommended to confirm the diverticulum and rule out other additional cardiac defects. As long as the diverticulum is small, isolated, and asymptomatic, conservative management is expected.
Conclusion
The congenital foetal diverticula are very rare in clinical practice and the ventricular aneurysm is a differential diagnosis. This case shows the importance of diagnosing ventricular diverticula correctly when an abnormal dilatation of the foetal ventricle is identified during routine prenatal ultrasound screening. Usually, the diverticula are benign but sometimes may be fatal, may cause sudden death due to rupture, arrhythmia, thrombus formation, heart failure, and rarely by infective endocarditis. It is difficult to accurately diagnose diverticula in the prenatal ultrasound and postnatal follow up with 2D Echo and cardiac MRI/CT is often required.
Supplementry Material
Supplementary video 1:
4 chamber view of the fetal heart showing right atrium (RA), right ventricle (RV), left atrium (LA), left ventricle (LV) and the diverticulum (DV) with a wide mouth connecting it with the right ventricle
Supplementary video 2:
Colour Doppler ultrasound showing blood flow in and out of the abnormal heart chamber.
[1]. Di Sessa TG, Howard SC, Salim MA, Congenital right ventricular diverticulum associated with a ventricular septal defect: a rare echocardiographic findingEchocardiography 2006 23(9):787-89.10.1111/j.1540-8175.2006.00312.x16999700 [Google Scholar] [CrossRef] [PubMed]
[2]. Caldaroni F, Rose D, Caiaro A, Casciani E, Martucci V, Manganaro L, Fetal right ventricular diverticulum with pericardial effusion: to drain or not to drain?J Pediatr Neonatal Care 2014 1(3):01-03.10.15406/jpnc.2014.01.00016 [Google Scholar] [CrossRef]
[3]. Marijon E, Ou P, Fermont L, Concordet S, Le Bidois J, Sidi D, Diagnosis and outcome in congenital ventricular diverticulum and aneurysmJ Thorac Cardiovasc Surg 2006 131(2):433-37.10.1016/j.jtcvs.2005.09.04616434275 [Google Scholar] [CrossRef] [PubMed]
[4]. Peters C, Wacker-Gussmann A, Strasburger J, Cuneo B, Gotteiner N, Gulecyuz M, Electrophysiologic features of fetal ventricular aneurysms and diverticulaPrenat Diagn 2014 35(2):129-36.10.1002/pd.450125284224 [Google Scholar] [CrossRef] [PubMed]
[5]. McAuliffe FM, Hornberger LK, Johnson J, Chitayat D, Ryan G, Cardiac diverticulum with pericardial effusion: report of two new cases treated by in-utero pericardiocentesis and a review of the literatureUltrasound in Obste and Gynecol 2005 25(4):401-04.10.1002/uog.185615747327 [Google Scholar] [CrossRef] [PubMed]
[6]. Koshiishi T, Osada H, Hata A, Furugen Y, Murakoshi T, Mitsuhashi N, Prenatal rupture of right ventricular diverticulum: a case report and review of the literaturePrenat Diagn 2007 27(12):1154-57.10.1002/pd.183317787028 [Google Scholar] [CrossRef] [PubMed]
[7]. Cavallé-Garrido T, Cloutier A, Harder JF, Boutin C, Smallhorn J, Evolution of fetal ventricular aneurysms and diverticula of the heart: an echocardiographic studyAm J Perinatol 1997 14(07):393-400.10.1055/s-2007-9941679263558 [Google Scholar] [CrossRef] [PubMed]
[8]. Del RM, Martínez JM, Bennasar M, Palacio M, Figueras F, Puerto B, Prenatal diagnosis of a right ventricular diverticulum complicated by pericardial effusion in the first trimesterUltrasound in Obstetrics and Gynecology 2005 25(4):409-11.10.1002/uog.187015789414 [Google Scholar] [CrossRef] [PubMed]
[9]. Katsura D, Hayashi K, Tsuji S, Ono T, Ishiko A, Takahashi K, Fetal right ventricular diverticulum detected by prenatal ultrasound screeningCase Reports in Obstetrics and Gynecology 2016 2016:01-04.10.1155/2016/638292027818814 [Google Scholar] [CrossRef] [PubMed]
[10]. Demir F, Ozbarlas N, Gocen U, Buyukkurt S, Prenatal diagnosis of giant left ventricular diverticulum: case reportEchocardiography 2014 32(2):395-97.10.1111/echo.1278125286772 [Google Scholar] [CrossRef] [PubMed]
[11]. Martínez Olorón P, Romero Ibarra C, Galdeano Miranda JM, Right ventricular outpouching associated with a ventricular septal defect: case reportPediatric Cardiology 2011 32(8):1269-70.10.1007/s00246-011-0059-921947405 [Google Scholar] [CrossRef] [PubMed]
[12]. Ohlow MA, Brunelli M, Lauer B, Characteristics, and outcome of primary congenital left ventricular aneurysm and diverticulum: analysis of cases from the literaturePrenatal Diagnosis 2014 34(9):893-99.10.1002/pd.438924752829 [Google Scholar] [CrossRef] [PubMed]